Abstract
Background
Somatostatin receptors (SSTR) represent an ideal target for nuclear theranostics applications in neuroendocrine tumors (NET). Studies suggest that high uptake on SSTR-PET is associated with response to SSTR peptide receptor radionuclide therapy (PRRT). The purpose of this study was to evaluate the role of baseline whole-body (WB) 68 Ga-DOTATATE PET/CT (SSTR-PET) quantitative parameters, and the presence of NET lesions without uptake on SSTR-PET, as outcome prognosticator in patients with NET treated with PRRT.
Methods
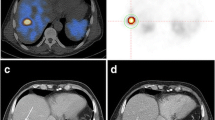
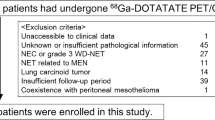
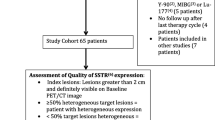
Patients with NET who underwent at least 4 177Lu-DOTATATE PRRT cycles between 07/2016 and 03/2021 were included in this retrospective analysis if they fulfilled the following inclusion criteria: SSTR-PET within 6 months of 1st PRRT cycle, follow-up CT and/or MRI performed > 6 months after the 4th cycle of PRRT. The SSTR-PET analysis consisted of a visual and a quantitative analysis done independently by two board-certified physicians. The visual analysis assessed the presence of NET lesions visible on the SSTR-PET co-registered CT. The quantitative analysis consisted in contouring all SSTR-avid lesions on SSTR-PET and extracting WB quantitative parameters: SUVmean (WB-SUVmean), SUVmax of the lesion with highest uptake (H-SUVmax), and tumor volume (WB-TV). WB-SSTR-PET parameters and the presence of SSTR-PET-negative lesions were correlated to radiologic response (assessed by RECIST 1.1 criteria) and progression-free survival (PFS). Fisher’s exact test, Mann–Whitney’s U test and Kaplan–Meier curves with Cox-regression analysis were used for the statistical analysis.
Results
Forty patients (F/M: 21/19; 34/40 with gastro-entero-pancreatic (GEP) NET, 6/40 with non-GEP NET) were included in the analysis. The median follow-up period after the 4th PRRT cycle was 25.7 months (range 15.2–59.1). Fourteen/40 (35%) patients showed radiologic response (RECIST PR). PFS event was observed in 17/40 (42.5%) patients. Thirteen/40 (32.5%) patients had SSTR-PET-negative lesions at baseline. Higher WB-SUVmean and H-SUVmax were associated with better response (p = 0.015 and 0.005, respectively). The presence of SSTR-PET-negative lesions and lower WB-SUVmean were associated with shorter PFS (p = 0.026 and 0.008, respectively).
Conclusion
Visual and quantitative analyses of baseline SSTR-PET can yield valuable information to prognosticate outcomes after 177Lu-DOTATATE PRRT.



Similar content being viewed by others
References
Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224–33.
Kvols LK, Moertel CG, O’Connell MJ, Schutt AJ, Rubin J, Hahn RG. Treatment of the malignant carcinoid syndrome. Evaluation of a long-acting somatostatin analogue. N Engl J Med. 1986;315(11):663–6.
Rinke A, Müller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656–63.
Pavel ME, Hainsworth JD, Baudin E, Peeters M, Hörsch D, Winkler RE, et al. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT-2): a randomised, placebo-controlled, phase 3 study. Lancet. 2011;378(9808):2005–12.
Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968–77.
Yao JC, Lombard-Bohas C, Baudin E, Kvols LK, Rougier P, Ruszniewski P, et al. Daily oral everolimus activity in patients with metastatic pancreatic neuroendocrine tumors after failure of cytotoxic chemotherapy: a phase II trial. J Clin Oncol. 2010;28(1):69–76.
Hope TA, Bodei L, Chan JA, El-Haddad G, Fidelman N, Kunz PL, et al. NANETS/SNMMI Consensus Statement on Patient Selection and Appropriate Use of (177)Lu-DOTATATE Peptide Receptor Radionuclide Therapy. J Nucl Med. 2020;61(2):222–7.
Hope TA, Pavel M, Bergsland EK. Neuroendocrine Tumors and Peptide Receptor Radionuclide Therapy: When Is the Right Time? J Clin Oncol. 2022;40(24):2818–29.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 Trial of (177)Lu-Dotatate for Midgut Neuroendocrine Tumors. N Engl J Med. 2017;376(2):125–35.
Hope TA, Bergsland EK, Bozkurt MF, Graham M, Heaney AP, Herrmann K, et al. Appropriate Use Criteria for Somatostatin Receptor PET Imaging in Neuroendocrine Tumors. J Nucl Med. 2018;59(1):66–74.
