Abstract
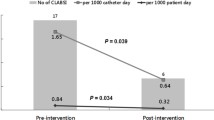
Central line-associated bloodstream infections (CLABSIs) can result in worse outcomes and high hospitalization cost for patients. This study aimed to assess the effectiveness of multi-department cooperation, intelligent prevention, and supervision (MDCIPS) in reducing the incidence of CLABSIs and improving the clinical outcomes of the patients. Key issues were identified through a literature review and survey on the status quo. A MDCIPS model was thus built. A total of 440 patients with indwelling central venous catheters (CVCs) were enrolled in the study. The control group (n = 219) received conventional infection-control managements, while the intervention group (n = 221) received MDCIPS interventions in addition to conventional infection-control managements. The number of CLABSIs patients, incidence of CLABSIs, average length of hospital stay, average total hospitalization cost, and disease outcomes were compared between the two groups. The intervention group had a significant reduction in the number and incidence of CLABSIs (0[0%] vs. 4[1.33%], P < 0.05). Two of the four patients with CLABSIs in the control group died. The average length of hospital stay was significantly longer in the control group than the intervention group (17 days vs. 13 days, P < 0.001). The average hospitalization cost in the control group was much higher than that in the intervention group (92.8 thousand yuan vs. 65.2 thousand yuan, P < 0.001). Patient outcome was improved in the intervention group than the control group (P = 0.001). In summary, the MDCIPS model effectively reduces the incidence of CLABSIs, alleviates the patients’ economic burden, and improves the clinical outcomes of the patients.
Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CVC:
-
Central Venous Catheter
- PICC:
-
Peripherally-Inserted Central Catheter
- CLABSIs:
-
Central Line-Associated Bloodstream Infection
- MDCIPS:
-
Multi-Department Cooperation, Intelligent Prevention, and Supervision
- KABP:
-
Knowledge-Attitude-Belief-Practice
References
Shashi KK, Callahan MJ, Tsai A (2022) Diagnostic challenges with central venous catheter studies. Pediatr Radiol 52(8):1581–1591. https://doi.org/10.1007/s00247-022-05362-2
Ford WJH, Bundy DG, Oyeku S, Heo M, Saiman L, Rosenberg RE, DeLaMora P, Rabin B, Zachariah P, Mirhaji P, Klein E, Obaro-Best O, Drasher M, Peshansky A, Rinke ML (2021) Central Venous Catheter Salvage in Ambulatory Central Line-Associated Bloodstream Infections. Pediatrics 148(6):e2020042069. https://doi.org/10.1542/peds.2020-042069
Mandolfo S, Anesi A, Maggio M, Rognoni V, Galli F, Forneris G (2020) High success rate in salvage of catheter-related bloodstream infections due to Staphylococcus aureus, on behalf of project group of Italian society of nephrology. J Vasc Access 21(3):336–341. https://doi.org/10.1177/1129729819875323
Rupp ME, Karnatak R (2018) Intravascular Catheter-Related Bloodstream Infections. Infect Dis Clin North Am 32(4):765–787. https://doi.org/10.1016/j.idc.2018.06.002
Cantón-Bulnes ML, Garnacho-Montero J (2019) Practical approach to the management of catheter-related bloodstream infection. Rev Esp Quimioter 32(Suppl 2):38–41
Cai Y, Zhu M, Sun W, Cao X, Wu H (2018) Study on the cost attributable to central venous catheter-related bloodstream infection and its influencing factors in a tertiary hospital in China. Health Qual Life Outcomes 16(1):198. https://doi.org/10.1186/s12955-018-1027-3
Warren DK, Zack JE, Mayfield JL, Chen A, Prentice D, Fraser VJ, Kollef MH (2004) The effect of an education program on the incidence of central venous catheter-associated bloodstream infection in a medical ICU. Chest 126(5):1612–1618. https://doi.org/10.1378/chest.126.5.1612
Buetti N, Marschall J, Drees M, Fakih MG, Hadaway L, Maragakis LL, Monsees E, Novosad S, O’Grady NP, Rupp ME, Wolf J, Yokoe D, Mermel LA (2022) Strategies to prevent central line-associated bloodstream infections in acute-care hospitals: 2022 Update. Infect Control Hosp Epidemiol 43(5):1–17. https://doi.org/10.1017/ice.2022.87
