Abstract
Background
Mycobacterial spindle cell pseudotumor (MSCP) represents an uncommon tumor-like proliferation associated with nontuberculous mycobacterial infection, i.e., M. avium intracellulare, affecting primarily the lymph nodes of immunocompromised men in their 5th decade. Involvement of the nasal cavity by MSCP is exceedingly rare with only 3 well-documented examples in the literature.
Methods
A 74-year-old, HIV-negative, man presented with a 0.5-cm nodule of the left nasal cavity clinically presenting as a “nasal polyp.” His medical history was significant for colonic adenocarcinoma, cutaneous basal cell carcinoma, and chronic lymphocytic leukemia (CLL) transforming to B-cell prolymphocytic leukemia, responsive to chemotherapy. The patient was diagnosed with prostatic adenocarcinoma treated with radiotherapy two months before the nasal lesion was detected. No lymph node enlargement, pulmonary involvement or hepatosplenomegaly were noticed. The nasal nodule was surgically excised and histopathologically examined to rule out metastatic disease or CLL relapse.
Results
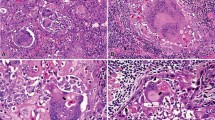
Microscopically, the lesion comprised a well-circumscribed, monotonous, spindle cell population in a vaguely storiform arrangement mixed with a heavy infiltrate of neutrophils and sparse lymphocytes. The spindle cells featured finely granular rich eosinophilic cytoplasm with rounded, oval to epithelioid, or elongated nuclei with vesicular chromatin and one or two distinct nucleoli. The lesional cells lacked overt cytologic atypia and showed occasional regular mitoses. The surface epithelium was intact or focally ulcerated. By immunohistochemistry, the spindle cell population stained strongly and diffusely for CD68 and was negative for AE1/AE3, SMA, CD34, and PSA. CD3 highlighted scattered lymphocytes. Ziehl–Neelsen stain disclosed numerous intracytoplasmic acid-fast bacilli. A diagnosis of MSCP was rendered. No recurrences were observed during a 24-month follow-up period.
Conclusion
Although exceptionally rare, MSCP should be considered in the differential diagnosis of nodular lesions of the nasal cavity that are characterized microscopically by marked spindle cell proliferation in a vague storiform pattern, admixed with a lymphocytic or mixed inflammatory infiltrate. A negative medical history for HIV infection and medication-induced immunosuppression should not preclude a diagnosis of MSCP, particularly in extranodal sites. Once the diagnosis is established, prognosis appears to be excellent for nasal MSCP following conservative surgical excision.


Similar content being viewed by others
Data Availability
The presented data are available upon request.
Code Availability
Not applicable.
References
Thompson LDR (2021) Algorithmic approach to fibroinflammatory sinonasal tract lesions. Head Neck Pathol 15:120–129
Sfeir MM, Schuetz A, Van Besien K, Borczuk AC, Soave R, Jenkins SG et al (2018) Mycobacterial spindle cell pseudotumour: epidemiology and clinical outcomes. J Clin Pathol 71:626–630
Brandwein M, Choi HS, Strauchen J, Stoler M, Jagirdar J (1990) Spindle cell reaction to nontuberculous mycobacteriosis in AIDS mimicking a spindle cell neoplasm. Evidence for dual histiocytic and fibroblast-like characteristics of spindle cells. Virchows Arch A Pathol Anat Histopathol 416:281–286
Logani S, Lucas DR, Cheng JD, Ioachim HL, Adsay NV (1999) Spindle cell tumors associated with mycobacteria in lymph nodes of HIV-positive patients: ‘Kaposi sarcoma with mycobacteria’ and ‘mycobacterial pseudotumor.’ Am J Surg Pathol 23:656–661
Gunia S, Behrens MH, Stosiek P (2005) Mycobacterial spindle cell pseudotumor (MSP) of the nasal septum clinically mimicking Kaposi’s sarcoma: case report. Rhinology 43:70–71
Ilyas S, Youssef D, Chaudhary H, Al-Abbadi MA (2011) Myocbacterium-avium intracellulare associated inflammatory pseudotumor of the anterior nasal cavity. Head Neck Pathol 5:296–301
Ohara K, Kimura T, Sakamoto K, Okada Y (2013) Nontuberculous mycobacteria-associated spindle cell pseudotumor of the nasal cavity: a case report. Pathol Int 63:266–271
Rahmani M, Alroy J, Zoukhri D, Wein RO, Tischler AS (2013) Mycobacterial pseudotumor of the skin. Virchows Arch 463:843–846
Yeh I, Evan G, Jokinen CH (2011) Cutaneous mycobacterial spindle cell pseudotumor: a potential mimic of soft tissue neoplasms. Am J Dermatopathol 33:e66–e69
McArthur JR, Kansu E, Uner A (2003) Hematology morphology forum case 2. Mycobacterial spindle-cell pseudotumor of the lymph nodes. Hematology 8:125–127
Chen KT (1992) Mycobacterial spindle cell pseudotumor of lymph nodes. Am J Surg Pathol 16:276–281
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Material preparation and data collection were performed by PPA and PEW. The first draft of the manuscript was written by PPA and reviewed by PEW.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to disclose.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Argyris, P.P., Wakely, P.E. Mycobacterial Spindle Cell Pseudotumor of the Nasal Cavity. Head and Neck Pathol 17, 782–787 (2023). https://doi.org/10.1007/s12105-023-01550-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-023-01550-0