Abstract
Background
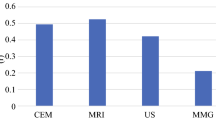
Enhanced magnetic resonance imaging (MRI) and ultrasonography (US) are used to assess residual lesions after preoperative chemotherapy before surgery. However, residual lesion assessments based on preoperative imaging often differ from postoperative pathologic diagnoses. We retrospectively reviewed the accuracy of preoperative residual lesion assessments, including ductal carcinoma in situ (DCIS) cases to find criteria for cases in which surgery can be omitted.
Methods
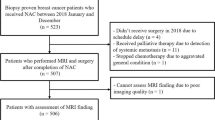
We reviewed 201 patients who received preoperative chemotherapy and surgery in our hospital from January 2013 to November 2016. Presurgical evaluations regarding the possible existence of residual lesions, and clinical Complete Response (cCR) or non-cCR, were compared with postoperative pathological diagnoses.
Results
Of the 201 patients, 52 were diagnosed with cCR, and 39 with pathological complete response (pCR). Predictions for residual lesions were 86.4% sensitive, 76.9% specific, and 84.6% accurate. When patients were divided into 4 groups by estrogen receptor (ER) and HER2 status, sensitivity in each group was ER+/HER2−: 91.4%; ER−/HER2−: 94.1%; ER+/HER2+: 78.6%; and ER−/HER2+: 78.5%. Of the 22 patients preoperatively assessed with cCR, but diagnosed with non-pCR, the median invasive residual tumor size was 2 mm (range 0–46 mm); 5 patients (22.7%) had only DCIS.
Conclusions
Predicting residual lesions after preoperative chemotherapy by using MRI and US is a reasonable strategy. However, current methods are inadequate for identifying patients who can omit surgery; therefore, a new strategy for detecting small tumors in these patients is needed.

Similar content being viewed by others
References
Fisher BB, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from national surgical adjuvant breast and bowel project B-18. J Clin Oncol. 1997;15:2483–93.
Rastogi P, Anderson SJ, Bear HD, Geyer CE, Kahlenberg MS, Robidoux A, et al. Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27. J Clin Oncol. 2008;26:778–85.
van der Hage JH, van de Velde CC, Mieog SJ. Preoperative chemotherapy for women with operable breast cancer. In: Mieog SJ, editor. Cochrane Database Syst Rev [Internet]. Chichester: John Wiley & Sons, Ltd.; 2007. https://doi.org/10.1002/14651858.CD005002.pub2.
Esserman LJ, Berry D a, DeMichele A, Carey L, Davis SE, Buxton M, et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J Clin Oncol [Internet]. 2012;30:3242–9. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3434983&tool=pmcentrez&rendertype=abstract.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet (London, England). 2014;384:164–72 (Internet). Available from: http://www.ncbi.nlm.nih.gov/pubmed/24529560.
Symmans WF, Wei C, Gould R, Yu X, Zhang Y, Liu M, et al. Long-term prognostic risk after neoadjuvant chemotherapy associated with residual cancer burden and breast cancer subtype. J Clin Oncol. 2017;35:JCO2015631010 (Internet). Available from: http://www.ncbi.nlm.nih.gov/pubmed/28135148.
von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–804. https://doi.org/10.1200/JCO.2011.38.8595 (Intranet).
Ring A, Webb A, Ashley S, Allum WH, Ebbs S, Gui G, et al. Is surgery necessary after complete clinical remission following neoadjuvant chemotherapy for early breast cancer? J Clin Oncol. 2003;21:4540–5.
Peintinger F, Kuerer HM, Anderson K, Boughey JC, Meric-bernstam F, Singletary SE, et al. Accuracy of the combination of mammography and sonography in predicting tumor response in breast cancer patients after neoadjuvant chemotherapy. Ann Oncol. 2006;13:1443–9.