Pérez-Granda MJ, Carrillo CS, Rabadán PM, Valerio M, Olmedo M, Muñoz P, Bouza E (2022) Increase in the frequency of catheter-related bloodstream infections during the COVID-19 pandemic: a plea for control. J Hosp Infect 119:149–154. https://doi.org/10.1016/j.jhin.2021.09.020
Fakih MG, Bufalino A, Sturm L, Huang RH, Ottenbacher A, Saake K, Winegar A, Fogel R, Cacchione J (2022) Coronavirus disease 2019 (COVID-19) pandemic, central-line-associated bloodstream infection (CLABSI), and catheter-associated urinary tract infection (CAUTI): The urgent need to refocus on hardwiring prevention efforts. Infect Control Hosp Epidemiol 43(1):26–31. https://doi.org/10.1017/ice.2021.70
Al Qadire M, Hani AM (2022) Nurses’ and physicians’ knowledge of guidelines for preventing catheter-related blood stream infections. Nurs Crit Care 27(4):594–601. https://doi.org/10.1111/nicc.12577
Walz JM, Ellison RT 3rd, Mack DA, Flaherty HM, McIlwaine JK, Whyte KG, Landry KE, Baker SP, Heard SO (2015) CCOC Research Group. The bundle “plus”: the effect of a multidisciplinary team approach to eradicate central line-associated bloodstream infections. Anesth Analg 120(4):868–76. https://doi.org/10.1213/ANE.0b013e3182a8b01b
Curto-García N, García-Suárez J, Callejas Chavarria M, Gil Fernández JJ, Martín Guerrero Y, Magro Mazo E, Marcellini Antonio S, Juárez LM, Gutierrez I, Arranz JJ, Montalvo I, Elvira C, Domínguez P, Díaz MT, Burgaleta C (2016) A team-based multidisciplinary approach to managing peripherally inserted central catheter complications in high-risk haematological patients: a prospective study. Support Care Cancer 24(1):93–101. https://doi.org/10.1007/s00520-015-2754-1
Choi JY, Kwak YG, Yoo H, Lee SO, Kim HB, Han SH, Choi HJ, Kim YK, Kim SR, Kim TH, Lee H, Chun HK, Kim JS, Eun BW, Kim DW, Koo HS, Bae GR, Lee K (2015) Korean Nosocomial Infections Surveillance System (KONIS). Trends in the incidence rate of device-associated infections in intensive care units after the establishment of the Korean Nosocomial Infections Surveillance System. J Hosp Infect 91(1):28–34. https://doi.org/10.1016/j.jhin.2015.06.002
Hussain AS, Ahmed AM, Arbab S, Ariff S, Ali R, Demas S, Zeb J, Rizvi A, Saleem A, Farooqi J (2021) CLABSI reduction using evidence based interventions and nurse empowerment: a quality improvement initiative from a tertiary care NICU in Pakistan. Arch Dis Child 106(4):394–400. https://doi.org/10.1136/archdischild-2019-318779
Guidelines for Prevention and Control of Vessel catheter-associated Infections (2021 edition). Infectious Disease Information. 2021;004:034. https://www.nstl.gov.cn/paper_detail.html?id=afe7aca92adeecaa0a2f467df52283dc. Accessed 2024 Feb 25
National Health Commission of the People's Republic of China. Statement of the Goals for Improving National Medical Quality and Safety in 2021.Chinese Practical Journal of Rural Doctor. 2021;3: 13–16. http://qikan.cqvip.com/Qikan/Article/Detail?id=7104352860. Accessed 2024 Feb 25
Hallam C, Jackson T, Rajgopal A, Russell B (2018) Establishing catheter-related bloodstream infection surveillance to drive improvement. J Infect Prev 19(4):160–166. https://doi.org/10.1177/1757177418767759
Institute of Hospital Administration, National Health Commission. Procedure Quality Control Kit for Preventing intravascular catheter-related bloodstream infections (trial version) May 2021. https://niha.org.cn/hwaciis/ueditor/jsp/upload/file/20211022/1634869866944016594.pdf. Accessed 2024 Feb 25
Wang M, Zhang L, Cai W, Lian H, Sha F, Ye H (2019) Effect of application of the knowledge-attitude-practice model on the reduction of catheter-related bloodstream infections. Chinese J Nosocomiol 29(16):2542-2545,2560
Wang X, Lu H, Ma Q, Wang W, Zhao L, Li J, Wang J, Geng Y, Shi W, Xu B, Chen J (2020) Research progress of risk factors for central venous catheter-related bloodstream infection. Med J Natl Defend Force Northwest China 41(9):584–589
Laboratory Physician Branch of Chinese Medical Doctor Association (2017) Expert consensus on diagnostic reporting patterns for catheter-associated bloodstream infections. Natl Med J China 97(18):1376–1379
General Office of the National Health Commission. Notice of the General Office of the National Health Commission on printing and distributing Indicators of Medical Quality Control in Pharmaceutical Administration and Nursing (2020 edition): Medical letter from the National Health Office〔2020〕No.654 [EB/OL].[2020–8–4][2022–8–11]. http://www.gov.cn/zhengce/zhengceku/2020-08/05/content_5532636.htm. Accessed 2024 Feb 25
