Abstract
Several exogenous or endogenous factors can lead to inflammatory heart disease. Beside infectious myocarditis, other systemic inflammatory disorders such as sarcoidosis, systemic lupus erythematosus (SLE), systemic sclerosis (SSc), Churg-Strauss syndrome, and rheumatoid arthritis can affect the myocardium. Myocardial inflammation may have a major impact on the outcome of these patients, resulting in sudden cardiac death, severe arrhythmias, or end-stage heart failure. The current gold standard for definite confirmation of inflammatory heart disease is endomyocardial biopsy (EMB), but is invasive and suffers low sensitivity and specificity due to sampling errors. Thus, non-invasive methods for detecting the extent and changes over time of the inflammatory myocardial disease are needed. Cardiac magnetic resonance (CMR) is such a non-invasive method. We will describe and discuss different approaches for CMR assessment of inflammatory myocardial disease including early gadolinium enhancement (EGE), T2-weighted imaging, late gadolinium enhancement (LGE), the newer mapping proton relaxation techniques (T1 pre-contrast, T1 post-contrast, T2 mapping), and the hybrid PET/MRI technique.
Similar content being viewed by others
Introduction
Several exogenous or endogenous factors can lead to acute or chronic inflammatory heart disease. Beside infectious myocarditis, which is mostly viral in origin, other systemic inflammatory disorders such as sarcoidosis, systemic lupus erythematosus (SLE), systemic sclerosis (SSc), Churg-Strauss syndrome, and rheumatoid arthritis can affect the myocardium.
Myocardial inflammation may have major impact on the outcome of these patients, resulting in sudden cardiac death, severe arrhythmias, or end-stage heart failure [1••]. Currently, a definite diagnosis of inflammatory heart disease requires endomyocardial biopsy (EMB) [2], which is the only procedure that can directly assess the extent of myocardial inflammation and clarify the underlying pathophysiology and its triggers, potentially yielding to adequate treatment of these patients. However, it is invasive and suffers from several limitations including low sensitivity and specificity due to sampling errors. Thus, new non-invasive methods for detecting and following inflammatory myocardial disease are needed in addition to biopsy.
Cardiac magnetic resonance (CMR) is such a new non-invasive method, which has high spatial resolution, allows evaluation of morphology, function, and tissue characterization as a one stop shop, and works without any radiation. In this manuscript, we will describe and discuss different approaches for CMR assessment of inflammatory myocardial disease (see Table 1) including early gadolinium enhancement (EGE), T2-weighted imaging, late gadolinium enhancement (LGE), the newer mapping proton relaxation techniques (T1 pre-contrast, T1 post-contrast, T2 mapping), and the hybrid novel PET/MRI technique.
CMR Techniques
Early Gadolinium Enhancement (EGE)
Acute inflammation leads to hyperemia, and some reports describe an increased early uptake of gadolinium in these areas [3]. Thus, after contrast application, signal intensity is elevated in the first few minutes compared to skeletal muscle, which can be quantified on spin echo images. However, the exact mechanism of EGE is less clear and non-specific, and image quality can be significantly affected by motion artifacts due to irregular heart rhythms and breathing patterns. Hence, EGE alone is usually insufficient for the diagnosis of myocardial inflammation. It is most informative when positive on good-quality images in combination with other tissue characterization techniques, and while it can be used clinically, many centers tend to reserve EGE as a research tool.
T2-Weighted Images
T2 is the time of transverse magnetization decay, which is prolonged in edematous, inflammatory myocardial tissue, appearing bright on T2-weighted images. Similar to EGE and using T2 dark-blood sequences, myocardial signal is indexed to skeletal muscle signal intensity. The underlying assumption to this approach is, that skeletal muscle is not influenced by inflammation, which seems quite problematic in acute viral or systemic inflammatory diseases.
On dark-blood T2-weighted imaging, the diagnosis of global myocardial edema is made when the ratio is >1.9 [4]. Unfortunately, image quality of this method depends heavily on a regular, normofrequent rhythm, and patient ability to breath-hold during the image acquisition. Furthermore, this method is prone to bright signal artifacts adjacent to the subendocardium due to poor dark-blood preparation of slow-flow blood within the LV cavity. Newer bright-blood T2-weighted sequences overcome some of these limitations, but were not shown to be superior to dark-blood T2-weighted imaging in the evaluation of global myocardial edema and myocarditis [5•, 6••].
Late Gadolinium Enhancement
LGE images are acquired late (15–25 min) after application of gadolinium. At that time, contrast is washed out in normal myocardium (which is nulled), but in regions with enlarged extracellular/interstitial space due to acute necrosis, chronic scar, or fibrotic tissue, the contrast agent exhibit delayed washout, appearing hyperintense on the images [7]. Hence, in comparison to EGE and T2-weighted imaging, LGE typically reveals areas of irreversible damage, such as acute necrosis and chronic fibrosis. It has its strengths in detecting focal processes, whereas in diffuse processes this technique has its limitations. Nevertheless, LGE is the most frequently used and best established method for myocardial tissue characterization, useful not only in diagnosing non-ischemic cardiac diseases, but also in prognostication [1••, 8•, 9•]. Furthermore, in comparison to EGE and T2-weighted imaging, LGE is best validated against histological evidence of myocarditis [10, 11].
“Two Out of Three Is Better than One?”