Kratochwil C, Stefanova M, Mavriopoulou E, Holland-Letz T, Dimitrakopoulou-Strauss A, Afshar-Oromieh A, et al. SUV of [68Ga]DOTATOC-PET/CT Predicts Response Probability of PRRT in Neuroendocrine Tumors. Mol Imaging Biol. 2015;17(3):313–8.
Öksüz M, Winter L, Pfannenberg C, Reischl G, Müssig K, Bares R, et al. Peptide receptor radionuclide therapy of neuroendocrine tumors with (90)Y-DOTATOC: is treatment response predictable by pre-therapeutic uptake of (68)Ga-DOTATOC? Diagn Interv Imaging. 2014;95(3):289–300.
Ortega C, Wong RKS, Schaefferkoetter J, Veit-Haibach P, Myrehaug S, Juergens R, et al. Quantitative (68)Ga-DOTATATE PET/CT Parameters for the Prediction of Therapy Response in Patients with Progressive Metastatic Neuroendocrine Tumors Treated with (177)Lu-DOTATATE. J Nucl Med. 2021;62(10):1406–14.
Sartor O, de Bono J, Chi KN, Fizazi K, Herrmann K, Rahbar K, et al. Lutetium-177-PSMA-617 for Metastatic Castration-Resistant Prostate Cancer. N Engl J Med. 2021;385(12):1091–103.
Hotta M, Gafita A, Czernin J, Calais J. Outcome of Patients with PSMA PET/CT Screen Failure by VISION Criteria and Treated with (177)Lu-PSMA Therapy: A Multicenter Retrospective Analysis. J Nucl Med. 2022;63(10):1484–8.
Buteau JP, Martin AJ, Emmett L, Iravani A, Sandhu S, Joshua AM, et al. PSMA and FDG-PET as predictive and prognostic biomarkers in patients given [(177)Lu]Lu-PSMA-617 versus cabazitaxel for metastatic castration-resistant prostate cancer (TheraP): a biomarker analysis from a randomised, open-label, phase 2 trial. Lancet Oncol. 2022;23(11):1389–97.
Gafita A, Calais J, Grogan TR, Hadaschik B, Wang H, Weber M, et al. Nomograms to predict outcomes after (177)Lu-PSMA therapy in men with metastatic castration-resistant prostate cancer: an international, multicentre, retrospective study. Lancet Oncol. 2021;22(8):1115–25.
Bozkurt MF, Virgolini I, Balogova S, Beheshti M, Rubello D, Decristoforo C, et al. Guideline for PET/CT imaging of neuroendocrine neoplasms with (68)Ga-DOTA-conjugated somatostatin receptor targeting peptides and (18)F-DOPA. Eur J Nucl Med Mol Imaging. 2017;44(9):1588–601.
Herrmann K, Czernin J, Wolin EM, Gupta P, Barrio M, Gutierrez A, et al. Impact of 68Ga-DOTATATE PET/CT on the management of neuroendocrine tumors: the referring physician’s perspective. J Nucl Med. 2015;56(1):70–5.
Hope TA, Allen-Auerbach M, Bodei L, Calais J, Dahlbom M, Dunnwald LK, et al. SNMMI Procedure Standard/EANM Practice Guideline for SSTR PET: Imaging Neuroendocrine Tumors. J Nucl Med. 2023;64(2):204–10.
Hope TA, Abbott A, Colucci K, Bushnell DL, Gardner L, Graham WS, et al. NANETS/SNMMI Procedure Standard for Somatostatin Receptor-Based Peptide Receptor Radionuclide Therapy with (177)Lu-DOTATATE. J Nucl Med. 2019;60(7):937–43.
Toriihara A, Baratto L, Nobashi T, Park S, Hatami N, Davidzon G, et al. Prognostic value of somatostatin receptor expressing tumor volume calculated from (68)Ga-DOTATATE PET/CT in patients with well-differentiated neuroendocrine tumors. Eur J Nucl Med Mol Imaging. 2019;46(11):2244–51.
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165(6):710–8.
Bodei L, Schöder H, Baum RP, Herrmann K, Strosberg J, Caplin M, et al. Molecular profiling of neuroendocrine tumours to predict response and toxicity to peptide receptor radionuclide therapy. Lancet Oncol. 2020;21(9):e431–43.
Binderup T, Knigge U, Johnbeck CB, Loft A, Berthelsen AK, Oturai P, et al. (18)F-FDG PET is Superior to WHO Grading as a Prognostic Tool in Neuroendocrine Neoplasms and Useful in Guiding PRRT: A Prospective 10-Year Follow-up Study. J Nucl Med. 2021;62(6):808–15.
