Abstract
Introduction
This literature review and exploratory network meta-analysis (NMA) aimed to compare the clinical effectiveness and tolerability of selective internal radiation therapy (SIRT) using yttrium-90 (Y-90) resin microspheres, regorafenib (REG), trifluridine–tipiracil (TFD/TPI), and best supportive care (BSC) in adult patients with chemotherapy-refractory or chemotherapy-intolerant metastatic colorectal cancer (mCRC).
Methods
In light of recently published data, the literature was searched to complement and update a review published in 2018. Studies up to December 2022 comparing two or more of the treatments and reporting overall survival (OS), progression-free survival (PFS), or incidence of adverse events (AE) were included. The NMA compared hazard ratios (HRs) for OS and PFS using Markov chain Monte Carlo techniques.
Results
Fifteen studies were included, with eight studies added (none addressing SIRT). All active treatments improved OS in relation to BSC. SIRT had the longest OS among all treatments, although without statistically significant differences (HR [95% credible interval] for SIRT, 0.48 [0.27, 0.87]; TFD/TPI, 0.62 [0.46, 0.83]; REG, 0.78 [0.57, 1.05]) in a fixed effects model. Information regarding SIRT was insufficient for PFS analysis, and TFD/TPI was the best intervention (HR 2.26 [1.6, 3.18]). One SIRT study reported radioembolization-induced liver disease in > 10% of the sample; this was symptomatically managed. Non-haematological AEs (hand-foot skin reaction, fatigue, diarrhoea, hypertension, rash or desquamation) were more common with REG, while haematological events (neutropoenia, leukopenia, and anaemia) were more common with TFD/TPI.
Conclusion
Current evidence supports SIRT treatment in patients with chemotherapy-refractory or chemotherapy-intolerant mCRC compared to newer oral agents, with comparable OS and low incidence of AEs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Selective internal radiation therapy (SIRT) using Y-90 resin microspheres had the highest probability of being ranked first for the overall survival outcome (surface under the cumulative ranking curve, 89.2%). |
There is evidence to support that all active treatments are superior to best supportive care for the outcomes of overall survival and progression-free survival. |
SIRT with Y-90 resin microspheres has fewer grade 3 adverse events compared with active comparators. |
SIRT using Y-90 resin microspheres shows more favourable response rates compared with the newer active agents. |
Introduction
Approximately 50–60% of patients diagnosed with colorectal cancer (CRC)—which accounts for 10.0% of all new cancer cases and 9.4% of all cancer-related deaths globally [1, 2]—will eventually develop metastatic disease (mCRC), with liver metastases responsible for more than half of mCRC cases and for two-thirds of CRC mortality [3]. Conventionally, surgical resection, adjuvant therapy, and neoadjuvant therapy, when recommended, represent the standard curative treatment for mCRC. However, only a minority of patients are suitable for upfront surgery, and patients with symptomatic and unresectable mCRC face a long treatment duration involving sequential combination chemotherapy as both first- and second-line treatments [4, 5]. In clinical practice, half of all patients with mCRC receiving first-line chemotherapy will relapse and progress to second-line therapies; of these, 25% are expected to progress to third-line therapies [6]. Nevertheless, systemic chemotherapy may itself cause hepatotoxicity and further complications, with many patients unable to tolerate multiple cycles [7]. For patients who depend on best supportive care (BSC), defined as palliative care aimed at improving quality of life, median survival is only 4–6 months [8]. Therefore, the poor prognosis after the recurrence of unresectable mCRC [9, 10], the hepatotoxicity of systemic chemotherapy [7], the high proportion of patients progressing to third-line therapies [6], and the limited median survival with BSC [8] warrant the search for new agents to treat mCRC.
Particularly for patients refractory to multiple lines of therapy, two agents, regorafenib (REG) and trifluridine–tipiracil (TFD/TPI), became available as third-line treatments after 2012 [11]. Another alternative, selective internal radiation therapy (SIRT) with yttrium-90 (Y-90) resin microspheres, has also emerged more recently as an innovative option for patients with liver-dominant mCRC, providing targeted radiotherapy through a one-off hospital procedure. A previous systematic review of literature (SRL) and meta-analysis showed that along with REG and TFD/TPI, SIRT with Y-90 resin microspheres is more effective than BSC in chemotherapy-resistant or chemotherapy-intolerant mCRC, with a favourable adverse event (AE) profile and increased overall survival (OS) [11]. Overall, recently published guidelines (Table S1 in the Supplementary Materials) [12,13,14,15] have advocated that SIRT be considered throughout the treatment pathway for patients with unresectable mCRC. The feasibility, safety, and favourable cost–benefit of SIRT with Y-90 resin microspheres have also been reported in a recent retrospective study in Switzerland [16].
