Abstract
Objectives
To determine the screening rates and incidence of retinopathy of prematurity (ROP), and risk factors associated with ROP in very low birthweight (VLBW, <1500 g) neonates of gestation <32 wk admitted to neonatal intensive care units (NICUs) in a middle-income country.
Methods
It was a retrospective cohort study of prospectively submitted data by 44 Malaysian NICUs participating in the Malaysian National Neonatal Registry. All VLBW neonates of gestation <32 wk born in 2015–2020 and survived to discharge were included.
Results
Of 11768 survivors, 90.5% (n = 10436) had ROP screening; 16.1% (1685/10436) had ROP. ROP was significantly more common in neonates <28 wk gestation (extremely preterm, EPT) than ≥28 wk gestation (37.7% vs. 9.7%; p <0.001), and more common in those with birthweight <1000 g (extremely low birthweight, ELBW) than ≥1000 g (32.9% vs. 9.1%; p <0.001). Multiple logistic regression analysis showed that the significant independent factors associated with increased risk of ROP were ELBW, EPT, Indian ethnic group, vaginal delivery, mechanical ventilation >5 d, high frequency ventilation, total parenteral nutrition, late-onset sepsis, bronchopulmonary dysplasia, and intraventricular hemorrhage. Receiving oxygen therapy at birth was associated with significantly lower risk of ROP.
Conclusions
The incidence and severity of ROP increased with decreasing gestation and birthweight. Prolonged duration of oxygen therapy, infection, invasive respiratory support, and conditions commonly causing fluctuations of oxygenation were significant factors associated with increased risk of ROP. Receiving oxygen at birth did not increase risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinopathy of prematurity (ROP) is a condition affecting premature neonates. It results from interruption of normal neurovascular development of the retina which stimulates abnormal compensatory vascularisation following premature birth. The outcome of this neovascularisation varies from complete recovery in mild ROP, to retinal hemorrhage, scarring, detachment, and blindness [1]. ROP-related visual impairment affects the neurodevelopment, learning and quality of life of the child and poses a major social and economic burden to society [2].
In high-income countries (HICs), incidence of ROP ranged from 90% in neonates born at gestation 24 wk to <40% in those born at gestation ≥32 wk [3]. Studies from HICs identified decreasing gestational age [4, 5], decreasing birthweight [4, 5], small-for-gestational age [6], longer duration of ventilation [7] as significant risk factors associated with ROP. In low- and middle-income countries (LMICs), population studies on ROP screening, incidence and risk factors associated with ROP in neonates of gestation <32 wk are limited. To help improve long-term outcome and quality of life of these neonates in resource limited LMICs, such information is extremely important to help guide management policy to reduce the incidence and severity of this condition.
In Malaysia, since 2005 the Ministry of Health has published a clinical practice guideline (CPG) on ROP screening and management [8]. This CPG recommends screening to be “performed at 4–6 wk after birth on all neonates of birthweight <1500 g (very low birthweight, VLBW), gestational age <32 wk, or infants with an unstable clinical course; screening should continue at two- to three-week intervals until the retina is completely vascularised, or ROP has fully regressed with no signs of risk for visual loss, or progressed to a level of severity where treatment is indicated”. The present study aimed to determine the ROP screening rates, its incidence, and risk factors associated with ROP in VLBW neonates of gestation <32 wk, born and admitted to Malaysian neonatal intensive care units (NICUs) in 2015–2020, and survived to discharge.
Material and Methods
This was a retrospective observational cohort study of neonates admitted to NICUs participating in the Malaysian National Neonatal Registry (MNNR). The MNNR included prospectively collected and anonymised data in a standardised format of all VLBW neonates and those <32 wk gestation. Trained personnel collected these data and merged data of neonates who were admitted more than once. The inclusion criteria for the present study were all VLBW neonates of gestation <32 wk, born in years 2015–2020 and survived to discharge from 44 participating NICUs (which included all major public hospitals, two private hospitals, and one of three university hospitals).
Gestation (in completed weeks) were estimated by antenatal ultrasound findings, maternal last menstrual period, or the New Ballard scores [9] for neonates born to mothers with irregular period and without antenatal ultrasound. Extremely preterm (EPT) neonates were those born at gestation <28 completed weeks, and very preterm (VPT) were those born between 28-<32 completed weeks. Antenatal steroids were steroids given before birth. Outborns were neonates born in non-participating centres. Continuous positive airway pressure therapy (CPAP) commenced shortly after birth was diagnosed as early CPAP (eCPAP). Unwell neonates with positive blood culture at ≤72 h of life were diagnosed to have early-onset sepsis (EOS); those who became symptomatic with positive blood culture after 72 h of life had late-onset sepsis (LOS). Neonates with clinical and radiological features according to Bell’s stage 2 or 3 criteria were diagnosed to have necrotizing enterocolitis (NEC) [10]. Patent ductus arteriosus (PDA) was diagnosed clinically and/or by cardiac ultrasound. Intraventricular hemorrhage (IVH) was diagnosed by cranial ultrasound and severity was graded (0–4) according to Papile’s criteria [11]. Bronchopulmonary dysplasia (BPD) was diagnosed when there was continuous need for oxygen therapy from birth to beyond 36 wk gestation. ROP was diagnosed by ophthalmologists using criteria of the Malaysian CPG [8] adapted from guidelines of the Royal College of Ophthalmologists and the British Association of Perinatal Medicine [12]. Severity of ROP was graded from stages 0 to 5 (with 0 indicating no ROP and 5 indicating highest severity).
