Abstract
Purpose of Review
Cryptococcal meningitis is one of the most seriously opportunistic infections in people living with HIV. We evaluated clinical and laboratorial features (minimum inhibitory concentrations for fluconazole, initial fungal burden in cerebrospinal fluid) and risk factors associated with in-hospital mortality.
Recent Findings
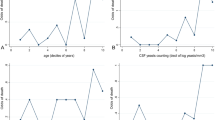
There is no good evidence for the use of minimum inhibitory concentrations for fluconazole in routine practice for the management of cryptococcosis patients. Counting yeast cells at cerebrospinal fluid can predict positive culture by not death.
Summary
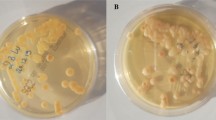
Data from 46 cryptococcal meningitis patients were reviewed, retrospectively. Patients who presented yeast cell count greater than 400 yeast cells/μ in their initial cerebrospinal fluid sample were associated with higher mortality (p = 0.014); moreover, the yeast cell count is an easy and cheap assay, with high values possibly associated to poor prognosis. Additionally, we verified no significant differences between fluconazole susceptibility profile, molecular type, clinical presentation, cytological analyses, time to sterilize the cerebrospinal fluid, agent recovering out of central nervous system, previous diagnosis of cryptococcal meningitis or usage of fluconazole, and overall mortality.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
GERMS-SA Annual Report 2016.
Jarvis JN, Boulle A, Loyse A, et al. High ongoing burden of cryptococcal disease in Africa despite antiretroviral roll out. AIDS. 2009;23(9):1182–3. https://doi.org/10.1097/QAD.0b013e32832be0fc.
• Meyer W, Castañeda A, Jackson S, et al. Molecular typing of IberoAmerican Cryptococcus neoformans isolates. Emerg Infect Dis. 2003:189–95 http://repositorio.unesp.br/handle/11449/67195. Accessed June 19, 2016. IberoAmerican molecular epidemiology of Cryptococcus.
• Hagen F, Khayhan K, Theelen B, Kolecka A, Polacheck I, Sionov E, et al. Recognition of seven species in the Cryptococcus gattii/Cryptococcus neoformans species complex. Fungal Genet Biol. 2015;78:16–48. https://doi.org/10.1016/j.fgb.2015.02.009Nomenclature consensus ofCryptococcusspecies.
• Kwon-Chung KJ, Bennett JE, Wickes BL, et al. The Case for Adopting the “Species Complex” Nomenclature for the Etiologic Agents of Cryptococcosis. Lorenz M, ed. mSphere. 2017;2(1). doi:https://doi.org/10.1128/mSphere.00357-16. Nomenclature consensus ofCryptococcusspecies.
• Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17(8):873–81. https://doi.org/10.1016/S1473-3099(17)30243-8Global epidemiology of cryptococcal meningitis.
Jarvis JN, Harrison TS. HIV-associated cryptococcal meningitis. Aids. 2007;21(16):2119–29 http://journals.lww.com/aidsonline/Citation/2007/10180/HIV_associated_cryptococcal_meningitis.1.aspx. Accessed 23 June 2016.
Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23(4):525–30. https://doi.org/10.1097/QAD.0b013e328322ffac.
Lanjewar DN. The spectrum of clinical and pathological manifestations of AIDS in a consecutive series of 236 autopsied cases in Mumbai, India. Pathol Res Int. 2011;2011:1–12. https://doi.org/10.4061/2011/547618.
Lortholary O, Poizat G, Zeller V, et al. Long-term outcome of AIDS-associated cryptococcosis in the era of combination antiretroviral therapy. AIDS (London, England). 2006;20(17):2183–91. https://doi.org/10.1097/01.aids.0000252060.80704.68.