Taking these aspects into consideration, the objective of the present study was to update the systematic literature review performed by Walter et al. [11] and to conduct an exploratory network meta-analysis (NMA) comparing the relative clinical effectiveness and tolerability of SIRT with Y-90 resin microspheres, REG, TFD/TPI, and BSC in patients with chemotherapy-refractory or chemotherapy-intolerant mCRC. Since that earlier review (Walter et al. [11]), new data, especially from randomised controlled trials, have become available, leading to the approval of TFD/TPI and REG in several countries. These new data are critical to guide decision-making, warranting an update the literature review including the analysis of OS, progression-free survival (PFS) and AEs.
Methods
An update of the systematic literature review by Walter et al. [11] was performed. The early review identified studies published up to December 2018 comparing two or more of the following treatments for chemotherapy-refractory or chemotherapy-intolerant mCRC: SIRT, TFD/TPI, REG, and BSC. Although the majority of publications from 2018 were covered in the original search reported by Walter et al. [11], we chose to include the year 2018 in the update to avoid missing relevant studies as a result of mismatches in publication/indexing dates. Thus, we searched for studies published from January 2018 up to December 2022. The review followed the Cochrane Handbook for Systematic Reviews of Interventions guidelines [17], and the results are reported in accordance with the PRISMA statement for Network Meta-Analyses [18].
The research question was structured according to the PICOS framework described in Table 1. Randomised controlled trials (RCTs) and observational studies focusing on adult patients with chemotherapy-refractory or chemotherapy-intolerant mCRC were included if they compared at least two of the following interventions: SIRT with Y-90 resin microspheres, TFD/TPI, REG, or BSC. Studies comparing any of the interventions with a placebo group were also included. Studies with designs, interventions, and populations different from the PICOS criteria were excluded.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Literature Search and Information Sources
The literature search strategies for the electronic databases MEDLINE, EMBASE, and Cochrane CENTRAL were based on MeSH or EMTREE terms as appropriate for the database search mechanism (Supplementary Materials Table S2). Searches were conducted on December 3, 2022.
Duplicates were removed with EndNote 20 software (EndNote 20, Thomson Reuters, New York, NY) and two independent reviewers (BMV and ALFA) selected articles by title and abstract for full-text review based on the inclusion criteria. Disagreements were resolved by consensus. In a subsequent stage, full texts were obtained and screened by the same two independent reviewers (BMV and ALFA). Disagreements were again resolved by consensus. All the study selection process was performed with Rayyan QCRI software [19]. Different publications from the same study were included only if reporting distinct outcomes.
Data were extracted to Excel (Microsoft Corp, Washington, USA) spreadsheets by two reviewers in duplicate. The following information was extracted: study characteristics (author and year, study type, interventions, and comparators) and locations; subject characteristics (sample size, median age, gender, Eastern Cooperative Oncology Group performance status [ECOG PS]); presence of KRAS mutation; presence of extrahepatic disease (EHD) aside from the primary site; presence of multiple sites of extrahepatic metastasis; number of prior chemotherapy regimens and drugs used for it; OS, PFS, and AEs. Data contents and formats were extracted to match the patient characteristics and outcomes reported in the Walter et al. [11] review. The authors of studies with missing or unclear data were contacted by e-mail for clarification.
Risk of Bias Within Individual Studies and Quality of the Body of Evidence
RCTs were evaluated for risk of bias (RoB) using the Cochrane risk of bias tool RoB 2.0 [20], considering the randomisation process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. The assessment of bias for non-RCTs was performed with the Risk Of Bias In Non-randomised Studies—of Interventions (ROBINS-I) tool [21] which considers confounding, selection of participants, classification of interventions, deviation from the intended interventions, missing data, measurement of outcomes, and selection of the reported results. The studies were initially rated by one reviewer (BMV), followed by a check performed by a second reviewer (ALFA). The Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to determine the quality of the evidence [22].
Network Meta-Analysis
An analysis was conducted for each outcome (5-year OS and PFS) separately. First, the approach proposed by DerSimonian and Laird was used for fitting the random effects model for meta-analysis of all pairs of interventions (including BSC) where data were available. The I2 statistic was calculated to investigate within-study heterogeneity. The extent of between-study heterogeneity was not estimated because of the small number of studies for each pair of direct evidence. An NMA was then performed to compare the clinical effectiveness of the interventions among themselves using BSC as the anchor. The model proposed by Lu and Ades was used with the arm-based approach [23]. To estimate hazard ratios (HRs), binomial likelihood with a complementary log–log link was used. Both fixed and random effects models with homogeneity of variances were developed. Visual inspection of autocorrelation plots was used to define the thinning interval and the trace plots to define the burn-in period and convergence.