Geng Y, Huang H, Liu J, Yang Q, Duan W, Cao H (2022) Research on internal optimization path of hospital average length of stay based on gradient descent method. Chinese Hospital Manag 42(12):47–49
Han L, Ding J, Qi F, Le H (2022) Study on the Change Trend and Influencing Factors of the Total Hospitalization Expenses of Wounded and Sick Military Casualties with Fractures from 2016 to 2020 in a Tertiary Hospital of a Troop. Military Med J South China 8:657–622
Vashi PG, Virginkar N, Popiel B, Edwin P, Gupta D (2017) Incidence of and factors associated with catheter-related bloodstream infection in patients with advanced solid tumors on home parenteral nutrition managed using a standardized catheter care protocol. BMC Infect Dis 17(1):372. https://doi.org/10.1186/s12879-017-2469-7
Tao F, Jiang R, Chen Y, Chen R (2015) Risk factors for early onset of catheter-related bloodstream infection in an intensive care unit in China: a retrospective study. Med Sci Monit 21:550–556. https://doi.org/10.12659/MSM.892121
Jayaweera JAAS, Sivakumar D (2020) Asymptomatic central line-associated bloodstream infections in children implanted with long term indwelling central venous catheters in a teaching hospital, Sri Lanka. BMC Infect Dis 20(1):457. https://doi.org/10.1186/s12879-020-05190-5
Moon HM, Kim S, Yun KW, Kim HY, Jung SE, Choi EH, Lee HJ (2018) Clinical Characteristics and Risk Factors of Long-term Central Venous Catheter-associated Bloodstream Infections in Children. Pediatr Infect Dis J 37(5):401–406. https://doi.org/10.1097/INF.0000000000001849
Pitiriga V, Bakalis J, Kampos E, Kanellopoulos P, Saroglou G, Tsakris A (2022) Duration of central venous catheter placement and central line-associated bloodstream infections after the adoption of prevention bundles: a two-year retrospective study. Antimicrob Resist Infect Control 11(1):96. https://doi.org/10.1186/s13756-022-01131-w
Pitiriga V, Kanellopoulos P, Bakalis I, Kampos E, Sagris I, Saroglou G, Tsakris A (2020) Central venous catheter-related bloodstream infection and colonization: the impact of insertion site and distribution of multidrug-resistant pathogens. Antimicrob Resist Infect Control 9(1):189. https://doi.org/10.1186/s13756-020-00851-1
Bell T, O’Grady NP (2017) Prevention of Central Line-Associated Bloodstream Infections. Infect Dis Clin North Am 31(3):551–559. https://doi.org/10.1016/j.idc.2017.05.007
Tang H, Zhang L, Chen Y, Li Y, Xu L (2020) Application of nurse specialist-led multidisciplinary cooperation in quality control of peripherally inserted central venous catheter placement. J Clin Nurs Pract 6(05):22–25
Wilder KA, Wall B, Haggard D, Epperson T (2016) CLABSI Reduction Strategy: A Systematic Central Line Quality Improvement Initiative Integrating Line-Rounding Principles and a Team Approach. Adv Neonatal Care 16(3):170–177. https://doi.org/10.1097/ANC.0000000000000259
Zhang L, Zhang Z, Zhang Q, Zang G, Tang N, Jia M, Li B (2020) The influence of intelligent hand hygiene monitoring system on reducing the incidence of catheter-related bloodstream infections. Chinese J Pract Nurs 36(31):2450–2454
Buetti N, Timsit JF (2019) Management and Prevention of Central Venous Catheter-Related Infections in the ICU. Semin Respir Crit Care Med 40(4):508–523. https://doi.org/10.1055/s-0039-1693705
Funding
This study was supported by Science Foundation of Hunan Province(N0.2019JJ80052), Scientific Research Project of Hunan Provincial Health Commission(N0.20201976), and Science Foundation of Changsha City (N0.kq2208435).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interests
The authors declare of no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, C., Dai, F., Yang, D. et al. Application of Multi-Department Cooperation, Intelligent Prevention, and Supervision to Reduce the Incidence of Central Line-Associated Bloodstream Infections. Indian J Hematol Blood Transfus (2024). https://doi.org/10.1007/s12288-024-01760-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12288-024-01760-8