Vidal JE, Penalva de Oliveira AC, Dauar RF, Boulware DR. Strategies to reduce mortality and morbidity due to AIDS-related cryptococcal meningitis in Latin America. Braz J Infect Dis. 2013;17(3):353–62. https://doi.org/10.1016/j.bjid.2012.10.020.
de Oliveira RB, Atobe JH, Souza SA, de Castro Lima Santos DW. Epidemiology of invasive fungal infections in patients with acquired immunodeficiency syndrome at a reference hospital for infectious diseases in Brazil. Mycopathologia. 2014;178(1–2):71–8. https://doi.org/10.1007/s11046-014-9755-3.
Pappalardo MCSM, Szeszs MW, Martins MA, Baceti LB, Bonfietti LX, Purisco SU, et al. Susceptibility of clinical isolates of Cryptococcus neoformans to amphotericin B using time-kill methodology. Diagn Microbiol Infect Dis. 2009;64(2):146–51. https://doi.org/10.1016/j.diagmicrobio.2009.02.007.
• World Health Organization. Guidelines for the Diagnosis, Prevention and Management of Cryptococcal Disease in HIV-Infected Adults, Adolescents and Children: Supplement to the 2016 Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection.; 2018. http://www.ncbi.nlm.nih.gov/books/NBK531449/. Accessed 2 June 2019. Cryptococcal disease guideline from WHO.
• Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(3):291–322. https://doi.org/10.1086/649858Cryptococcal disease guideline from Infectious Diseases Society of America.
Brandt ME, Pfaller MA, Hajjeh RA, Hamill RJ, Pappas PG, Reingold AL, et al. Trends in antifungal drug susceptibility of Cryptococcus neoformans isolates in the United States: 1992 to 1994 and 1996 to 1998. Antimicrob Agents Chemother. 2001;45(11):3065–9. https://doi.org/10.1128/AAC.45.11.3065-3069.2001.
Armengou A, Porcar C, Mascaró J, García-Bragado F. Possible development of resistance to fluconazole during suppressive therapy for AIDS-associated cryptococcal meningitis. Clin Infect Dis. 1996;23(6):1337–8 http://cid.oxfordjournals.org/content/23/6/1337.2.short. Accessed June 19, 2016.
Berg J, Clancy CJ, Nguyen MH. The hidden danger of primary fluconazole prophylaxis for patients with AIDS. Clin Infect Dis. 1998;26(1):186–7 http://cid.oxfordjournals.org/content/26/1/186.2.short. Accessed June 19, 2016.
Dalhoff A, Ambrose PG, Mouton JW. A long journey from minimum inhibitory concentration testing to clinically predictive breakpoints: deterministic and probabilistic approaches in deriving breakpoints. Infection. 2009;37(4):296–305. https://doi.org/10.1007/s15010-009-7108-9.
Kahlmeter G. European harmonization of MIC breakpoints for antimicrobial susceptibility testing of bacteria. J Antimicrob Chemother. 2003;52(2):145–8. https://doi.org/10.1093/jac/dkg312.
Chandenier J, Adou-Bryn KD, Douchet C, Sar B, Kombila M, Swinne D, et al. In vitro activity of amphotericin B, fluconazole and voriconazole against 162 Cryptococcus neoformans isolates from Africa and Cambodia. Eur J Clin Microbiol Infect Dis. 2004;23(6):506–8. https://doi.org/10.1007/s10096-004-1136-2.
Chong HS, Dagg R, Malik R, Chen S, Carter D. In vitro susceptibility of the yeast pathogen Cryptococcus to fluconazole and other azoles varies with molecular genotype. J Clin Microbiol. 2010;48(11):4115–20. https://doi.org/10.1128/JCM.01271-10.
De Bedout C, Ordóñez N, Gómez BL, et al. In vitro antifungal susceptibility of clinical isolates of Cryptococcus neoformans var. neoformans and C. neoformans var. gattii. Rev Iberoam Micol. 1999;16:36–9 http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.380.1233&rep=rep1&type=pdf. Accessed June 23, 2016.