The sample size (number of iterations after the burn-in period) was defined for a Monte Carlo error smaller than the standard error divided by 20 [24]. Values for thin, burn-in, and sample size were chosen for the random effects model and, for practicality, were repeated and checked for the fixed model. The consistency assumption was checked using the split node method. Comparison between the fixed and the random effects model fit was done using deviance information criterion (DIC). All analyses were performed using R with the “meta” package for pairwise and the “gemtc” for NMA. The analyses were updated using the same methods employed by Walter et al. [11].
Results
Systematic Review of the Literature
The literature search update yielded 1589 titles and abstracts. After duplicates were removed, 1403 titles and abstracts were assessed for eligibility. Of these, 19 articles were selected for full text assessment. In addition to the seven studies originally included in the review by Walter et al. [11], eight new publications met the eligibility criteria and were included [4, 25,26,27,28,29,30,31] (Fig. 1), resulting in a total of 15 studies. Of the eight new studies, three were RCTs [4, 30, 31] and five were observational studies [25,26,27,28,29].

Adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71
PRISMA 2020 flow diagram for the study selection process. aMEDLINE and EMBASE searches were made simultaneously in the embase.com search engine. bRecords excluded after assessment of title and abstract with the justification of not addressing the research question.
The key characteristics of the included studies are summarized in Table 2 [4, 25,26,27,28,29,30,31,32,33,34,35,36,37,38]. Of the new studies, none assessed SIRT; five studies compared TFD/TPI with REG [25,26,27,28,29], one compared TFD/TPI with a placebo group [30], and two compared REG with a placebo group [4, 31].
Risk of Bias and Quality of the Body of Evidence
The risk of bias was assessed for randomised and non-randomised studies separately. All RCTs presented low risk of bias for both OS and PFS (Supplementary Materials Tables S3 and S4). Two non-randomised studies presented critical risk of bias and the other five presented serious risk of bias (Supplementary Materials Table S5). The main issues in these studies referred to patient selection and lack of information on adjustments for confounders. Although blinding is not mandatory and also not possible for some outcomes, the fact that patients and investigators knew the intervention introduces some level of bias.
Assessment of the certainty of the evidence (GRADE) is shown in Supplementary Materials Tables S6–S9. There was moderate confidence in the effect size estimate for OS in the pairwise comparisons of SIRT versus BSC and of TFD/TPI versus REG. In the pairwise comparisons of TFD/TPI versus BSC and REG versus BSC, there was a high confidence effect estimate for both OS and PFS. The comparison between TFD/TPI and REG provided low certainty in the estimated effect for PFS. There were no available data to compare SIRT and BSC for PFS.
Population Characteristics
The demographic and clinical characteristics of the study populations are summarized in Supplementary Materials Table S10. The median age ranged from 55 to 68 years and most patients were men. Three of the eight new studies assessed the presence of KRAS mutation [28, 30, 31], detected in half of the population in one study [28] and in approximately one-third of the sample in the other two studies [30, 31]. Two found extrahepatic metastases in more than 70% of the population [26, 31]. Nakashima et al. [27] found three or more metastatic sites including the liver in about one third of the sample (2165 of 7279 patients); Xu et al. [30] also found three or more metastatic sites in about one third of the sample (158 out of 406 patients); however, location was not specified.
Considering all 15 studies, ECOG performance status was not reported in three studies [25, 27, 32]. EHD was an exclusion criterion in one study [33]. Two studies evaluated EHD [32, 34] and four described the number of metastatic sites (including the liver) [26, 31, 32, 34].
The proportion of patients exposed to previous chemotherapy is summarized in Supplementary Materials Table S11. Among the 15 studies, three did not provide information on the number of prior chemotherapy regimens [4, 27, 33], and five did not report the chemotherapeutic agent used [25, 26, 28]. Of the studies providing this information, most reported two or three prior chemotherapy regimens.
Network Meta-Analysis
Overall Survival
Thirteen studies provide HR results. Four of them compared REG with BSC [4, 31, 35, 36], three compared TFD/TPI with BSC [30, 37, 38], three compared SIRT using Y-90 resin microspheres with BSC [32,33,34], and the other three compared TAS with REG [26,27,28].
The fixed effects model had the best fit, with lower residual deviance (DIC < 3), and was therefore chosen for the base-case analysis. Random effects model results were calculated in a sensitivity analysis, with no change in the overall interpretation of the results (Table 3). The results of individual studies can be seen in Supplementary Materials Table S12.
