Abstract
Introduction
Collectively, coronary artery disease (CAD) and peripheral artery disease (PAD) are highly prevalent and are associated with increased risk of major adverse cardiovascular events (MACE) and major adverse limb events (MALE). Improved ability to identify those at highest risk of these events may help optimize secondary prevention efforts in this population.
Methods
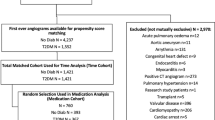
Using the Optum Integrated Database, a healthcare claims database linked to electronic medical records (EMR), we identified patients with CAD and/or PAD between January 1, 2009, and September 30, 2016. Index date was the earliest date on which chronic and stable disease was established. Follow-up ran from index date until earliest of patient death, plan disenrollment, or end of study. We developed multivariate Cox proportional hazards models to identify predictors of MACE and/or MALE, limited to measures presumed available to clinicians during patient encounters (e.g., age, presence of selected comorbidities).
Results
A total of 20,932 patients met all selection criteria; 86.9% had CAD and 26.1% had PAD; 13% (n = 2753) experienced MACE and/or MALE during a mean follow-up of 2.3 years, for a rate of 7.1 events per 100 person-years (PYs). We identified 11 predictors of MACE and/or MALE. Most (95.1%) patients had ≥ 1 predictors; 34.0% and 6.9% had ≥ 4 and ≥ 6, respectively. Incidence of MACE and/or MALE was strongly correlated with number of predictors (r2 = 0.98), ranging from 2.3 per 100 PYs among those without predictors (4.9% of patients) to 18.7 per 100 PYs among those with ≥ 6 (6.9%). Patients with ≥ 1 predictor experienced 7.4 MACE and/or MALE per 100 PYs.
Conclusion
Readily identifiable predictors can be used to identify subgroups with chronic CAD and/or PAD at elevated risk of MACE and/or MALE. Further research is required to understand the degree to which these subgroups may benefit from early identification and treatment with secondary prevention therapies.
Funding
Janssen Pharmaceuticals.


Similar content being viewed by others
Change history
13 January 2020
In the original article. The third author name is incorrect. The correct name is Nicholas J. Leeper.
References
Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann Transl Med. 2016;4(13):256.
Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–603.
Yazdanyar A, Newman AB. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. 2009;25(4):563–77 (vii).
Bhatt DL, Eagle KA, Ohman EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA. 2010;304(12):1350–7.
Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(12):e726–79.
World Health Organization (WHO). The top 10 causes of death. 2018. http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.Published.201/. Accessed 30 Nov 2018.
Khoury H, Lavoie L, Welner S, Folkerts K. The burden of major adverse cardiac events and antiplatelet prevention in patients with coronary or peripheral arterial disease. Cardiovasc Ther. 2016;34(2):115–24.
Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835–42.
Boersma E, Pieper KS, Steyerberg EW, et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation. 2000;101(22):2557–67.
Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163(19):2345–53.
Paramore LC, Thomas SK, Knopf KB, Cragin LS, Fraeman KH. Estimating costs of care for patients with newly diagnosed metastatic colorectal cancer. Clin Colorectal Cancer. 2006;6(1):52–8.
Armstrong PW, Fu Y, Chang WC, et al. Acute coronary syndromes in the GUSTO-IIb trial: prognostic insights and impact of recurrent ischemia. The GUSTO-IIb Investigators. Circulation. 1998;98(18):1860–8.
Lee KL, Woodlief LH, Topol EJ, et al. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. GUSTO-I Investigators. Circulation. 1995;91(6):1659–68.
Janssen US. FDA approves XARELTO® (rivaroxaban) to reduce the risk of major cardiovascular events in patients with chronic coronary artery disease (CAD) or peripheral artery disease (PAD). 2018. https://www.janssen.com/us-fda-approves-xareltor-rivaroxaban-reduce-risk-major-cardiovascular-events-patients-chronic. Updated October 11. Accessed 30 Nov 2018.
Eikelboom J, Connolly S, Bosch J, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377:1319–30.
Huybrechts KF, Rothman KJ, Silliman RA, Brookhart MA, Schneeweiss S. Risk of death and hospital admission for major medical events after initiation of psychotropic medications in older adults admitted to nursing homes. CMAJ. 2011;183(7):E411–9.
Mitchell SL. Care of patients with advanced dementia. 2018. https://www.uptodate.com/contents/care-of-patients-with-advanced-dementia#H423254540. Accessed 18 Sep 2019.
Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529–38.
Luepker RV, Steffen LM, Duval S, Zantek ND, Zhou X, Hirsch AT. Population trends in aspirin use for cardiovascular disease prevention 1980–2009: the Minnesota Heart Survey. J Am Heart Assoc. 2015;4:12.
Ferencik M, Mayrhofer T, Bittner DO, et al. Use of high-risk coronary atherosclerotic plaque detection for risk stratification of patients with stable chest pain: a secondary analysis of the PROMISE randomized clinical trial. JAMA Cardiol. 2018;3(2):144–52.
Kronzon I, Tunick PA. Aortic atherosclerotic disease and stroke. Circulation. 2006;114(1):63–75.
Acknowledgements
Funding
This work was sponsored by Janssen Pharmaceuticals who were responsible for financing the study and the decision to publish the findings. The journal’s Rapid Service Fee was funded by Janssen Pharmaceuticals.
Editorial Assistance
We thank Sean Smith of Evidera for his editorial assistance in the development of this manuscript. This assistance was funded by Janssen Pharmaceuticals.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Ariel Berger is employed by Evidera, a research and consulting company to the biopharma industry. In this salaried position, he works with a variety of companies and organizations and is precluded from receiving payment or honoraria directly from these organizations for services rendered. Brian Murphy is employed by Evidera, a research and consulting company to the biopharma industry. In this salaried position, he works with a variety of companies and organizations and is precluded from receiving payment or honoraria directly from these organizations for services rendered. Beth Nordstrom is employed by Evidera, a research and consulting company to the biopharma industry. In this salaried position, she works with a variety of companies and organizations and is precluded from receiving payment or honoraria directly from these organizations for services rendered. Nicholas J. Leeper reports other modest research support from Bayer and Janssen. Windsor Ting reports a modest research grant from Janssen. Jeffrey Berger reports other modest research support from Janssen and AstraZeneca. Qi Zhao is currently employed at Eisai, Woodcliff Lake, NJ, USA. Alex Simpson was an employee of Evidera at the time research was conducted.
Compliance with Ethics Guidelines
This was a retrospective database study that used only completely de-identified data. Accordingly, institutional review board approval and informed consent were neither required nor sought.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available because of being “work for hire,” but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original version of this article was revised due to incorrect name of the third author in the author group.
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.9963986.
Rights and permissions
About this article
Cite this article
Berger, A., Simpson, A., Leeper, N.J. et al. Real-World Predictors of Major Adverse Cardiovascular Events and Major Adverse Limb Events Among Patients with Chronic Coronary Artery Disease and/or Peripheral Arterial Disease. Adv Ther 37, 240–252 (2020). https://doi.org/10.1007/s12325-019-01132-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-019-01132-z