There is an ongoing debate about the best diagnostic approach to inflammatory heart disease using different CMR sequences. In 2009, some experts formulated an approach to detect myocardial inflammation using EGE, T2-weighted, and LGE imaging. Based on collective evidence available at that time, albeit small number studies, the diagnostic accuracy of acute myocarditis may be improved when two out of the three imaging techniques were positive, also known as the “Lake Louise criteria” [12]. This is sensible in principle, as increasing the number of measurements may increase the diagnostic yield for detecting disease, although EGE and T2-weighted techniques often require longer acquisition times and image quality prone to motion artifacts, making these challenging to apply especially in acutely ill patients who have tachyarrhythmia and difficulty breath-holding.
T1 Mapping Pre-/post-contrast
Recently developed pre-contrast T1 quantitative mapping techniques represent a fundamental step forward in the non-invasive assessment of myocardial inflammation [13]. Despite saturation recovery and inversion recovery based T1 mapping techniques being developed since the 1980s [14, 15], important challenges impeded their clinical application [16]. It is only since a more robust and reproducible mapping sequence (e.g., the modified Look-Locker inversion recovery (MOLLI) sequence) [17] has become available that wider clinical applications have become possible. Technical advances allowing for shorter acquisitions and shorter breath-holds (such as the ShMOLLI technique) facilitate the implementation in acutely ill patients [18, 19•, 20].
Post-contrast T1 mapping techniques are also available; these are currently being used to assess for expansion of interstitial space/fibrosis (extracellular volume, ECV) and distinguish it from replacement fibrosis (such as scarred myocardium) [21, 22]. Using an extravascular gadolinium contrast medium, once an equilibrium distribution between blood and tissue is attained, the partition coefficient of the contrast can be derived using pre- and post-contrast T1 values of the blood and myocardium. Further methods such as equilibrium contrast CMR (EQ-CMR) [23] and dynamic equilibrium CMR [24] adjust for the hematocrit to derive the ECV.
The diagnostic accuracy of T1 mapping techniques can be hampered by motion artifacts due to inconsistent breath-holding or patient movements. To overcome these limitations, technical developments allowing for motion correction and co-registration are now available [25].
T2 Mapping
Spin echo-based T2 mapping techniques are known to be prone to effects of cardiac motion and stimulated echoes [26]. T2 mapping techniques using T2-prepared steady-state free precession (T2p-SSFP) were initially developed for BOLD imaging [27]. Using a similar mapping scheme, Giri et al. [28], validated the technique and demonstrated its increased accuracy in detecting T2 variations across the myocardium compared not only to standard T2-weighted techniques but also to spin echo-based T2 mapping techniques. Further developments aiming specifically to address misregistration of the parametric maps are available using navigator gating and map registration, enabling a more robust-free breathing T2 mapping technique [29].
T1/T2 Mapping in Myocardial Inflammation/Edema
Myocardial inflammation and edema are characterized by an increase in free water content, which prolongs both T2 and T1 relaxation times. Myocardial T1 and T2 mapping have been validated against microspheres to detect myocardial edema in experimental animal models [30••] and also in human clinical populations with superior diagnostic performance to conventional T2-weighted techniques [5•, 31]. Quantitative T1 and T2 mapping techniques are well suited to detect myocardial inflammation and edema, which are common final pathways of myocardial injury in a number of myocardial conditions, with potentially high sensitivity and ability to locate small areas of abnormality.
PET/MRI
PET/MRI combines the strengths of both techniques. PET is a non-invasive imaging technique, which can detect metabolic active processes with high sensitivity: 18F-FDG PET cumulates in inflammatory regions due to the glycolytic activity of cells, which participate in inflammatory processes (neutrophils, monocytes/macrophages). Disadvantages of PET are radiation exposure and reduced spatial resolution, so small areas of inflammation might be missed. Hence, a combination with MRI (providing high spatial resolution and lack of radiation exposure) seems reasonable [32].
Clinics
Myocarditis
Viral myocarditis is the most common inflammatory heart disorder. Symptoms and clinical presentation may vary, making the diagnosis a challenge. Furthermore, the clinical course comprises a wide spectrum ranging from complete recovery to terminal heart disease or sudden cardiac death. Autopsy studies revealed that myocarditis is responsible for 5 to 20 % of sudden deaths in young adults [33], so getting the diagnosis right is of vital importance in this population.
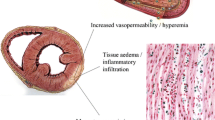
CMR and its unique ability of non-invasive tissue characterization are extremely helpful in the work-up of suspected myocarditis. There are three stages of myocardial alterations in these patients: firstly, myocardial damage due to the trigger; secondly, myocardial inflammation by the host immune system; and thirdly, chronic myocardial inflammation, which may result in myocardial fibrosis, leading to remodeling, consequent ventricular dysfunction [34] and arrhythmic substrates.
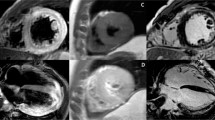
These alterations lead to acute myocardial necrosis and/or chronic scarring/fibrosis reflected by subepicardial or intramural regions of LGE, often patchy, and preferentially located in the posterolateral wall [10], see Fig. 1.