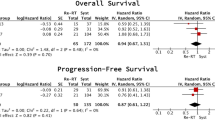
The HR (95% credible interval [95% CrI]) for OS considering SIRT versus BSC was 0.48 (0.27, 0.87); SIRT versus REG was 0.62 (0.32, 1.21); and SIRT versus TFD/TPI was 0.78 (0.4, 1.53). For TFD/TPI versus REG, HR was 0.79 (0.6, 1.06) for OS and 0.97 (0.65, 1.44) for PFS; for TFD/TPI versus BSC, HR was 0.62 (0.46, 0.83) for OS and 0.44 (0.31, 0.62) for PFS; and for REG versus BSC, HR was 0.78 (0.57, 1.05) for OS and 0.46 (0.33, 0.63) for PFS. HR estimates show SIRT using Y-90 resin microspheres as the best intervention from all compared treatments (point estimates of effect size), followed by TFD/TPI, REG, and BSC in the fixed effect model. This is confirmed by surface under the cumulative ranking curve (SUCRA) analysis (which indicates the probability of a treatment being ranked first among comparators in the NMA) (Table 4). Considering the results of both direct and indirect comparisons, any of the active comparators may be considered superior to BSC. Current evidence is unable to demonstrate statistically significant differences between SIRT, TFD/TPI, and REG in terms of OS.
A scenario analysis was performed to exclude studies assessing SIRT plus chemotherapy, which entailed exclusion of the Hendlisz et al. study [33]. In this analysis, the HR for OS, comparing SIRT versus BSC, yielded a HR of 0.37 (95% CrI 0.18, 0.75), indicating a notably more favourable outcome for SIRT using Y-90 resin microspheres.
Progression-Free Survival
Eight studies provided data for PFS analyses. Four studies compared REG with BSC [4, 31, 35, 36], three studies compared TFD/TPI with BSC [30, 37, 38], and one study compared TAS with REG [26]. Information regarding SIRT was not sufficient for inclusion in the PFS analysis. HR and SUCRA estimates suggest that TFD/TPI (HR 0.44 [0.33, 0.63]; SUCRA 0.56) has the highest probability of being the best intervention in terms of PFS followed by REG (HR 0.46 [0.33, 0.63]; SUCRA 0.44) in the fixed effects model. The graphic representation of the NMA for OS and PFS are shown in Supplementary Materials Fig. S1. The results of individual studies are shown in Supplementary Materials Table S12.
Adverse Events
None of the studies added to the present review reported on SIRT. Therefore, the percentage of patients experiencing grade 3 or higher adverse events remained the same for patients receiving SIRT as those reported by Walter et al. [11]: hand-food skin reaction (4.8% of the sample) [33] and radioembolization-induced liver disease (REILD) (10.3%), which was symptomatically managed [32]. It should be noted that in the study reporting hand-food skin reaction, SIRT was used in combination with 5-FU, which could explain these AEs. Conversely, higher levels of non-haematological AEs such as severe hand-foot skin reaction fatigue, diarrhoea, hypertension, and rash or desquamation are reported with REG compared to TFD/TPI and SIRT using Y-90 resin microspheres [26, 29]. While TFD/TPI was associated with a higher number of haematological events such as febrile neutropoenia (4%) [37] and with one death attributed to septic shock [37], grade 3 or higher drug-related AEs occurred in 57% patients receiving REG treatment compared to 37% patients receiving TFD/TPI treatment in the European Vitale et al. study [29] (Supplementary Materials Table S13), indicating a favourable safety profile for SIRT using Y-90 resin microspheres.
Discussion
This study set out to update the literature review and exploratory NMA performed by Walter et al. [11] comparing the relative clinical effectiveness and tolerability of SIRT using Y-90 resin microspheres, REG, TFD/TPI, and BSC in patients with chemotherapy-refractory or chemotherapy-intolerant mCRC, the second most lethal cancer and the third most prevalent malignant tumour worldwide [1]. The present results are consistent with that earlier review and NMA, which showed that all treatments improved OS in relation to BSC in patients with chemotherapy-refractory or chemotherapy-intolerant mCRC Walter et al. [11]. Based on pivotal RCTs for TFD/TPI and REG, the present updated NMA adds that SIRT using Y-90 resin microspheres had the longest OS among all treatments, with the highest probability of being ranked first followed by TFD/TPI and REG (SUCRA 89.2%). Information regarding SIRT was still insufficient for PFS NMA in the present study, with TFD/TPI presenting as the best intervention.
