Abstract
This study focused on the dosimetric impact of variations in respiratory motion during lung stereotactic body radiotherapy (SBRT). Dosimetric comparisons between volumetric modulated arc therapy (VMAT) and three-dimensional conformal radiotherapy (3DCRT) were performed using four-dimensional computed tomography (4DCT)-based internal target volumes (ITV). We created retrospective plans for ten patients with lung cancer who underwent SBRT using 3DCRT and VMAT techniques. A Delta4 Phantom + (ScandiDos, Uppsala, Sweden) was used to evaluate the dosimetric robustness of 4DCT-based ITV against variations in respiratory motion during treatment. We analyzed respiratory motion during treatment. Dose–volume histogram parameters were evaluated for the 95% dose (D95%) to the planning target volume (PTV) contoured on CT images obtained under free breathing. The correlations between patient respiratory parameters and dosimetric errors were also evaluated. In the phantom study, the average PTV D95% dose differences for all fractions were − 2.9 ± 4.4% (− 16.0 − 1.2%) and − 2.0 ± 2.8% (− 11.2 − 0.7%) for 3DCRT and VMAT, respectively. The average dose difference was < 3% for both 3DCRT and VMAT; however, in 5 out of 42 fractions in 3DCRT, the difference in PTV D95% was > 10%. Dosimetric errors were correlated with respiratory amplitude and velocity, and differences in respiratory amplitude between 4DCT and treatment days were the main factors causing dosimetric errors. The overall average dose error of the PTV D95% was small; however, both 3DCRT and VMAT cases exceeding 10% error were observed. Larger errors occurred with amplitude variation or baseline drift, indicating limited robustness of 4DCT-based ITV.



Similar content being viewed by others
References
Keall PJ, Mageras GS, Balter JM, Emery RS, Forster KM, Jiang SB, et al. The management of respiratory motion in radiation oncology report of AAPM task group 76. Med Phys. 2006;33:3874–900.
Schwarz M, Cattaneo GM, Marrazzo L. Geometrical and dosimetrical uncertainties in hypofractionated radiotherapy of the lung: a review. Phys Medica. 2017;36:126–39.
Underberg RWM, Lagerwaard FJ, Cuijpers JP, Slotman BJ, Van Sörnsen De KJR, Senan S. Four-dimensional CT scans for treatment planning in stereotactic radiotherapy for stage I lung cancer. Int J Radiat Oncol Biol Phys. 2004;60:1283–90.
Cai J, Read PW, Baisden JM, Larner JM, Benedict SH, Sheng K. Estimation of error in maximal intensity projection-based internal target volume of lung tumors: a simulation and comparison study using dynamic magnetic resonance imaging. Int J Radiat Oncol Biol Phys. 2007;69:895–902.
Purdie TG, Moseley DJ, Bissonnette JP, Sharpe MB, Franks K, Bezjak A, et al. Respiration correlated cone-beam computed tomography and 4DCT for evaluating target motion in stereotactic lung radiation therapy. Acta Oncol (Madr). 2006;45:915–22.
Steiner E, Shieh CC, Caillet V, Booth J, O’Brien R, Briggs A, et al. Both four-dimensional computed tomography and four-dimensional cone beam computed tomography under-predict lung target motion during radiotherapy. Radiother Oncol. 2019;135:65–73.
Takao S, Miyamoto N, Matsuura T, Onimaru R, Katoh N, Inoue T, et al. Intrafractional baseline shift or drift of lung tumor motion during gated radiation therapy with a real-time tumor-tracking system. Int J Radiat Oncol. 2016;94:172–80.
Leste J, Medjahed I, Arnaud FX, Ferrand R, Franceries X, Bardies M, et al. A study of the interplay effect for VMAT SBRT using a four-axes motion phantom. J Appl Clin Med Phys. 2020;21:208–15.
Wang W, Chen D, Han C, Zheng X, Zhou Y, Gong C, et al. Partial and full arc volumetric modulated arc therapy in lung cancer stereotactic body radiotherapy with different definitions of internal target volume based on 4D CT. Int J Med Phys Clin Eng Radiat Oncol. 2018;07:491–502.
Afrin KT, Ahmad S (2021) Is IMRT or VMAT superior or inferior to 3D conformal therapy in the treatment of lung cancer? A brief literature review. J Radiother Pract
Shirato H, Shimizu S, Kitamura K, Nishioka T, Kagei K, Hashimoto S, et al. Four-dimensional treatment planning and fluoroscopic real-time tumor tracking radiotherapy for moving tumor. Int J Radiat Oncol Biol Phys. 2000;48:435–42.
Shiinoki T, Onizuka R, Kawahara D, Suzuki T, Yuasa Y, Fujimoto K, et al. Estimation of patient-specific imaging dose for real-time tumour monitoring in lung patients during respiratory-gated radiotherapy. Phys Med Biol. 2018;63:2018–21.
Imura M, Yamazaki K, Shirato H, Onimaru R, Fujino M, Shimizu S, et al. Insertion and fixation of fiducial markers for setup and tracking of lung tumors in radiotherapy. Int J Radiat Oncol Biol Phys. 2005;63:1442–7.
Tanabe Y, Kiritani M, Deguchi T, Hira N, Tomimoto S. Patient-specific respiratory motion management using lung tumors vs fiducial markers for real-time tumor-tracking stereotactic body radiotherapy. Phys Imaging Radiat Oncol. 2023;25:100405.
