Abstract
Purpose
In breast cancer, FoxP3-positive tumor-infiltrating lymphocytes (FoxP3+ TILs) vary depending on lymph node status, histological grade, and subtype. All these studies have compared the numbers of FoxP3+ TILs among different hosts, but recruitment of FoxP3+ TILs might depend on each individual’s immune environment and each tumor’s biological characteristics. In the present study, FoxP3+ TIL numbers were investigated in patients with synchronous bilateral breast cancer (SBBC) to determine the factors that affect FoxP3+ TIL recruitment in the same anti-tumor immune environment.
Methods
Patients diagnosed with SBBC who underwent curative surgery at two institutions were enrolled in this study. Patients who underwent primary systemic therapy or who were diagnosed with ductal carcinoma in situ or who had distant metastases at diagnosis were excluded. The average numbers of Foxp3+ TILs were determined from the scores of five high-power microscopic fields (HPF). The associations between Foxp3+ TIL numbers and the clinicopathological features of bilateral breasts in a single individual were examined.
Results
Nuclear grade (NG) (p = 0.007) and subtype (p = 0.03), but not size (p = 0.18) and axillary lymph node (p = 0.23) were significantly associated with increase of FoxP3 + TIL numbers by univariate analysis. Further, only NG was a statistically significant clinicopathological factor for change in the number of FoxP3+ TILs by multivariate analysis (p = 0.046)
Conclusions
There was no relationship between FoxP3+ TIL numbers and cancer progression as reflected in tumor size and axillary lymph node in patients with SBBC. Aggressive biological factors, especially high NG, were significantly related to enhanced recruitment of FoxP3+ TILs.




Similar content being viewed by others

References
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–64.
Fridman WH, Zitvogel L, Sautès-Fridman C, Kroemer G. The immune contexture in cancer prognosis and treatment. Nat Rev Clin Oncol. 2017;14(12):717–34.
Wing K, Sakaguchi S. Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol. 2010; 11(1):7–13
Levings MK, Sangregorio R, Human RMG. cd25(+)cd4(+) t regulatory cells suppress naive and memory T cell proliferation and can be expanded invitro without loss of function. J Exp Med. 2001;193(11):1295–302.
Ng WF, Duggan PJ, Ponchel F, Matarese G, Lombardi G, Edwards AD, et al. Human CD4(+)CD25(+) cells: a naturally occurring population of regulatory T cells. Blood. 2001;98(9):2736–44.
Shevach EM. CD4+ CD25+ suppressor T cells: more questions than answers. Nat Rev Immunol. 2002;2(6):389–400.
Bach JF. Regulatory T cells under scrutiny. Nat Rev Immunol. 2003;3(3):189–98.
Coffer PJ, Burgering BM. Forkhead-box transcription factors and their role in the immune system. Nat Rev Immunol. 2004;4(11):889–99.
Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Sci (N Y). 2003;299(5609):1057–61.
Sakaguchi S, Ono M, Setoguchi R, Yagi H, Hori S, Fehervari Z, et al. Foxp3+ CD25+ CD4+ natural regulatory T cells in dominant self-tolerance and autoimmune disease. Immunol Rev. 2006;212:8–27.
deLeeuw RJ, Kost SE, Kakal JA, Nelson BH. The prognostic value of FoxP3+ tumor-infiltrating lymphocytes in cancer: a critical review of the literature. Clin Cancer Res. 2012;18(11):3022–9.
Sakaguchi S. Naturally arising Foxp3-expressing CD25 + CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat Immunol. 2005;6(4):345–52.
Jiang D, Gao Z, Cai Z, Wang M, He J. Clinicopathological and prognostic significance of FOXP3+ tumor infiltrating lymphocytes in patients with breast cancer: a meta-analysis. BMC Cancer. 2015;15:727.