Also, the present findings indicate a persistent high incidence (> 10% of patients) of grade 3 or higher AE rates with TFD/TPI and REG [4, 26, 29,30,31]. Such AEs included hand-foot skin reaction, fatigue, diarrhoea, hypertension, and rash or desquamation for REG, while haematological events such as neutropoenia, leukopenia, and anaemia were more common with TFD/TPI [26, 29, 35, 37]. Therefore, even though no new studies focusing on SIRT have been added in the present literature review update, the AE profiles observed for REG and TFD/TPI corroborate an important advantage of SIRT using Y-90 resin microspheres in terms of grade 3 AEs or higher. As suggested by Walter et al. [11], the adverse event profile of SIRT using Y-90 resin microspheres vs. systemic therapy should be considered for clinical decision-making, but the absence of trials with a focus on AE profile is a gap in the literature and a limitation of the present NMA. Only one RCT compared SIRT with BSC for refractory mCRC, which limits any conclusions about toxicity and efficacy.
However, real-world evidence provides compelling support to SIRT in terms of safety outcomes [39, 40]. The European Multicentre Observational Study CIRT provides evidence of effectiveness and safety in a clinical setting where SIRT is largely considered to be a part of an only palliative treatment strategy across indications [40, 41]. During the CIRT study, 95 of 237 (40.1%) patients experienced 197 adverse events, with 28 of 237 (11.8%) patients having a grade 3 or higher adverse events: 4 (1.7%) had abdominal pain, 1 (0.4%) had nausea, 2 (0.8%) had gastrointestinal ulceration, 2 (0.8%) had gastritis, and 1 (0.4%) had radiation cholecystitis. In addition, 18 (7.6%) of the 237 patients experienced 29 all-cause “other” grade 3–4 adverse events [40]. In the Radiation-Emitting SIR-Spheres in Non-Resectable Liver (RESIN Registry) study, 43% received third-line and beyond. The rate of grade 3 or higher hepatic function toxicity was as low as 1.4% at 6 months among 347 patients [39]. In addition to that, a retrospective study in Switzerland demonstrated that only 7 (3.3%) out of 196 ambulatory patients had severe AEs requiring hospital readmission, leading to the conclusion that the safety profile of SIRT precludes hospital treatment which may also entail a higher cost–benefit associated with SIRT [16].
SIRT has emerged as a targeted treatment that delivers tumoricidal doses of radiation to liver metastasis while sparing healthy liver tissues, with important advantages in terms of administration. For example, it is now possible to perform the necessary mapping of the hepatic vasculature prior to SIRT as well as the SIRT procedure itself on the same day, so that only one hospital visit is needed instead of two. In addition to circumventing the issue of patient adherence (an issue with oral agents REG and TFD/TPI), an order-map-treat (OMT) program in which mapping of the hepatic vasculature and the SIRT procedure are performed on the same day in England has estimated savings with the reduction in hospital visits, from the payer perspective and from the patient perspective with less travel time [42].
A Delphi panel with practitioners including surgical oncologists, transplant surgeons, and hepatopancreatobiliary surgeons has also indicated that SIRT using Y-90 resin microspheres is effective at multiple points in the algorithm of liver-dominant mCRC management, i.e. for complete treatment of small metastases, as first-line therapy for liver metastases either alone or in combination with chemotherapy, in combination with second- or third-line chemotherapy, and as salvage therapy for patients who are chemotherapy-refractory. According to the authors, SIRT should be part of the treatment algorithm to control liver tumour progression before severe chemotherapy damage to the liver [43] (Supplementary Materials Table S1). The RESIN Registry study did use SIRT as first-line therapy in 17% of 442 participants, second-line therapy in 41% of participants and third-line therapy or beyond in 43% of participants. The median OS was 15.0 months (95% CI 13.3, 16.9) for the entire cohort and 13.9 months for first-line therapy, 17.4 months for second-line therapy, and 12.5 months for third-line therapy (χ2 = 9.7; P = 0.002). Whole-group PFS was 7.4 months (95% CI 6.4, 9.5), 7.9 months for first-line therapy, 10.0 months for second-line therapy, and 5.9 months for third-line therapy (χ2 = 8.3; P = 0.004) [39, 44].