Edvardsson A, Nordström F, Ceberg C, Ceberg S. Motion induced interplay effects for VMAT radiotherapy. Phys Med Biol. 2018;63:1–15.
Bortfeld T, Jokivarsi K, Goitein M, Kung J, Jiang SB. Effects of intra-fraction motion on IMRT dose delivery: statistical analysis and simulation. Phys Med Biol. 2002;47:2203–20.
Videtic GMM, Hu C, Singh AK, Chang JY, Parker W, Olivier KR, et al. A randomized phase 2 study comparing 2 stereotactic body radiation therapy schedules for medically inoperable patients with stage i peripheral non-small cell lung cancer: NRG oncology RTOG 0915 (NCCTG N0927). Int J Radiat Oncol Biol Phys. 2015;93:757–64.
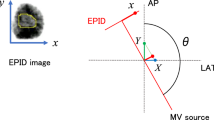
Shiinoki T, Hanazawa H, Yuasa Y, Fujimoto K, Uehara T, Shibuya K. Verification of respiratory-gated radiotherapy with new real-time tumour-tracking radiotherapy system using cine EPID images and a log file. Phys Med Biol. 2017;62:1585–99.
Kitagawa M, Hirosawa A, Takemura A. Evaluation of time delay and fluoroscopic dose in a new real-time tumor-tracking radiotherapy system. IFMBE Proc. 2019;68:487–91.
Mori S, Knopf AC, Umegaki K. Motion management in particle therapy. Med Phys. 2018;45:e994-1010.
Ernst F, Schlaefer A, Schweikard A. Smoothing of respiratory motion traces for motion-compensated radiotherapy. Med Phys. 2010;37:282–94.
Bedford JL, Lee YK, Wai P, South CP, Warrington AP. Evaluation of the Delta4 phantom for IMRT and VMAT verification. Phys Med Biol. 2009;54:167–76.
Capomolla C, Zagari A, Quarta S, De LD, Carlà A, Cazzato M, et al. 131 Performance analysis of new Delta4 Phantom+ using flattening-filter and flattening filter-free beams. Phys Medica. 2018;56:146.
Satory P, Rice A, Ng JA, Booth JT. Commissioning the Delta4 hexamotion 6d motion JIG. Eng Phys Sci Med Conf. 2013;84:2013.
Liu HH, Balter P, Tutt T, Choi B, Zhang J, Wang C, et al. Assessing respiration-induced tumor motion and internal target volume using four-dimensional computed tomography for radiotherapy of lung cancer. Int J Radiat Oncol Biol Phys. 2007;68:531–40.
Miften M, Olch A, Mihailidis D, Moran J, Pawlicki T, Molineu A, et al. Tolerance limits and methodologies for IMRT measurement-based verification QA: recommendations of AAPM Task Group No. 218. Med Phys. 2018;45:e53-83.
Menten MJ, Wetscherek A, Fast MF. MRI-guided lung SBRT: present and future developments. Phys Medica. 2017;44:139–49.
Booth J, Caillet V, Briggs A, Hardcastle N, Angelis G, Jayamanne D, et al. MLC tracking for lung SABR is feasible, efficient and delivers high-precision target dose and lower normal tissue dose. Radiother Oncol. 2021;155:131–7.
Harada K, Katoh N, Suzuki R, Ito YM, Shimizu S, Onimaru R, et al. Evaluation of the motion of lung tumors during stereotactic body radiation therapy (SBRT) with four-dimensional computed tomography (4DCT) using real-time tumor-tracking radiotherapy system (RTRT). Phys Medica. 2016;32:305–11.
Duggan DM, Ding GX, Coffey CW, Kirby W, Hallahan DE, Malcolm A, et al. Deep-inspiration breath-hold kilovoltage cone-beam CT for setup of stereotactic body radiation therapy for lung tumors: Initial experience. Lung Cancer. 2007;56:77–88.
Pokhrel D, Visak J, Critchfield LC, Stephen J, Bernard ME, Randall M, et al. Clinical validation of ring-mounted halcyon linac for lung SBRT: comparison to SBRT-dedicated C-arm linac treatments. J Appl Clin Med Phys. 2021;22:261–70.
Pokhrel D, Sanford L, Dhanireddy B, Molloy J, Randall M, McGarry RC. Flattening filter free VMAT for a stereotactic, single-dose of 30 Gy to lung lesion in a 15-min treatment slot. J Appl Clin Med Phys. 2020;21:6–12.
Ong CL, Dahele M, Slotman BJ, Verbakel WFAR. Dosimetric impact of the interplay effect during stereotactic lung radiation therapy delivery using flattening filter-free beams and volumetric modulated arc therapy. Int J Radiat Oncol Biol Phys. 2013;86:743–8.
Funding
Funding for this research was provided by a university research fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The Institutional Review Board of Juntendo University approved this retrospective study and waived the requirement for informed consent from patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Fujimoto, D., Takatsu, J., Hara, N. et al. Dosimetric comparison of four-dimensional computed tomography based internal target volume against variations in respiratory motion during treatment between volumetric modulated arc therapy and three-dimensional conformal radiotherapy in lung stereotactic body radiotherapy. Radiol Phys Technol 17, 143–152 (2024). https://doi.org/10.1007/s12194-023-00757-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-023-00757-8