CMR of a 28-year-old male presenting with dyspnea and chest pain 5 days after flu-like symptoms. Due to ST elevation and elevated cardiac enzymes, the patient underwent coronary angiography where coronary stenosis could be excluded. Cine images reveal global preserved left ventricular ejection fraction (LVEF = 60 %) with discrete hypokinesia at the lateral wall. LGE is present in multiple locations (white arrows), suggestive of myocarditis. The acute nature of the disease is demonstrated by positive dark-blood T2W images displaying a clear bright signal in the lateral wall, in an area consistent with LGE findings. Note that on the correspondent T2-weighted images in the long-axis, these lesions are not well delineated. This patient received state of the art heart failure medication (betablocker, ARB); in the next few months, the initial extensive LGE lesions decreased in size (which could be observed at a subsequent CMR scan) and the patients complaints resolved completely
In the setting of viral myocarditis, CMR studies with LGE are being performed for more than 10 years, first looking at the diagnostic performance of the technique, followed by prognostic data. To date, there is clear evidence that positive LGE is associated with an adverse outcome: patients with LGE are at increased risk of suffering adverse cardiac events. Grün et al. demonstrated in more than 220 patients with biopsy-proven viral myocarditis that the presence of LGE is the best independent predictor of all-cause mortality and of cardiac mortality [1••]. Furthermore, patients with no LGE have an excellent prognosis. This was confirmed by Schumm and Greulich et al. in a large study with more than 400 patients with suspected myocarditis (“all comers”): patients who had a CMR scan without pathological findings (normal left ventricular ejection fraction, normal left ventricular enddiastolic volume, no LGE) had a good prognosis, independent of their clinical symptoms and other findings [9•]. Nevertheless, we have to keep in mind that not all LGE-positive patients will suffer an event, but they are at an increased risk to do so.
Despite the limitations of EGE and T2-weighted imaging, these techniques may be useful in supporting the acute nature of the inflammatory process when images are diagnostic. Friedrich et al. recently published data on 35 patients with suspected acute myocarditis, in whom the overall diagnostic accuracy of “T2 and/or LGE” was significantly better than LGE alone. For patients in whom a high positive likelihood ratio is needed, the full Lake Louise criteria may be useful [35]. However, as described above, these techniques can be challenging to apply in the practical clinical setting, and novel quantitative mapping techniques may circumvent many of the recognized technical and methodological limitations.
T1 Mapping and ECV
Recently, mapping techniques have been shown to have great utility in this disease owing to its sensitivity to detecting myocardial water and pixel-wise quantification. Ferreira and Piechnik et al. [6••] first demonstrated that native T1 mapping using the ShMOLLI technique [18, 36••] is a superior diagnostic technique (ROC area-under-the-curve 0.95) compared to conventional T2-weighted imaging, with an equivalent performance to LGE. Not only can native T1 mapping be used as a novel diagnostic criterion like the Lake Louise criteria, with superior sensitivity to T2-weighted and LGE imaging, but native T1 maps can also display the typical non-ischemic patterns in acute myocarditis without the need for gadolinium contrast agents [37]. In addition, T1 mapping offers a significant incremental diagnostic value, detecting additional areas of myocardial involvement beyond T2-weighted and LGE imaging and identified extra (30 %) cases when at least one of these conventional methods failed to identify abnormalities [37].
Compared to the diagnostic performance of some of the Lake Louise criteria, native T1 mapping, as a method for imaging edema, may replace dark-blood T2-weighted imaging either as a single criterion or in combination with LGE. ShMOLLI T1 mapping offers a number of advantages to conventional dark-blood T2-weighted imaging such as for cases in which tachyarrhythmia, patient inability to perform long breath-hold or skeletal muscle inflammation lead to non-diagnostic or false-negative images. The added ability of T1 mapping to demonstrate non-ischemic patterns of myocardial injury using incremental thresholds means that T1 mapping can effectively act as a method for both edema and LGE pattern imaging. In the future, it may be possible to perform a gadolinium-free CMR protocol using cine and T1 mapping, with T1 mapping as a single criterion demonstrating around 90 % in sensitivity, specificity, accuracy, PPV, and NPV [37].
Luetkens et al. [38] compared the diagnostic performance of the Lake Louise criteria, native T1 relaxation times and ECV at 3 Tesla and found that native T1 mapping significantly outperformed the other techniques tested (ROC area under the curve 0.94), with a high diagnostic performance (sensitivity 92 %, specificity 91 %, diagnostic accuracy 91 %), consistent with the results by Ferreira et al. [6••, 37]. The specificity of T1 mapping was significantly higher with native T1 mapping than that of the combined Lake Louise criteria (sensitivity, 92 %; specificity, 80 %; diagnostic accuracy, 85 %).
ECV quantification has utility in acute to subacute, severe myocarditis, as shown by Radunski et al. [39], who assessed the diagnostic performance of T2, T1, and extracellular volume (ECV) quantification as novel quantitative tissue markers compared to the Lake Louise criteria. ECV quantification with LGE imaging significantly improved the diagnostic accuracy of CMR compared with the Lake Louise criteria, in patients being evaluated 1–7 weeks after the index presentation.
T2 Mapping
T2 mapping techniques have been shown to allow detection of myocardial edema beyond standard techniques such as wall motion abnormalities, T2-weighted, or LGE in a variety of cardiac pathologies including myocarditis. As shown by Thavendiranathan et al. [31], T2 mapping has a sensitivity and specificity of 94 and 97 %, respectively, in detecting acute inflammatory diseases such as myocarditis and Takotsubo cardiomyopathy. T2 mapping had also shown some utility in detecting severe myocarditis up to 7 weeks after presentation [39].