It should be mentioned as a limitation that the studies of SIRT with Y-90 resin microspheres only included patients with liver-only or liver-dominant colorectal metastases, while studies of systemic treatment with REG or TFD/TPI included a not-only liver-dominant CRC-metastases population. However, since this exploratory NMA was undertaken comparing HRs, it is expected to capture differences in baseline characteristics across studies. It may also be noted that, although tumour response rate criterion was not studied in the present analysis, the results in terms of tumour response to treatment with SIRT using Y-90 resin microspheres should also be put into perspective with those of systemic treatments: indeed, no patient achieved a complete tumour response in recent observational studies of REG or TFD/TPI treatments with an objective response rate of 1–34% [4, 35] and 1–44% [25, 26], respectively, compared to 9.5–41% for SIRT using Y-90 resin microspheres [32, 33]. Other limitations include the fact that both RCTs and observational studies were included and that results are based on data extracted from published studies, rather than on individual patient data. Finally, the emergence of new treatment combinations and drugs will likely impact third-line mCRC treatments, such as TFD/TPI + bevacizumab and fruquintinib, with a median OS of 10.8 months [45] and 7.4 months respectively [46]. However, their trials results have been released in peer-reviewed articles after the SLR update search scope [45, 46].
SIRT using SIR-spheres was found to be cost-effective compared with BSC in the UK [47], and cost-effectiveness analyses have been conducted for other third-line mCRC treatments in relation to different comparators and in various geographies, leading to more uncertainty on the cost-effectiveness profile of REG and TFD/TPI versus BSC [48,49,50,51,52].
Conclusions
This updated systematic review of the literature with NMA provides both direct and indirect evidence for the efficacy comparisons among SIRT, REG, TFD/TPI, and BSC. There is evidence to support that all active treatments are superior to BSC for the outcomes OS and PFS. Although SIRT, TFD/TPI, and REG have comparable OS, the NMA indicated that SIRT using Y-90 resin microspheres had a higher probability of being ranked first in comparison to the other treatments (SUCRA 89.2%) for OS. The systematic review also indicated a more favourable grade 3 or higher adverse event profile for SIRT in comparison to REG or TFD/TPI. On the basis of these findings, the current evidence supports that SIRT using Y-90 resin microspheres provides a comparable effectiveness to newer orally active agents without the inconvenience of continuous treatment and with minimal potential for significant AEs.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Henry JT, Johnson B. Current and evolving biomarkers for precision oncology in the management of metastatic colorectal cancer. Chin Clin Oncol. 2019;8:49.
Takahashi H, Berber E. Role of thermal ablation in the management of colorectal liver metastasis. Hepatobiliary Surg Nutr. 2020;9:49–58.
Sanoff HK, Goldberg RM, Ivanova A, et al. Multicenter, randomized, double-blind phase 2 trial of FOLFIRI with regorafenib or placebo as second-line therapy for metastatic colorectal cancer. Cancer. 2018;124:3118–26.
Kow AWC. Hepatic metastasis from colorectal cancer. J Gastrointest Oncol. 2019;10:1274–98.
Abrams TA, Meyer G, Schrag D, Meyerhardt JA, Moloney J, Fuchs CS. Chemotherapy usage patterns in a US-wide cohort of patients with metastatic colorectal cancer. J Natl Cancer Inst. 2014;106:djt371.
Maor Y, Malnick S. Liver injury induced by anticancer chemotherapy and radiation therapy. Int J Hepatol. 2013;2013:815105.
Foubert F, Matysiak-Budnik T, Touchefeu Y. Options for metastatic colorectal cancer beyond the second line of treatment. Dig Liver Dis. 2014;46:105–12.
Sanoff HK, Sargent DJ, Campbell ME, et al. Five-year data and prognostic factor analysis of oxaliplatin and irinotecan combinations for advanced colorectal cancer: N9741. J Clin Oncol. 2008;26:5721–7.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Walter T, Hawkins NS, Pollock RF, Colaone F, Shergill S, Ross PJ. Systematic review and network meta-analyses of third-line treatments for metastatic colorectal cancer. J Cancer Res Clin Oncol. 2020;146:2575–87.
National Comprehensive Cancer Network. Rectal cancer, Version 3.2023. 2023. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1461. Accessed 22 June 2023.
National Comprehensive Cancer Network. Colon cancer, Version 2.2023. 2023. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1428. Accessed 23 June 2023.
Buzaid AC, Maluf FC, Barrios CH. Manual de Oncologia Clínica do Brasil. 2021. https://mocbrasil.com/. Accessed 03 Dec 2022.
Cervantes A, Adam R, Roselló S, et al. Metastatic colorectal cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023;34:10–32.
Aberle S, Kenkel D, Becker AS, et al. Outpatient yttrium-90 microsphere radioembolization: assessment of radiation safety and quantification of post-treatment adverse events causing hospitalization. Radiol Med. 2020;125:971–80.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). 2022. www.training.cochrane.org/handbook. Accessed 03 Dec 2022.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355: i4919.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105–24.
Cowles MK. Applied Bayesian statistics: with R and OpenBUGS examples. New York: Springer; 2013.