Govender NP, Patel J, van Wyk M, Chiller TM, Lockhart SR, for the Group for Enteric, Respiratory and Meningeal Disease Surveillance in South Africa (GERMS-SA). Trends in antifungal drug susceptibility of Cryptococcus neoformans isolates obtained through population-based surveillance in South Africa in 2002-2003 and 2007-2008. Antimicrob Agents Chemother. 2011;55(6):2606–11. https://doi.org/10.1128/AAC.00048-11.
• Pfaller MA, Castanheira M, Diekema DJ, Messer SA, Jones RN. Wild-type MIC distributions and epidemiologic cutoff values for fluconazole, posaconazole, and voriconazole when testing Cryptococcus neoformans as determined by the CLSI broth microdilution method. Diagn Microbiol Infect Dis. 2011;71(3):252–9. https://doi.org/10.1016/j.diagmicrobio.2011.07.007Epidemiological cutoff values forCryptococcus.
Thompson GR, Wiederhold NP, Fothergill AW, Vallor AC, Wickes BL, Patterson TF. Antifungal susceptibilities among different serotypes of Cryptococcus gattii and Cryptococcus neoformans. Antimicrob Agents Chemother. 2009;53(1):309–11. https://doi.org/10.1128/AAC.01216-08.
•• Espinel-Ingroff A, Aller AI, Canton E, Castañón-Olivares LR, Chowdhary A, Cordoba S, et al. Cryptococcus neoformans-Cryptococcus gattii species complex: an international study of wild-type susceptibility endpoint distributions and epidemiological cutoff values for fluconazole, itraconazole, posaconazole, and voriconazole. Antimicrob Agents Chemother. 2012;56(11):5898–906. https://doi.org/10.1128/AAC.01115-12Epidemiological cutoff values forCryptococcus—international isolates.
• Dannaoui E, Abdul M, Arpin M, Michel-Nguyen A, Piens MA, Favel A, et al. Results obtained with various antifungal susceptibility testing methods do not predict early clinical outcome in patients with Cryptococcosis. Antimicrob Agents Chemother. 2006;50(7):2464–70. https://doi.org/10.1128/AAC.01520-05Antifungal susceptibility testing methods and cryptococcal meningitis outcome.
Witt MD, Lewis RJ, Larsen RA, Milefchik EN, Leal MA, Haubrich RH, et al. Identification of patients with acute AIDS-associated cryptococcal meningitis who can be effectively treated with fluconazole: the role of antifungal susceptibility testing. Clin Infect Dis. 1996;22(2):322–8 http://cid.oxfordjournals.org/content/22/2/322.short. Accessed June 19, 2016.
• Aller AI, Martin-Mazuelos E, Lozano F, Gomez-Mateos J, Steele-Moore L, Holloway WJ, et al. Correlation of fluconazole MICs with clinical outcome in cryptococcal infection. Antimicrob Agents Chemother. 2000;44(6):1544–8 http://aac.asm.org/content/44/6/1544.short. Accessed June 19, 2016. Antifungal susceptibility testing methods and cryptococcal meningitis outcome.
Graybill JR, Sobel J, Saag M, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. Clin Infect Dis. 2000;30(1):47–54 http://cid.oxfordjournals.org/content/30/1/47.short. Accessed June 19, 2016.
•• Vidal JE, Gerhardt J, Peixoto de Miranda ÉJ, et al. Role of quantitative CSF microscopy to predict culture status and outcome in HIV-associated cryptococcal meningitis in a Brazilian cohort. Diagn Microbiol Infect Dis. 2012;73(1):68–73. https://doi.org/10.1016/j.diagmicrobio.2012.01.014Role of quantitative cerebrospinal fluid microscopy to predict outcome.