Overall, while quantitative mapping techniques hold promise to diagnose myocarditis, establishing which method has the best diagnostic accuracy is still challenging and requires further evidence, such as larger studies and multicenter trials.
Sarcoid Myocarditis
Sarcoidosis is a systemic granulomatous inflammatory disease with unknown etiology that can affect the heart additionally, or isolated. In case of cardiac involvement, typical manifestations include arrhythmias, heart failure and/or sudden cardiac death, which is a frequent cause of death in these patients. Prevalence of cardiac involvement ranges from 20 to 30 % [40], depending on the patient population. As described above, the gold standard endomyocardial biopsy has a low sensitivity, underlining the need of alternative (non-invasive) tools for diagnosis and management. In line with the results of Patel et al. [41], Greulich et al. could clearly demonstrate in a cohort of 155 patients with suspected cardiac sarcoidosis that the presence of LGE is correlated with major adverse advents such as ventricular tachycardia and sudden cardiac death [8•]. Thus, CMR screening for cardiac involvement in patients with sarcoidosis is now available in the clinical routine. Figure 2 illustrates a typical patient example, in which CMR revealed cardiac involvement of sarcoid disease.
A 61-year-old female presenting with chest pain and elevated cardiac enzymes. Coronary artery disease (CAD) was ruled out by coronary angiography. a Cine images showed a slightly diminished left ventricular ejection fraction (LVEF = 53 %). b LGE images revealed an almost transmural LGE inferoseptal from midventricular to the apex, from epicardial origin. This pattern could indicate cardiac manifestation of a systemic disease such as sarcoid. c T2-weighted images demonstrate hyperintense regions (edema) in the inferoseptal wall (white arrows), corresponding to LGE. Biopsies were taken, which confirmed the diagnosis of sarcoidosis, and steroid therapy was initiated
PET/MRI is a promising approach in patients with known or suspected cardiac sarcoidosis to detect inflammation with high sensitivity (active cardiac sarcoidosis), as well as fibrosis by LGE (chronic cardiac sarcoidosis), which may have implications for diagnosis and clinical follow-up [42, 43]. First results are convincing (see Fig. 3), but prospective studies are needed. In addition, PET imaging is expensive and not widely available, yet. Furthermore, preparation for PET (12–18-h fasting to suppress physiologic glucose metabolism by the heart) and radiation exposure have to be considered in these (often young) patients. On the other hand, due to the wide implication of possible cardiac involvement, detailed diagnostic testing may be warranted.
A 72-year-old woman was referred with increasing shortness of breath and intermittent chest pain. Echocardiography revealed a diminished left ventricular ejection fraction (35 %); significant CAD could be ruled out by coronary angiography. Biopsy of an enlarged scalene lymph node showed non-caseating granulomas, so cardiac sarcoid was considered, and a hybrid PET/MRI was scheduled. In the upper row T2-weighted images are displayed in cine short axis views. Middle row shows the concomitant LGE images; the presence of LGE is indicated by the white arrows. In the bottom row, there are fused images (MRI and PET): note that PET images show an increased uptake in the border zones of the LGE, suggesting that the process of inflammation affects more regions than displayed solely by LGE. Far right, CMR images showing splenic nodules with enhancement on both LGE sequences and by PET. Reprinted with permission from LWW [42]
Collagenosis: Systemic Lupus Erythematosus (SLE) and Systemic Sclerosis (SSc)
The group of collagenosis consists of a heterogenous group of systemic diseases affecting connective tissue and is characterized by necrosis or vasculitis.
Systemic Lupus Erythematosus
This disease affects predominantly females, with cardiac involvement reported in 60–70 % of the patients. These patients are exposed to an increased risk of coronary atherosclerosis, which may result in myocardial infarction. Beside of atherosclerosis, myocarditis and pericardial effusion could be observed, justifying the use of non-invasive imaging techniques. The prevalence of LGE in these patients ranges from low to high in the literature. This might be due to the fact that there is a wide spectrum of disease activity in these patients. Nevertheless, a study from Mavrogeni et al. [44], which compared 50 patients with suspected infective myocarditis and 25 active SLE patients to 20 controls revealed that LGE was positive only in the minority of SLE-active patients, underlining the need of additional CMR techniques, which can detect inflammatory processes.
T1 Mapping and ECV
Native T1 mapping and ECV quantification were able to detect subclinical myocardial involvement in patients with SLE who were asymptomatic and had normal LV indices [45•]. Compared to normal controls, both native myocardial T1 and extracellular volume fraction (26 ± 5 % vs. 30 ± 6 %) were significantly increased in patients with SLE, both of which also correlated with reduced longitudinal strain. Native myocardial T1 values showed the greatest concordance with the presence of clinical diagnosis of SLE compared to other CMR markers such as myocardial function, perfusion, and LGE. Thus, T1 mapping is able to demonstrate subclinical myocardial involvement in systemic diseases otherwise not apparent on conventional cardiac diagnostic tests.
Systemic Sclerosis
In contrast to SLE, the role of SSc in the pathogenesis of coronary atherosclerosis is not as well defined: data range from elevated risk to risk equal to the general population. There is consensus about potential cardiac involvement, which can manifest as myocardial damage, disturbances of the conduction system, pericardial disease, or alterations of the valves. Aside from that, secondary cardiac complications may occur due to extracardiac manifestations of SSc: e.g., secondary pulmonary hypertension due to sclerotic pulmonary alterations.