Hsieh MC, Rau KM, Lin SE, et al. An observational study of trifluridine/tipiracil-containing regimen versus regorafenib-containing regimen in patients with metastatic colorectal cancer. Front Oncol. 2022;12: 867546.
Moriwaki T, Fukuoka S, Taniguchi H, et al. Propensity score analysis of regorafenib versus trifluridine/tipiracil in patients with metastatic colorectal cancer refractory to standard chemotherapy (REGOTAS): a Japanese Society for Cancer of the Colon and Rectum multicenter observational study. Oncologist. 2018;23:7–15.
Nakashima M, Takeuchi M, Kawakami K. Effectiveness and safety of regorafenib vs. trifluridine/tipiracil in unresectable colorectal cancer: a retrospective cohort study. Clin Colorectal Cancer. 2020;19:e208–25.
Patel AK, Abhyankar R, Brais LK, et al. Trifluridine/tipiracil and regorafenib in patients with metastatic colorectal cancer: a retrospective study at a tertiary oncology center. Oncologist. 2021;26:e2161–9.
Vitale P, Zanaletti N, Famiglietti V, et al. Retrospective study of regorafenib versus TAS-102 efficacy and safety in chemorefractory metastatic colorectal cancer (mCRC) patients: a multi-institution real life clinical data. Clin Colorectal Cancer. 2021;20:227–35.
Xu J, Kim TW, Shen L, et al. Results of a randomized, double-blind, placebo-controlled, phase III trial of trifluridine/tipiracil (TAS-102) monotherapy in asian patients with previously treated metastatic colorectal cancer: the TERRA study. J Clin Oncol. 2018;36:350–8.
Xu J, Xu RH, Qin S, et al. Regorafenib in Chinese patients with metastatic colorectal cancer: Subgroup analysis of the phase 3 CONCUR trial. J Gastroenterol Hepatol. 2020;35:1307–16.
Seidensticker R, Denecke T, Kraus P, et al. Matched-pair comparison of radioembolization plus best supportive care versus best supportive care alone for chemotherapy refractory liver-dominant colorectal metastases. Cardiovasc Intervent Radiol. 2012;35:1066–73.
Hendlisz A, Van den Eynde M, Peeters M, et al. Phase III trial comparing protracted intravenous fluorouracil infusion alone or with yttrium-90 resin microspheres radioembolization for liver-limited metastatic colorectal cancer refractory to standard chemotherapy. J Clin Oncol. 2010;28:3687–94.
Bester L, Meteling B, Pocock N, et al. Radioembolization versus standard care of hepatic metastases: comparative retrospective cohort study of survival outcomes and adverse events in salvage patients. J Vasc Interv Radiol. 2012;23:96–105.
Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–12.
Li J, Qin S, Xu R, et al. Regorafenib plus best supportive care versus placebo plus best supportive care in Asian patients with previously treated metastatic colorectal cancer (CONCUR): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2015;16:619–29.
Mayer RJ, Van Cutsem E, Falcone A, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015;372:1909–19.
Yoshino T, Mizunuma N, Yamazaki K, et al. TAS-102 monotherapy for pretreated metastatic colorectal cancer: a double-blind, randomised, placebo-controlled phase 2 trial. Lancet Oncol. 2012;13:993–1001.
Emmons EC, Bishay S, Du L, et al. Survival and toxicities after. Radiology. 2022;305:228–36.
Schaefer N, Grözinger G, Pech M, et al. Prognostic factors for effectiveness outcomes after transarterial radioembolization in metastatic colorectal cancer: results from the multicentre observational study CIRT. Clin Colorectal Cancer. 2022;21:285–96.
Helmberger T, Golfieri R, Pech M, et al. Clinical application of trans-arterial radioembolization in hepatic malignancies in Europe: first results from the prospective multicentre observational study CIRSE registry for SIR-spheres therapy (CIRT). Cardiovasc Intervent Radiol. 2021;44:21–35.
Pollock RF, Shergill S, Carion PL, von Oppen N, Agirrezabal I, Brennan VK. Advances in delivery of selective internal radiation therapy (SIRT): economic and logistical effects of same-stay work-up and procedure in the treatment of unresectable liver tumors in England. Adv Ther. 2023;40:294–309.
Jeyarajah DR, Doyle MBM, Espat NJ, et al. Role of yttrium-90 selective internal radiation therapy in the treatment of liver-dominant metastatic colorectal cancer: an evidence-based expert consensus algorithm. J Gastrointest Oncol. 2020;11:443–60.
Frantz S, Matsuoka L, Vaheesan K, et al. Multicenter evaluation of survival and toxicities of hepatocellular carcinoma following radioembolization: analysis of the resin registry. J Vasc Interv Radiol. 2021;32:845–52.