Binderup T, Knigge U, Loft A, Federspiel B, Kjaer A. 18F-fluorodeoxyglucose positron emission tomography predicts survival of patients with neuroendocrine tumors. Clin Cancer Res. 2010;16(3):978–85.
Krenning EP, Valkema R, Kooij PP, Breeman WA, Bakker WH, deHerder WW, et al. Scintigraphy and radionuclide therapy with [indium-111-labelled-diethyl triamine penta-acetic acid-D-Phe1]-octreotide. Ital J Gastroenterol Hepatol. 1999;31(Suppl 2):S219–23.
Hope TA, Calais J, Zhang L, Dieckmann W, Millo C. (111)In-Pentetreotide Scintigraphy Versus (68)Ga-DOTATATE PET: Impact on Krenning Scores and Effect of Tumor Burden. J Nucl Med. 2019;60(9):1266–9.
Graf J, Pape UF, Jann H, Denecke T, Arsenic R, Brenner W, et al. Prognostic Significance of Somatostatin Receptor Heterogeneity in Progressive Neuroendocrine Tumor Treated with Lu-177 DOTATOC or Lu-177 DOTATATE. Eur J Nucl Med Mol Imaging. 2020;47(4):881–94.
Werner RA, Ilhan H, Lehner S, Papp L, Zsótér N, Schatka I, et al. Pre-therapy Somatostatin Receptor-Based Heterogeneity Predicts Overall Survival in Pancreatic Neuroendocrine Tumor Patients Undergoing Peptide Receptor Radionuclide Therapy. Mol Imaging Biol. 2019;21(3):582–90.
Jadvar H. The VISION Forward: Recognition and Implication of PSMA-/(18)F-FDG+ mCRPC. J Nucl Med. 2022;63(6):812–5.
Seifert R, Telli T, Hadaschik B, Fendler WP, Kuo PH, Herrmann K. Is (18)F-FDG PET Needed to Assess (177)Lu-PSMA Therapy Eligibility? A VISION-like. Single-Center Analysis J Nucl Med. 2023;64(5):731–7.
Zhang J, Liu Q, Singh A, Schuchardt C, Kulkarni HR, Baum RP. Prognostic Value of (18)F-FDG PET/CT in a Large Cohort of Patients with Advanced Metastatic Neuroendocrine Neoplasms Treated with Peptide Receptor Radionuclide Therapy. J Nucl Med. 2020;61(11):1560–9.
Beauregard JM, Hofman MS, Kong G, Hicks RJ. The tumour sink effect on the biodistribution of 68Ga-DOTA-octreotate: implications for peptide receptor radionuclide therapy. Eur J Nucl Med Mol Imaging. 2012;39(1):50–6.
Kwekkeboom DJ, Kam BL, van Essen M, Teunissen JJ, van Eijck CH, Valkema R, et al. Somatostatin-receptor-based imaging and therapy of gastroenteropancreatic neuroendocrine tumors. Endocr Relat Cancer. 2010;17(1):R53-73.
Zhang J, Kulkarni HR, Singh A, Niepsch K, Müller D, Baum RP. Peptide Receptor Radionuclide Therapy in Grade 3 Neuroendocrine Neoplasms: Safety and Survival Analysis in 69 Patients. J Nucl Med. 2019;60(3):377–85.
Carlsen EA, Fazio N, Granberg D, Grozinsky-Glasberg S, Ahmadzadehfar H, Grana CM, et al. Peptide receptor radionuclide therapy in gastroenteropancreatic NEN G3: a multicenter cohort study. Endocr Relat Cancer. 2019;26(2):227–39.
Su D, Yang H, Qiu C, Chen Y. Peptide receptor radionuclide therapy in advanced Pheochromocytomas and Paragangliomas: a systematic review and meta-analysis. Front Oncol. 2023;13:1141648.
Ma J, Hu X, Li L, Rao Z, Zhang C. Efficacy and safety of (177)Lu-DOTATATE targeted therapy in advanced/metastatic pulmonary neuroendocrine tumors: A systematic review and meta-analysis. Front Oncol. 2022;12: 993182.
Savelli G, Zaniboni A, Bertagna F, Bosio G, Nisa L, Rodella C, et al. Peptide Receptor Radionuclide Therapy (PRRT) in a Patient Affected by Metastatic Breast Cancer with Neuroendocrine Differentiation. Breast Care (Basel). 2012;7(5):408–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors report that no potential conflicts of interest relevant to this article exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hotta, M., Sonni, I., Thin, P. et al. Visual and whole-body quantitative analyses of 68 Ga-DOTATATE PET/CT for prognosis of outcome after PRRT with 177Lu-DOTATATE. Ann Nucl Med 38, 296–304 (2024). https://doi.org/10.1007/s12149-023-01899-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-023-01899-w