Abstract
Background
Prescription medication costs increase financial burden, often leading individuals to engage in intentional nonadherence. Little is known about what specific medication cost-coping strategies individuals with arthritis employ.
Purpose
The purposes of this study are (1) to identify characteristics of individuals with arthritis who self-report prescription medication cost-coping strategies and (2) to examine the association between medication cost-coping strategies and health status.
Methods
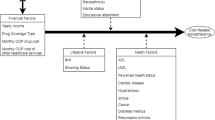
Seven hundred twenty-nine people self-reporting arthritis and prescription medication use completed a telephone survey. Adjusted regression models examined medication cost-coping strategies and five health status outcomes.
Results
Participants reported engaging in cost-coping strategies due to medication costs. Those borrowing money had worse psychosocial health and greater disability; those with increasing credit card debt reported worse physical functioning, self-rated health, and greater helplessness. Medication underuse was associated with worse psychosocial health, greater disability, and depressive symptoms.
Conclusion
Individuals with arthritis use multiple strategies to cope with medication costs, and these strategies are associated with adverse physical and psychosocial health status.

Similar content being viewed by others
References
Centers for Disease Control and Prevention (CDC). Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2003–2005. MMWR. 2006; 55(40): 1089–1092.
Abraido-Lanza AF, Revenson TA. Illness intrusion and psychological adjustment to rheumatic diseases: A social identity framework. Arthritis Rheum. 2006; 55(2): 224–232.
Katz PP, Morris A. Use of accommodations for valued life activities: Prevalence and effects on disability scores. Arthritis Care Res. 2007; 57(5): 730–737.
Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults—United States, 2005. MMWR. 2009; 58(16): 421–426.
Centers for Disease Control and Prevention (CDC). National and state medical expenditures and lost earnings attributable to arthritis and other rheumatic conditions—United States, 2003. MMWR. 2007; 56(1): 4–7.
Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007; 56(5): 1397–1407.
Cisternas MG, Murphy LB, Yelin EH, Forman AJ, Pasta DJ, Helmick CG. Trends in medical care expenditures of US adults with arthritis and other rheumatic conditions 1997 to 2005. J Rheumatol. 2009; 36(11): 2531–2538.
Dunlop DD, Manheim LM, Song J, Chang RW. Health care utilization among older adults with arthritis. Arthritis Rheum. 2003; 49(2): 164–171.
Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff. 2003; 22(4): 220–229.
Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically III adults: The treatments people forgo, how often, and who is at risk. Am J Public Health. 2004; 94(10): 1782–1787.
Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States. JAMA. 2002; 287(3): 337–344.
Stagnitti M. Trends in outpatient prescription drug utilization and expenditures, 1997 and 2004. Agency for Healthcare Research and Quality [cited 2010 Sept. 29]; April 2007. Available at http://www.meps.ahrq.gov/mepsweb/data_files/publications/st168/stat168.pdf
Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: A review of the literature. J Gen Intern Med. 2007; 22(6): 864–871.
National Center for Health Statistics. Health, United States, 2009 with Special Feature on Medical Technology. Hyattsville, Maryland: Public Health Service; 2009.
Cohen E. Ten ways to save on prescription drugs. CNNhealth com [cited 2010 May 20]. Available at http://articles.cnn.com/2009-03-19/health/ep.prescription.drug.costs_1_prescription-drugs-elderly-patients-coumadin?_s=PM:HEALTH
Sticker shock at the pharmacy counter: CR poll finds high cost of drugs leads to risky behaviors. Consumer Reports Health [cited 2010 May 20]. Available at http://www.consumerreports.org/health/prescription-drugs/sticker-shock-at-the-pharmacy-counter/overview/sticker-shock-at-the-pharmacy-counter.htm
Connolly C, Marr K. As budgets tighten, more people decide medical care can wait. The Washington Post 2008 Oct 16.
Donovan JL, Blake DR. Patient non-compliance: Deviance or reasoned decision-making? Social Sci Med. 1992; 34(5): 507–513.
Elliott RA. Poor adherence to medication in adults with rheumatoid arthritis: Reasons and solutions. Dis Manag Health Outcomes. 2008; 16(1): 13–29.
Heisler M, Wagner TH, Piette JD. Patient strategies to cope with high prescription medication costs: Who is cutting back on necessities, increasing debt, or underusing medications? J Behav Med. 2005; 28(1): 43–51.
Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004; 27(2): 384–391.
Dunlay SM, Eveleth JM, Shah ND, McNallan SM, Roger VL. Medication adherence among community-dwelling patients with heart failure. Mayo Clin Proc. 2011; 86(4): 273–281.
Zivin K, Ratliff S, Heisler MM, Langa KM, Piette JD. Factors influencing cost-related nonadherence to medication in older adults: A conceptually based approach. Value Health. 2010; 13(4): 338–345.
Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004; 42(7): 626–634.
Heisler M, Choi H, Rosen AB, Vijan S, Kabeto M, Langa KM, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: A longitudinal analysis. Med Care. 2010; 48(2): 87–94.
Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004; 42(2): 102–109.
Wilson IB, Rogers WH, Chang H, Safran DG. Cost-related skipping of medications and other treatments among Medicare beneficiaries between 1998 and 2000. J Gen Intern Med. 2005; 20(8): 715–720.
Tamblyn R, Laprise R, Hanley JA, Abrahamowicz M, Scott S, Mayo N, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001; 285(4): 421–429.
Harrold LR, Andrade SE. Medication adherence of patients with selected rheumatic conditions: A systematic review of the literature. Semin Arthritis Rheum. 2009; 38(5): 396–402.
Curkendall S, Patel V, Gleeson M, Campbell RS, Zagari M, Dubois R. Compliance with biologic therapies for rheumatoid arthritis: Do patient out of pocket payments matter? Arthritis Care Res. 2008; 59(10): 1519–1526.
Garcia Popa-Lisseanu MG, Greisinger A, Richardson M, O’Malley KJ, Janssen NM, et al. Determinants of treatment adherence in ethnically diverse, economically disadvantaged patients with rheumatic disease. J Rheumatol. 2005; 32(5): 913–919.
Sloane PD, Callahan L, Kahwati L, Mitchell CM. Development of a practice-based patient cohort for primary care research. Fam Med. 2006; 38(1): 50–57.
Centers for Disease Control and Prevention (CDC). BRFSS Arthritis Questions 1996–2010. Centers for Disease Control and Prevention [cited 2010 July 27]. Available at http://www.cdc.gov/arthritis/data_statistics/brfss_questions.htm.
Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis: National Health Interview Survey, 2002. Am J Prev Med. 2006; 30(5): 385–393.
Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005; 52(4): 1274–1282.
Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980; 23(2): 137–145.
Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: Dimensions and practical applications. Health Qual Life Outcomes 2003; I:20.
Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: A review of its history, issues, progress, and documentation. J Rheumatol. 2003; 30(1): 167–178.
Pope JE, Khanna D, Norrie D, Ouimet JM. The minimally important difference for the Health Assessment Questionnaire in rheumatoid arthritis clinical practice is smaller than in randomized controlled trials. J Rheumatol. 2009; 36(2): 254–259.
Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996; 34: 220–233.
Ware JE Jr, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston: The Health Institute, New England Medical Center; 1994.
Gandhi SK, Salmon JW, Zhao SZ, Lambert BL, Gore PR, Conrad K. Psychometric evaluation of the 12-item short-form health survey (SF-12) in osteoarthritis and rheumatoid arthritis clinical trials. Clin Ther. 2001; 23(7): 1080–1098.
Kovac SH, Mikuls TR, Mudano A, Saag KG. Health-related quality of life among self-reported arthritis sufferers: Effects of race/ethnicity and residence. Qual Life Res. 2006; 15(3): 451–460.
Centers for Disease Control and Prevention. Measuring Healthy Days: Population Assessment of Health-Related Quality of Life. Atlanta: CDC; 2000.
Moriarty DG, Kobau R, Zack MM, Zahran HS. Tracking healthy days—A window on the health of older adults. Prevent Chron Dis. 2005; 2(3): 1–8.
Mielenz T, Jackson E, Currey S, DeVellis R, Callahan LF. Psychometric properties of the Centers for Disease Control and Prevention Health-Related Quality of Life (CDC HRQOL) items in adults with arthritis. Health Qual Life Outcomes. 2006; 4: 66.
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977; 1: 385–401.
Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample. Understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. 1982; 39(10): 1195–1200.
Callahan LF, Brooks RH, Pincus T. Further analysis of learned helplessness in rheumatoid arthritis using a “Rheumatology Attitudes Index”. J Rheumatol. 1988; 15(3): 418–426.
Nicassio PM, Wallston KA, Callahan LF, Herbert M, Pincus T. The measurement of helplessness in rheumatoid arthritis. The development of the arthritis helplessness index. J Rheumatol. 1985; 12(3): 462–467.
Stein MJ, Wallston KA, Nicassio PM. Factor structure of the arthritis helplessness index. J Rheumatol. 1988; 15(3): 427–432.
DeVellis RF, Callahan LF. A brief measure of helplessness in rheumatic disease: The helplessness subscale of the Rheumatology Attitudes Index. J Rheumatol. 1993; 20(5): 866–869.
Heisler M, Wagner TH, Piette JD. Clinician identification of chronically ill patients who have problems paying for prescription medications. Am J Med. 2004; 116(11): 753–758.
Gellad WF, Haas JS, Safran DG. Race/ethnicity and nonadherence to prescription medications among seniors: Results of a national study. J Gen Intern Med. 2007; 22(11): 1572–1578.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51: 1173–1182.
MacKinnon DP. Introduction to Statistical Mediation Analyses. New York, NY: Taylor & Francis Group; 2008.