Prager GW, Taieb J, Fakih M, et al. Trifluridine-tipiracil and bevacizumab in refractory metastatic colorectal cancer. N Engl J Med. 2023;388:1657–67.
Dasari A, Lonardi S, Garcia-Carbonero R, et al. Fruquintinib versus placebo in patients with refractory metastatic colorectal cancer (FRESCO-2): an international, multicentre, randomised, double-blind, phase 3 study. Lancet. 2023;402:41–53.
Brennan VK, Colaone F, Shergill S, et al. A cost-utility analysis of SIR-Spheres Y-90 resin microspheres versus best supportive care in the treatment of unresectable metastatic colorectal cancer refractory to chemotherapy in the UK. J Med Econ. 2020;23:1588–97.
Goldstein DA, Ahmad BB, Chen Q, et al. Cost-effectiveness analysis of regorafenib for metastatic colorectal cancer. J Clin Oncol. 2015;33:3727–32.
Cho SK, Hay JW, Barzi A. Cost-effectiveness analysis of regorafenib and TAS-102 in refractory metastatic colorectal cancer in the United States. Clin Colorectal Cancer. 2018;17:e751–61.
Kashiwa M, Matsushita R. Comparative cost-utility analysis of regorafenib and trifluridine/tipiracil in the treatment of metastatic colorectal cancer in Japan. Clin Ther. 2020;42:1376–87.
Bullement A, Underhill S, Fougeray R, et al. Cost-effectiveness of trifluridine/tipiracil for previously treated metastatic colorectal cancer in England and Wales. Clin Colorectal Cancer. 2018;17:e143–51.
Gourzoulidis G, Maniadakis N, Petrakis D, et al. Economic evaluation of trifluridine and tipiracil hydrochloride in the treatment of metastatic colorectal cancer in Greece. J Comp Eff Res. 2019;8:133–42.
Funding
Sponsorship for this study and the journal's Rapid Service and Open Access Fees were funded by Sirtex Medical United Kingdom Ltd.
Author information
Authors and Affiliations
Contributions
Conceptualization: André L. Ferreira Azeredo-da-Silva, Ion Agirrezabal, Victoria K Brennan, Phuong Lien Carion, Nathalie Amoury, Bruna Muhlinberg Vetromilla, Suki Shergill; Methodology: Victor Hugo Fonseca de Jesus; Data curation: André L. Ferreira Azeredo-da-Silva, Bruna Stella Zanotto, Bruna Muhlinberg Vetromilla, Patricia Klarmann Ziegelmann; Formal analysis: André L. Ferreira Azeredo-da-Silva, Bruna Stella Zanotto, Bruna Muhlinberg Vetromilla, Patricia Klarmann Ziegelmann; Writing – original draft: André L. Ferreira Azeredo-da-Silva, Bruna Muhlinberg Vetromilla, Bruna Stella Zanotto, Patricia Klarmann Ziegelmann; Writing – review and editing: André L. Ferreira Azeredo-da-Silva, Victor Hugo Fonseca de Jesus, Ion Agirrezabal, Victoria K Brennan, Phuong Lien Carion, Nathalie Amoury, Bruna Stella Zanotto, Suki Shergill, Patricia Klarmann Ziegelmann.
Corresponding author
Ethics declarations
Conflict of Interest
Ion Agirrezabal was affiliated with Sirtex Medical at the time of the study. They now work for Sanofi. Victoria K. Brennan was affiliated with Sirtex Medical at the time of the study. They now work for Open Health. Phuong L. Carion was a Sirtex Medical employee at the time of the analysis. Nathalie Amoury was a Sirtex Medical employee at the time of the analysis. Suki Shergill was a Sirtex Medical employee at the time of the analysis. Bruna S. Zanotto was working on behalf of Sirtex Medical on the project. Bruna M. Vetromilla was working on behalf of Sirtex Medical on the project. André L. F. Azeredo-da-Silva was working on behalf of Sirtex Medical on the project. Patricia K. Ziegelmann was working on behalf of Sirtex Medical on the project. Victor Hugo F. de Jesus has received honoraria for academic purposes and consulting for Sirtex.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Azeredo-da-Silva, A.L.F., de Jesus, V.H.F., Agirrezabal, I. et al. Selective Internal Radiation Therapy Using Y-90 Resin Microspheres for Metastatic Colorectal Cancer: An Updated Systematic Review and Network Meta-Analysis. Adv Ther 41, 1606–1620 (2024). https://doi.org/10.1007/s12325-024-02800-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02800-5