A recent study [46] revealed that myocarditis is a common finding in SSc patients with recent-onset cardiac involvement, presenting with new onset of clinical symptoms (heart failure, chest pain, palpitations) and elevated cardiac enzymes: six out of seven patients showed LGE; all had evidence of acute or chronic myocarditis by histology. Only in two out of these six LGE positive patients, T2 hyperintensity (edema) was present. Despite the initiation of immunosuppressive treatment, two out of seven patients suffered SCD. This study underscores, that, if cardiac involvement is present, LGE may be a good prognosticator, and these patients may require a closer observation or maybe even a more aggressive treatment to decrease the likelihood of adverse cardiovascular events, although larger studies are needed. The combination of repeated ischemia/vasoconstriction and inflammation may result in diffuse interstitial fibrosis, which was reported in endomyocardial biopsies of SSc patients [47•].
T1 Mapping and ECV
Three groups of investigators have been able to detect early subclinical myocardial involvement in systemic sclerosis using T1 mapping and ECV quantification when there is no apparent cardiac disease. Ntusi et al. [48] found that in patients with SSc without overt cardiovascular disease, native T1 values were significantly elevated, detecting large areas of myocardial abnormality (median 52 vs. 3 % in controls) and expansion of ECV (35.4 ± 4.8 vs. 27.6 ± 2.5 %), likely resulting from a combination of low-grade inflammation and diffuse myocardial fibrosis (see Fig. 4). Native T1 and ECV were correlated with disease activity and severity, and ECV inversely correlated with subclinical myocardial dysfunction as reflected in impairment in the peak systolic circumferential strain and peak diastolic strain rate despite normal biventricular size and systolic function. Thuny et al. [49] reported similar findings in patients with SSc, normal LV systolic function, and no LGE, who had significantly increased ECV (median 30.0 vs. 26.8 % in controls), which correlated with left atrial volume and diastolic dysfunction. Barison et al. [50] also demonstrated ECV expansion in asymptomatic SSc patients with normal LV systolic function and without LGE, both in the myocardium (30 ± 4 % vs. 28 ± 4 % in controls) and in skeletal muscle (23 ± 6 % vs. 18 ± 4 %). T1 mapping and ECV quantification can detect subclinical myocardial disease in this condition and may identify patients with early myocardial involvement, with potential to treat early before permanent irreversible injury occurs.
Cardiac magnetic resonance images from a 48-year-old patient with systemic sclerosis (SSc), with a normal left ventricular (LV) ejection fraction of 63 %. a LGE imaging with no focal areas of enhancement. b T2 map. c Native T1 map (acquired using ShMOLLI at 1.5 T) showed significantly elevated average LV myocardial T1 values of 1009 ± 47 ms (normal 962 ± 25 ms). d Post-contrast T1 map acquired at 15 min after gadolinium administration. Average post-contrast T1 values were 479 ± 18 ms. Extracellular volume (ECV) quantification using pre- and post-contrast T1 mapping and adjusting for the hematocrit demonstrated a significant expansion of interstitial space at 40 % (normal 27 ± 3 %). Images courtesy Dr. Ntobeko Ntusi, University of Oxford
Churg-Strauss Syndrome
The vasculitides encompass a wide spectrum of diseases with different entities. Aside from large-vessel vasculitis (e.g., Takayasu, Kawasaki), vasculitis of the small vessels (EGPA = eosinophilic granulomatosis with polyangiitis, also known as Churg-Strauss syndrome) has gained attention, showing some impressive cardiac manifestation leading to impaired left ventricular function. Interestingly, LGE images show a subendocardial and also intramural pattern, sometimes resembling ischemic heart disease, but typically not related to a coronary territory, representing destructed coronary capillaries due to the inflammation process. More recent advances in characterizing inflammation by mapping sequences seem promising, but there is no published data yet.
Rheumatoid Arthritis (RA)
Patients with rheumatoid arthritis (RA) suffer accelerated atherosclerosis. The prevalence of myocardial tissue involvement is very variable in the literature, due to different inclusion criteria and patient population.
Ntusi et al. [51] compared 39 RA patients (28 female, mean age 50 ± 12 years, diagnosed with RA for a median of 7 years, mean DAS28-CRP score 3.3 ± 1.3) to 39 matched controls, all without previously known cardiovascular disease using CMR at 1.5 T, including cine, T2-weighted, native T1 mapping, ECV quantification, and LGE imaging. RA patients had larger areas of focal myocardial edema on T2-weighted imaging (median 10 vs. 0 % LV involvement). Forty-six percent had LGE, of which 28 % showed a midwall pattern and 13 % patchy enhancement; two patients (5 %) revealed previously unknown myocardial infarction, subsequently confirmed to have a significant CAD on angiography. Overall, however, the LGE burden was small (3.7 ± 0.4 % of total LV mass).
T1 Mapping and ECV
Further, the utility of T1 mapping and ECV has been shown in patients with RA but no prior history of cardiovascular disease and normal LV indices [51]. Compared to normal controls, native T1 and ECV (30.3 ± 3.4 % vs. 27.9 ± 2.0 %) were significantly elevated in these patients, regardless of the presence of LGE, and both correlated with impaired peak systolic and diastolic strain and RA disease activity. In RA patients with apparently normal hearts, subclinical myocardial involvement can be detected using conventional and mapping CMR techniques, which show focal myocardial fibrosis, inflammation, and expansion of extracellular space, likely reflecting a degree of diffuse myocardial fibrosis in this systemic disease. T1 mapping and ECV quantification may provide incremental value as novel biomarkers for early disease detection, monitoring, and determining response to therapy in systemic inflammatory diseases.