Del Poeta M, Toffaletti DL, Rude TH, Dykstra CC, Heitman J, Perfect JR. Topoisomerase I is essential in Cryptococcus neoformans: role in pathobiology and as an antifungal target. Genetics. 1999;152(1):167–78 http://www.genetics.org/content/152/1/167.short. Accessed June 19, 2016.
Aoki FH, Imai T, Tanaka R, Mikami Y, Taguchi H, Nishimura NF, et al. New PCR primer pairs specific for Cryptococcus neoformans serotype A or B prepared on the basis of random amplified polymorphic DNA fingerprint pattern analyses. J Clin Microbiol. 1999;37(2):315–20 http://jcm.asm.org/content/37/2/315.short. Accessed June 19, 2016.
Chaturvedi S, Rodeghier B, Fan J, McClelland CM, Wickes BL, Chaturvedi V. Direct PCR of Cryptococcus neoformans MATalpha and MATa pheromones to determine mating type, ploidy, and variety: a tool for epidemiological and molecular pathogenesis studies. J Clin Microbiol. 2000;38(5):2007–9.
Espinel-Ingroff A, Chowdhary A, Cuenca-Estrella M, Fothergill A, Fuller J, Hagen F, et al. Cryptococcus neoformans-Cryptococcus gattii species complex: an international study of wild-type susceptibility endpoint distributions and epidemiological cutoff values for amphotericin B and flucytosine. Antimicrob Agents Chemother. 2012;56(6):3107–13. https://doi.org/10.1128/AAC.06252-11.
Saag MS, Powderly WG, Cloud GA, et al. Comparison of amphotericin B with fluconazole in the treatment of acute AIDS-associated cryptococcal meningitis. The NIAID Mycoses Study Group and the AIDS Clinical Trials Group. N Engl J Med. 1992;326(2):83–9. https://doi.org/10.1056/NEJM199201093260202.
Bicanic T, Muzoora C, Brouwer AE, et al. Independent association between rate of clearance of infection and clinical outcome of HIV-associated Cryptococcal meningitis: analysis of a combined cohort of 262 patients. Clin Infect Dis. 2009;49(5):702–9. https://doi.org/10.1086/604716.
Jarvis JN, Bicanic T, Loyse A, et al. Determinants of mortality in a combined cohort of 501 patients with HIV-associated Cryptococcal meningitis: implications for improving outcomes. Clin Infect Dis. 2014;58(5):736–45. https://doi.org/10.1093/cid/cit794.
Cerikçioğlu N. Mating types, sexual reproduction and ploidy in fungi: effects on virulence. Mikrobiyol Bul. 2009;43(3):507–13.
Matsumoto MT, Fusco-Almeida AM, Baeza LC, M de Melhem SC, Medes-Giannini MJS. Genotyping, serotyping and determination of mating-type of Cryptococcus neoformans clinical isolates from São Paulo State, Brazil. Rev Inst Med Trop São Paulo. 2007;49(1):41–7.
Trilles L, M dos Lazéra S, Wanke B, et al. Regional pattern of the molecular types of Cryptococcus neoformans and Cryptococcus gattii in Brazil. Mem Inst Oswaldo Cruz. 2008;103(5):455–62 http://www.scielo.br/scielo.php?pid=S0074-02762008000500008&script=sci_arttext&tlng=es. Accessed June 19, 2016.
Souza LKH, Ode Fernandes FL, Kobayashi CCBA, et al. Antifungal susceptibilities of clinical and environmental isolates of Cryptococcus neoformans in Goiânia city, Goiás, Brazil. Rev Inst Med Trop São Paulo. 2005;47(5):253–6 doi:/S0036–46652005000500003.
Matos CS, de Souza AA, Oliveira NS, Barros TF. Microbiological characteristics of clinical isolates of Cryptococcus spp. in Bahia, Brazil: molecular types and antifungal susceptibilities. Eur J Clin Microbiol Infect Dis. 2012;31(7):1647–52. https://doi.org/10.1007/s10096-011-1488-3.