Steinman MA, Sands LP, Covinsky KE. Self-restriction of medications due to cost in seniors without prescription coverage. J Gen Intern Med. 2001; 16(12): 793–799.
Safran DG, Neuman P, Schoen C, Montgomery JE, Li W, Wilson IB et al. Prescription drug coverage and seniors: How well are states closing the gap? Health Aff 2002.
Kennedy J, Erb C. Prescription noncompliance due to cost among adults with disabilities in the United States. Am J Public Health. 2002; 92(7): 1120–1124.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med Care. 2003; 41(5): 582–592.
Hays RD, Farivar SS, Liu H. Approaches and recommendations for estimating minimally important differences for health-related quality of life measures. COPD: J Chron Obstr Pulm Dis. 2004; 2(1): 63–67.
Farivar SS, Liu H, Hays RD. Half standard deviation estimate of the minimally important difference in HRQOL scores? Expert Rev Pharmacoecon Outcomes Res. 2004; 4(5): 515–523.
Redelmeier DA, Lorig K. Assessing the clinical importance of symptomatic improvements. An illustration in rheumatology. Arch Intern Med. 1993; 153(11): 1337–1342.
Callahan LF, Martin KR, Shreffler J, Kumar D, Schoster B, Kaufman JS, et al. Independent and combined influence of homeownership, occupation, education, income and community poverty on physical health in persons with arthritis. Arthritis Care Res. 2011; 63(5): 643–653.
Chambers SA, Rahman A, Isenberg DA. Treatment adherence and clinical outcome in systemic lupus erythematosus. Rheumatology. 2007; 46(6): 895–898.
Pascual-Ramos V, Contreras-Yanez I, Villa AR, Cabiedes J, Rull-Gabayet M. Medication persistence over 2 years of follow-up in a cohort of early rheumatoid arthritis patients: Associated factors and relationship with disease activity and with disability. Arthritis Res Ther. 2009; 11(1): R26.
Rojas-Serrano J, Cardiel MH. Lupus patients in an emergency unit. Causes of consultation, hospitalization and outcome. A cohort study. Lupus. 2000; 9(8): 601–606.
Kirking DM, Lee JA, Ellis JJ, Briesacher B, Mckercher PL. Patient-reported underuse of prescription medications: A comparison of nine surveys. Med Care Res Rev. 2006; 63(4): 427–446.
Piette JD, Heisler M. Problems due to medication costs among VA and non-VA patients with chronic illnesses. Am J Manag Care. 2004; 10(11(part 2)): 861–868.
Goldman DP, Joyce GF, Escarce JJ, Pace JE, Solomon MD, Laouri M, et al. Pharmacy benefits and the use of drugs by the chronically Ill. JAMA. 2004; 291(19): 2344–2350.
Piette JD, Heisler M, Krein S, Kerr EA. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005; 165(15): 1749–1755.
Piette JD, Heisler M, Horne R, Alexander GC. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Soc Sci Med. 2006; 62(4): 846–857.
Piette JD, Heisler M, Wagner TH. Cost-related medication underuse: Do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004; 164(16): 1749–1755.
Acknowledgments
The authors thank the following participating family practices in the NC-FM-RN for their assistance: Black River Health Services, Burgaw; Bladen Medical Associates, Elizabethtown; Blair Family Medicine, Wallace; Cabarrus Family Medicine, Concord; Cabarrus Family Medicine, Harrisburg; Cabarrus Family Medicine, Kannapolis; Cabarrus Family Medicine, Mt. Pleasant; Chatham Primary Care, Siler City; Carolinas Medical Center Biddle Point, Charlotte; Carolinas Medical Center North Park, Charlotte; Community Family Practice, Asheville; Cornerstone Medical Center, Burlington; Dayspring Family Medicine, Eden; Family Practice of Summerfield, Summerfield; Goldsboro Family Physicians, Goldsboro; Henderson Family Health Center, Henderson; Orange Family Medical Group, Hillsborough; Person Family Medical Center, Roxboro; Pittsboro Family Medicine, Pittsboro; Prospect Hill Community Health Center, Prospect Hill; Robbins Family Practice, Robbins; and Village Family Medicine, Chapel Hill. Finally, we thank the individuals who willingly participated in the study.
Grant Support
This project was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Disease Multidisciplinary Clinical Research Center Rheumatic Diseases: P60-AR049465-05 and the Thurston Arthritis Research Center Training Grant 5T32-AR007416. This research was conducted while Dr. Martin was a postdoctoral research fellow at the Thurston Arthritis Research Center. She is currently a National Institute on Aging (NIA) postdoctoral research fellow, and her research is now supported in part by the Intramural Research Program of the NIA.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Martin, K.R., Shreffler, J., Schoster, B. et al. Coping with Prescription Medication Costs: a Cross-sectional Look at Strategies Used and Associations with the Physical and Psychosocial Health of Individuals with Arthritis. ann. behav. med. 44, 236–247 (2012). https://doi.org/10.1007/s12160-012-9380-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-012-9380-7