Conclusion
In summary, CMR techniques are able to provide detailed information about myocardial inflammation. LGE is the most validated tool for diagnosis and prognosis, but has limitations in detecting acute inflammatory processes without scar or fibrosis. EGE and T2-weighted imaging may be useful in increasing the diagnostic accuracy of acute inflammatory myocardial processes in selected cases but can be challenging to apply in the practical clinical setting due to recognized technical and methodological limitations. Novel quantitative mapping techniques seem very promising, as they can detect edema as well as fibrosis while circumventing some of the challenges of conventional CMR techniques, allowing a more holistic approach to the different stages of inflammation. Prospective multicenter studies are warranted to clarify the future role of their clinical utility.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grun S, Schumm J, Greulich S, Wagner A, Schneider S, Bruder O, et al. Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. J Am Coll Cardiol. 2012;59(18):1604–15. doi:10.1016/j.jacc.2012.01.007. Prognostic role of LGE in patients with biopsy-proven viral myocarditis: Presence of LGE is the best independent predictor of all-cause mortality and of cardiac mortality.
Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636–48. doi:10.1093/eurheartj/eht210. 48a–48d.
Friedrich MG, Strohm O, Schulz-Menger J, Marciniak H, Luft FC, Dietz R. Contrast media-enhanced magnetic resonance imaging visualizes myocardial changes in the course of viral myocarditis. Circulation. 1998;97(18):1802–9.
Abdel-Aty H, Boye P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D, et al. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. 2005;45(11):1815–22. doi:10.1016/j.jacc.2004.11.069.
Ferreira VM, Piechnik SK, Dall’Armellina E, Karamitsos TD, Francis JM, Choudhury RP, et al. Non-contrast T1-mapping detects acute myocardial edema with high diagnostic accuracy: a comparison to T2-weighted cardiovascular magnetic resonance. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2012;14:42. doi:10.1186/1532-429X-14-42.
Ferreira VM, Piechnik SK, Dall’Armellina E, Karamitsos TD, Francis JM, Ntusi N, et al. T(1) mapping for the diagnosis of acute myocarditis using CMR: comparison to T2-weighted and late gadolinium enhanced imaging. J Am Coll Cardiol Img. 2013;6(10):1048–58. doi:10.1016/j.jcmg.2013.03.008. Native T1 mapping as a novel criterion for the detection of acute myocarditis showed excellent and superior diagnostic performance compared with T2W-CMR.
Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005;26(15):1461–74. doi:10.1093/eurheartj/ehi258.
Greulich S, Deluigi CC, Gloekler S, Wahl A, Zurn C, Kramer U, et al. CMR imaging predicts death and other adverse events in suspected cardiac sarcoidosis. J Am Coll Cardiol Img. 2013;6(4):501–11. doi:10.1016/j.jcmg.2012.10.021.
Schumm J, Greulich S, Wagner A, Grun S, Ong P, Bentz K, et al. Cardiovascular magnetic resonance risk stratification in patients with clinically suspected myocarditis. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2014;16(1):14. doi:10.1186/1532-429X-16-14. In clinically suspected myocarditis, patients with normal CMR have an excellent prognosis independent of their clinical symptoms and other findings.
Mahrholdt H, Goedecke C, Wagner A, Meinhardt G, Athanasiadis A, Vogelsberg H, et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation. 2004;109(10):1250–8. doi:10.1161/01.CIR.0000118493.13323.81.
Mahrholdt H, Wagner A, Deluigi CC, Kispert E, Hager S, Meinhardt G, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114(15):1581–90. doi:10.1161/CIRCULATIONAHA.105.606509.
Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, et al. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol. 2009;53(17):1475–87. doi:10.1016/j.jacc.2009.02.007.
Higgins DM, Moon JC. Review of T1 mapping methods: comparative effectiveness including reproducibility issues. Curr Cardiovasc Imaging Rep. 2014;7(9252). doi:10.1007/s12410-013-9252-y.
Pykett IL, Rosen BR, Buonanno FS, Brady TJ. Measurement of spin–lattice relaxation times in nuclear magnetic resonance imaging. Phys Med Biol. 1983;28(6):723–9.
Zhang Y, Yeung HN, O’Donnell M, Carson PL. Determination of sample time for T1 measurement. J Magn Reson Imaging JMRI. 1998;8(3):675–81.
Messroghli DR, Niendorf T, Schulz-Menger J, Dietz R, Friedrich MG. T1 mapping in patients with acute myocardial infarction. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2003;5(2):353–9.
Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med Off J Soc Magn Reson Med Soc Magn Reson Med. 2004;52(1):141–6. doi:10.1002/mrm.20110.
Piechnik SK, Ferreira VM, Dall’Armellina E, Cochlin LE, Greiser A, Neubauer S, et al. Shortened modified Look-Locker Inversion recovery (ShMOLLI) for clinical myocardial T1-mapping at 1.5 and 3 T within a 9 heartbeat breathhold. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2010;12:69. doi:10.1186/1532-429X-12-69.
Dall’Armellina E, Piechnik SK, Ferreira VM, Si QL, Robson MD, Francis JM, et al. Cardiovascular magnetic resonance by non contrast T1-mapping allows assessment of severity of injury in acute myocardial infarction. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2012;14:15. doi:10.1186/1532-429X-14-15.