Favalessa OC, de Paula DAJ, Dutra V, Nakazato L, Tadano T, Lazera Mdos S, et al. Molecular typing and in vitro antifungal susceptibility of Cryptococcus spp from patients in Midwest Brazil. J Infect Dev Ctries. 2014;8(8):1037–43.
Day JN, Duong VA, Chau TTH, Hoang TN, Wolbers M. Relationship of susceptibility testing of Cryptococcus neoformans to survival and mycological cleareance in HIV associated cryptococcal meningitis. Mycoses. 2014:33–108.
Turnidge J, Kahlmeter G, Kronvall G. Statistical characterisation of bacterial wild-type MIC value distributions and the determination of epidemiological cut-off values. Clin Microbiol Infect. 2006;12(5):418–25. https://doi.org/10.1111/j.1469-0691.2006.01377.x.
Park BJ, Arthington-Skaggs BA, Hajjeh RA, Iqbal N, Ciblak MA, Lee-Yang W, et al. Evaluation of amphotericin B interpretive breakpoints for Candida bloodstream isolates by correlation with therapeutic outcome. Antimicrob Agents Chemother. 2006;50(4):1287–92. https://doi.org/10.1128/AAC.50.4.1287-1292.2006.
Schwarz P, Dromer F, Lortholary O, Dannaoui E. Efficacy of amphotericin B in combination with flucytosine against flucytosine-susceptible or flucytosine-resistant isolates of Cryptococcus neoformans during disseminated murine Cryptococcosis. Antimicrob Agents Chemother. 2006;50(1):113–20. https://doi.org/10.1128/AAC.50.1.113-120.2006.
Schwarz P, Dromer F, Lortholary O, Dannaoui E. In vitro interaction of flucytosine with conventional and new antifungals against Cryptococcus neoformans clinical isolates. Antimicrob Agents Chemother. 2003;47(10):3361–4. https://doi.org/10.1128/AAC.47.10.3361-3364.2003.
Andes D. Pharmacokinetics and pharmacodynamics of antifungals. Infect Dis Clin N Am. 2006;20(3):679–97. https://doi.org/10.1016/j.idc.2006.06.007.
Clancy CJ, Yu VL, Morris AJ, Snydman DR, Nguyen MH. Fluconazole MIC and the fluconazole dose/MIC ratio correlate with therapeutic response among patients with candidemia. Antimicrob Agents Chemother. 2005;49(8):3171–7. https://doi.org/10.1128/AAC.49.8.3171-3177.2005.
Rodriguez-Tudela JL, Almirante B, Rodriguez-Pardo D, et al. Correlation of the MIC and Dose/MIC ratio of fluconazole to the therapeutic response of patients with mucosal candidiasis and Candidemia. Antimicrob Agents Chemother. 2007;51(10):3599–604. https://doi.org/10.1128/AAC.00296-07.
Acknowledgments
We would like to thank Jane Atobe and Simone Aparecida de Souza from the laboratory group of the IIER. Molecular-type standard strains were kindly provided by the Mycology Laboratory of the Instituto Nacional de Infectologia Evandro Chagas—Fundação Oswaldo Cruz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Oscar José Chagas, Renata Buccheri, Márcia de Souza Carvalho Melhem, Walderez Szeszs, Marilena dos Anjos Martins, Lidiane de Oliveira, Rosa Marcusso and Daniel Wagner Santos declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Clinical Mycology Lab Issues
Rights and permissions
About this article
Cite this article
Chagas, O.J., Buccheri, R., de Souza Carvalho Melhem, M. et al. Usefulness of Yeast Cell Counting and Lack of Clinical Correlation of the Antifungal Susceptibility Testing Results in Management of Aids-associated Cryptococcal Meningitis. Curr Fungal Infect Rep 14, 1–8 (2020). https://doi.org/10.1007/s12281-020-00368-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-020-00368-5