Nichol AM, Yerushalmi R, Tyldesley S, Lesperance M, Bajdik CD, Speers C, et al. A case-match study comparing unilateral with synchronous bilateral breast cancer outcomes. J Clin Oncol. 2011;29(36):4763–8.
Verkooijen HM, Chatelain V, Fioretta G, Vlastos G, Rapiti E, Sappino AP, et al. Survival after bilateral breast cancer: results from a population-based study. Breast Cancer Res Treat. 2007;105(3):347–57.
Kurebayashi J, Miyosi Y, Ishikawa T, Saji S, Sugie T, Suzuki T, et al. Clinicopathological characteristics of breast cancer and trends in the management of breast cancer patients in Japan: Based on the Breast Cancer Registry of the Japanese Breast Cancer Society between 2004 and 2011. Breast Cancer. 2015;22(3):235–44.
Japanese Breast Cancer Society. General rules for clinical and pathological recording of breast cancer, the 17 Kanehara & Co. Ltd, Tokyo; 2012.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31(31):3997–4013.
Aruga T, Suzuki E, Saji S, Horiguchi S, Horiguchi K, Kitagawa D, et al. A low number of tumor-infiltrating FOXP3-positive cells during primary systemic chemotherapy correlates with favorable anti-tumor response in patients with breast cancer. Oncol Rep. 2009;22:273–8.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48(3):452–8.
Padmanabhan N, Subramanyan A, Radhakrishna S. Synchronous bilateral breast cancers. J Clin Diagn Res. 2015;9(9):XC05–8.
Renz DM, Böttcher J, Baltzer PA, Dietzel M, Vag T, Gajda M, et al. The contralateral synchronous breast carcinoma: a comparison of histology, localization, and magnetic resonance imaging characteristics with the primary index cancer. Breast Cancer Res Treat. 2010;120(2):449–59.
Baker B, Morcos B, Daoud F, Sughayer M, Shabani H, Salameh H, et al. Histo-biological comparative analysis of bilateral breast cancer. Med Oncol. 2013;30(4):711.
Liu F, Lang R, Zhao J, Zhang X, Fan Y, et al. CD8+ cytotoxic T cell and FOXP3+ regulatory T cell infiltration in relation to breast cancer survival and molecular subtypes. Breast Cancer Res Treat. 2011;130(2):645–55.
Martin F, Ladoire S, Mignot G, Apetoh L, Ghiringhelli G. Human FOXP3 and cancer. Oncogene. 2010;29:4121–9.
Acknowledgements
We thank Ms. Tomoko Nagai, medical technician of department of pathology Showa University School of Medicine, for technical assistance with immunostaining method.
Funding
The present study was supported by Clinical Research Found of Tokyo Metropolitan Government (Grant no. H290303015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of Showa University Hospital (approval number #1969), and Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital (approval number #1638).
Informed consent
Participants comprehensively provided their consent stating that the tissue samples from resected specimen may be used for various researches. The ethics committee of Showa University Hospital (approval number #1969), and Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital (approval number #1638) approved the authors’ request for waiver of informed consent based on ethical consideration. All patients have the option to confirm ongoing studies on Showa University and Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital web sites and may choose to opt out of consent at any time. The ethics committee approved this consent procedure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12282_2020_1049_MOESM2_ESM.tif
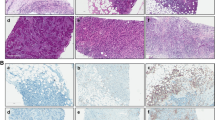
Supplementary Fig. 2 The median of FoxP3-positive tumor-infiltrating lymphocytes (FoxP3+ TILs) increased in order from luminal type with nuclear grade (NG) 1/2, luminal type with NG3, HER2 type, to basal-type (TIF 5000 kb)
About this article
Cite this article
Goto, R., Hirota, Y., Aruga, T. et al. The number of FoxP3-positive tumor-infiltrating lymphocytes in patients with synchronous bilateral breast cancer. Breast Cancer 27, 586–593 (2020). https://doi.org/10.1007/s12282-020-01049-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-020-01049-4