Dall’Armellina E, Ferreira VM, Kharbanda RK, Prendergast B, Piechnik SK, Robson MD, et al. Diagnostic value of pre-contrast T1 mapping in acute and chronic myocardial infarction. J Am Coll Cardiol Img. 2013;6(6):739–42. doi:10.1016/j.jcmg.2012.11.020.
Kehr E, Sono M, Chugh SS, Jerosch-Herold M. Gadolinium-enhanced magnetic resonance imaging for detection and quantification of fibrosis in human myocardium in vitro. Int J Cardiovasc Imaging. 2008;24(1):61–8. doi:10.1007/s10554-007-9223-y.
Jerosch-Herold M, Sheridan DC, Kushner JD, Nauman D, Burgess D, Dutton D, et al. Cardiac magnetic resonance imaging of myocardial contrast uptake and blood flow in patients affected with idiopathic or familial dilated cardiomyopathy. Am J Physiol Heart Circ Physiol. 2008;295(3):H1234–42. doi:10.1152/ajpheart.00429.2008.
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM, et al. Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation. 2010;122(2):138–44. doi:10.1161/CIRCULATIONAHA.109.930636.
Miller C, Naish J, Bishop P, Coutts G, Clark D, Zhao S, et al. Histological validation of dynamic-equilibrium cardiovascular magnetic resonance for the measurement of myocardial extracellular volume. J Cardiovasc Magn Reson. 2013;15 Suppl 1:O16.
Kellman P, Wilson JR, Xue H, Ugander M, Arai AE. Extracellular volume fraction mapping in the myocardium, part 1: evaluation of an automated method. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2012;14:63. doi:10.1186/1532-429X-14-63.
Kim D, Jensen JH, Wu EX, Sheth SS, Brittenham GM. Breathhold multiecho fast spin-echo pulse sequence for accurate R2 measurement in the heart and liver. Magn Reson Med Off J Soc Magn Reson Med Soc Magn Reson Med. 2009;62(2):300–6. doi:10.1002/mrm.22047.
Huang TY, Liu YJ, Stemmer A, Poncelet BP. T2 measurement of the human myocardium using a T2-prepared transient-state TrueFISP sequence. Magn Reson Med Off J Soc Magn Reson Med Soc Magn Reson Med. 2007;57(5):960–6. doi:10.1002/mrm.21208.
Giri S, Chung YC, Merchant A, Mihai G, Rajagopalan S, Raman SV, et al. T2 quantification for improved detection of myocardial edema. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2009;11:56. doi:10.1186/1532-429X-11-56.
Giri S, Shah S, Xue H, Chung YC, Pennell ML, Guehring J, et al. Myocardial T(2) mapping with respiratory navigator and automatic nonrigid motion correction. Magn Reson Med Off J Soc Magn Reson Med Soc Magn Reson Med. 2012;68(5):1570–8. doi:10.1002/mrm.24139.
Ugander M, Bagi PS, Oki AJ, Chen B, Hsu LY, Aletras AH, et al. Myocardial edema as detected by pre-contrast T1 and T2 CMR delineates area at risk associated with acute myocardial infarction. J Am Coll Cardiol Img. 2012;5(6):596–603. doi:10.1016/j.jcmg.2012.01.016.
Thavendiranathan P, Walls M, Giri S, Verhaert D, Rajagopalan S, Moore S, et al. Improved detection of myocardial involvement in acute inflammatory cardiomyopathies using T2 mapping. Circ Cardiovasc Imaging. 2012;5(1):102–10. doi:10.1161/CIRCIMAGING.111.967836.
Nappi C, El Fakhri G. State of the art in cardiac hybrid technology: PET/MR. Curr Cardiovasc Imaging Rep. 2013;6(4):338–45. doi:10.1007/s12410-013-9213-5.
Cooper Jr LT, Fairweather D. We see only what we look for: imaging cardiac inflammation. Circ Cardiovasc Imaging. 2013;6(2):165–6. doi:10.1161/CIRCIMAGING.113.000166.
Yilmaz A, Ferreira V, Klingel K, Kandolf R, Neubauer S, Sechtem U. Role of cardiovascular magnetic resonance imaging (CMR) in the diagnosis of acute and chronic myocarditis. Heart Fail Rev. 2013;18(6):747–60. doi:10.1007/s10741-012-9356-5.
Chu GC, Flewitt JA, Mikami Y, Vermes E, Friedrich MG. Assessment of acute myocarditis by cardiovascular MR: diagnostic performance of shortened protocols. Int J Cardiovasc Imaging. 2013;29(5):1077–83. doi:10.1007/s10554-013-0189-7.
Piechnik SK, Ferreira VM, Lewandowski AJ, Ntusi NA, Banerjee R, Holloway C, et al. Normal variation of magnetic resonance T1 relaxation times in the human population at 1.5 T using ShMOLLI. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2013;15:13. doi:10.1186/1532-429X-15-13.
Ferreira VM, Piechnik SK, Dall’Armellina E, Karamitsos TD, Francis JM, Ntusi N, et al. Native T1-mapping detects the location, extent and patterns of acute myocarditis without the need for gadolinium contrast agents. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2014;16:36. doi:10.1186/1532-429X-16-36.