Vriens BEPJ, De Vries B, Lobbes MBI, Van Gastel SM, Van Den Berkmortel FWPJ, Smilde TJ, et al. Ultrasound is at least as good as magnetic resonance imaging in predicting tumour size post-neoadjuvant chemotherapy in breast cancer. Eur J Cancer. 2016;52:67–76. https://doi.org/10.1016/j.ejca.2015.10.010.
Straver ME, Loo CE, Rutgers EJT, Oldenburg HSA, Wesseling J, Vrancken Peeters MJTFD, et al. MRI-model to guide the surgical treatment in breast cancer patients after neoadjuvant chemotherapy. Ann Surg. 2010;251:701–7.
McGuire KP, Toro-Burguete J, Dang H, Young J, Soran A, Zuley M, et al. MRI staging after neoadjuvant chemotherapy for breast cancer: does tumor biology affect accuracy? Ann Surg Oncol. 2011;18:3149–54 (Internet). Available from: http://www.ncbi.nlm.nih.gov/pubmed/21947592.
Yuan Y, Chen XS, Liu SY, Shen KW. Accuracy of MRI in prediction of pathologic complete remission in breast cancer after preoperative therapy: a meta-analysis. Am J Roentgenol. 2010;195:260–8.
Mussurakis S, Buckley DL, Coady AM, Turnbull LW, Horsman A. Observer variability in the interpretation of contrast enhanced MRI of the breast. Br J Radiol. 1996;69:1009–16. https://doi.org/10.1259/0007-1285-69-827-1009 (Internet).
Belli P, Costantini M, Malaspina C, Magistrelli A, LaTorre G, Bonomo L. MRI accuracy in residual disease evaluation in breast cancer patients treated with neoadjuvant chemotherapy. Clin Radiol. 2006;61:946–53.
Rosen EL, Blackwell KL, Baker JA, Soo MS, Bentley RC, Yu D, et al. Accuracy of MRI in the detection of residual breast cancer after neoadjuvant chemotherapy. AJR Am J Roentgenol. 2003;181:1275–82.
Lee HJ, Seo AN, Kim EJ, Jang MH, Suh KJ, Ryu HS, et al. HER2 heterogeneity affects trastuzumab responses and survival in patients with her2-positive metastatic breast cancer. Am J Clin Pathol. 2014;142:755–66.
Arnould L, Arveux P, Couturier J, Gelly-Marty M, Loustalot C, Ettore F, et al. Pathologic complete response to trastuzumab-based neoadjuvant therapy is related to the level of HER-2 amplification. Clin Cancer Res. 2007;13:6404–9.
Lee HJ, Kim JY, Park SY, Park IA, Song IH, Yu JH, et al. Clinicopathologic significance of the intratumoral heterogeneity of HER2 gene amplification in HER2-positive breast cancer patients treated with adjuvant trastuzumab. Am J Clin Pathol. 2015;144:570–8.
Bianchini G, Balko JM, Mayer IA, Sanders ME, Gianni L. Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol [Internet]. Nature Publishing Group; 2016;13:674–90. Available from: https://doi.org/10.1038/nrclinonc.2016.66%5Cn http://www.ncbi.nlm.nih.gov/pubmed/27184417.
Jiang T, Shi W, Wali VB, Pongor LS, Li C, Lau R, et al. Predictors of chemosensitivity in triple negative breast cancer: an integrated genomic analysis. PLoS Med. 2016;13:1–23.
Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, Dhingra K, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17:460. https://doi.org/10.1200/JCO.1999.17.2.460.
Acknowledgements
The authors thank all the staff from the Departments of Breast Oncology and Pathology, Aichi Cancer Center Hospital, for their help in collecting the clinical data. We also extend special thanks to Mr. David Ujike and Asuka Kropp M.D. for their help.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
About this article
Cite this article
Iwase, M., Sawaki, M., Hattori, M. et al. Assessing residual cancer cells using MRI and US after preoperative chemotherapy in primary breast cancer to omit surgery. Breast Cancer 25, 583–589 (2018). https://doi.org/10.1007/s12282-018-0856-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-018-0856-6