Luetkens JA, Doerner J, Thomas DK, Dabir D, Gieseke J, Sprinkart AM, et al. Acute myocarditis: multiparametric cardiac MR imaging. Radiology. 2014:132540. doi:10.1148/radiol.14132540.
Radunski UK, Lund GK, Stehning C, Schnackenburg B, Bohnen S, Adam G, et al. CMR in patients with severe myocarditis: diagnostic value of quantitative tissue markers including extracellular volume imaging. J Am Coll Cardiol Img. 2014;7(7):667–75. doi:10.1016/j.jcmg.2014.02.005.
Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation. 1978;58(6):1204–11.
Patel MR, Cawley PJ, Heitner JF, Klem I, Parker MA, Jaroudi WA, et al. Detection of myocardial damage in patients with sarcoidosis. Circulation. 2009;120(20):1969–77. doi:10.1161/CIRCULATIONAHA.109.851352.
White JA, Rajchl M, Butler J, Thompson RT, Prato FS, Wisenberg G. Active cardiac sarcoidosis: first clinical experience of simultaneous positron emission tomography–magnetic resonance imaging for the diagnosis of cardiac disease. Circulation. 2013;127(22):e639–41. doi:10.1161/CIRCULATIONAHA.112.001217.
Schneider S, Batrice A, Rischpler C, Eiber M, Ibrahim T, Nekolla SG. Utility of multimodal cardiac imaging with PET/MRI in cardiac sarcoidosis: implications for diagnosis, monitoring and treatment. Eur Heart J. 2014;35(5):312. doi:10.1093/eurheartj/eht335.
Mavrogeni S, Bratis K, Markussis V, Spargias C, Papadopoulou E, Papamentzelopoulos S, et al. The diagnostic role of cardiac magnetic resonance imaging in detecting myocardial inflammation in systemic lupus erythematosus. Differentiation from viral myocarditis. Lupus. 2013;22(1):34–43. doi:10.1177/0961203312462265.
Puntmann VO, D’Cruz D, Smith Z, Pastor A, Choong P, Voigt T, et al. Native myocardial T1 mapping by cardiovascular magnetic resonance imaging in subclinical cardiomyopathy in patients with systemic lupus erythematosus. Circ Cardiovasc Imaging. 2013;6(2):295–301. doi:10.1161/CIRCIMAGING.112.000151.
Pieroni M, De Santis M, Zizzo G, Bosello S, Smaldone C, Campioni M, et al. Recognizing and treating myocarditis in recent-onset systemic sclerosis heart disease: potential utility of immunosuppressive therapy in cardiac damage progression. Semin Arthritis Rheum. 2014;43(4):526–35. doi:10.1016/j.semarthrit.2013.07.006.
Fernandes F, Ramires FJ, Arteaga E, Ianni BM, Bonfa ES, Mady C. Cardiac remodeling in patients with systemic sclerosis with no signs or symptoms of heart failure: an endomyocardial biopsy study. J Card Fail. 2003;9(4):311–7. doi:10.1054/jcaf.2003.51.
Ntusi NA, Piechnik SK, Francis JM, Ferreira VM, Rai AB, Matthews PM, et al. Subclinical myocardial inflammation and diffuse fibrosis are common in systemic sclerosis—a clinical study using myocardial T1-mapping and extracellular volume quantification. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2014;16:21. doi:10.1186/1532-429X-16-21.
Thuny F, Lovric D, Schnell F, Bergerot C, Ernande L, Cottin V, et al. Quantification of myocardial extracellular volume fraction with cardiac MR imaging for early detection of left ventricle involvement in systemic sclerosis. Radiology. 2014;271(2):373–80. doi:10.1148/radiol.13131280.
Barison A, Gargani L, De Marchi D, Aquaro GD, Guiducci S, Picano E, et al. Early myocardial and skeletal muscle interstitial remodelling in systemic sclerosis: insights from extracellular volume quantification using cardiovascular magnetic resonance. Eur Heart J Cardiovasc Imaging. 2014. doi:10.1093/ehjci/jeu167.
Ntusi N, Piechnik S, Francis J, Ferreira V, Matthews P, Robson M, et al. Diffuse myocardial fibrosis and inflammation in rheumatoid arthritis: insights from cardiovascular magnetic resonance T1 mapping. JACC: Cardiovascular Imaging. 2014; Provisionally accepted.
Acknowledgments
This work was funded in part by the Robert Bosch Foundation (1) clinical research grant for inflammatory heart disease and (2) clinical research grant for myocardial involvement in rheumatic disorders, KKF-11-18, KKF-13-2]. Dr. Erica Dall’Armellina is a BHF intermediate clinical research fellow; BHF grant FS/13/71/30378. Dr. Vanessa Ferreira acknowledges funding and support from the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre based at The Oxford University Hospitals NHS Trust and the University of Oxford. We also thank Dr. Ntobeko Ntusi and Dr. Stefan Piechnik, University of Oxford, for providing images and colored T1 maps in Fig. 4.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Simon Greulich, Vanessa M Ferreira, Erica Dall’Armellina, and Heiko Mahrholdt declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiac Magnetic Resonance
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Greulich, S., Ferreira, V.M., Dall’Armellina, E. et al. Myocardial Inflammation—Are We There Yet?. Curr Cardiovasc Imaging Rep 8, 6 (2015). https://doi.org/10.1007/s12410-015-9320-6
Published:
DOI: https://doi.org/10.1007/s12410-015-9320-6