The National Medical Ethics and Research Committee of the Ministry Health of Malaysia (NMRR-05-04-168) and the National Institute of Health approved the study and waiver of informed consent (NIH.800-4/4/1 Jld.124 (34)).
The data were analysed using IBM SPSS version 28.0. Categorical variables were summarised as number and percentage, continuous variables as mean±SD, or median and interquartile range (IQR), where appropriate. For between group analysis, Chi square test was used for categorical variables and Student’s T-test or Mann-Whithey U test for continuous variables, where appropriate. Multiple logistic regression analysis was used to identify risk factors significantly associated with ROP. The following potential risk factors were selected a priori for multiple logistic regression analysis: demographic characteristics, history of exposure to oxygen therapy and antenatal steroid, EOS, LOS, and treatment procedures [modes of delivery, resuscitation procedures at birth, surfactant therapy, duration of mechanical ventilation, high frequency ventilation (HFV), total parenteral nutrition (TPN)], and clinical conditions (pneumothorax, NEC, PDA, IVH, and BPD) which were known to cause repeated episodes of oxygen fluctuation in neonates. To check for multicollinearity of independent factors, the variance inflection factors (VIF) were calculated; authors removed factors with VIF >2 before final analysis, and considered p values of <0.05 as statistically significant.
Results
There were 15128 VLBW neonates of gestation <32 wk admitted during this six-year period. Their median gestation was 29.0 wk (IQR: 27.0, 30.0), 31.4% were EPT; median birthweight was 1095 g (IQR: 880, 1290), 37.7% were ELBW; 52.8% were males. There were 63.8% Malay, 9.4% Chinese, 6.0% Indian, 13.9% Malaysians of other ethnicities, and 6.9% foreigners. Of these neonates, 77.8% (n = 11768, Supplementary Fig. S1) survived; none had major congenital malformations.
The average ROP screening rate of survivors was 90.5%, varying from 69.8% to 100% in the 44 NICUs. Six (13.6%) centers screened <80%, 20 (45.5%) centers screened between 80 to <90%, and 18 (40.9%) centers screened ≥90% of their survivors. Compared with those not screened for ROP (n = 1098, 9.5%), neonates who were screened (Table 1) had significantly lower gestation and birthweight, and lower proportions of Malays and foreigners.
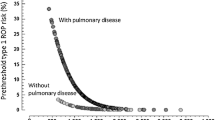
Of the 10436 neonates screened, 16.1% (n = 1685) had ROP (13.3% mild and 2.9% severe ROP). More than half were stage 1 ROP (56.3%, n = 949); 26.0% (n = 438) were stage 2, 15.0% (n = 253) were stage 3, 1.4% (n = 24) were stage 4, 0.8% (n = 13) were stage 5, and 0.5% (n = 8) had aggressive posterior ROP (APROP); Plus disease was detected in 73 neonates (26 neonates with stage 1 or 2, and 47 neonates with stage 3 or higher). More than half of neonates with ROP were EPT (54.0%, n = 910), and/or extremely low birthweight (<1000 g, ELBW) (60.5%, n = 1019). The incidence and severity of ROP increased with decreasing gestational age (Fig. 1) and deceasing birthweight (Fig. 2). Compared with VPT neonates, a significantly higher proportion of EPT neonates had all stages of ROP (37.7% vs. 9.7%, p <0.001) and severe ROP ≥stages 3 (8.6% vs. 1.1%; p <0.001). Compared with those weighing ≥1000 g, a significantly higher proportion of ELBW neonates had all stages of ROP (32.9% vs. 9.1%; p <0.001) and severe ROP ≥stages 3 (7.0% vs. 1.1%; p <0.001). Of the 1685 neonates with ROP, 239 (14.2%) received laser therapy, four (0.2%) received cryotherapy, and 17 (1.0%) had vitrectomy.
When compared with neonates without ROP (Table 2), those with ROP had significantly lower birthweight and gestation, lower proportion of ‘Malaysian of other ethnicity”, higher proportions of outborns and vaginal delivery, lower Apgar scores, lower proportions receiving oxygen and eCPAP at birth; higher proportions receiving bag-and-mask ventilation, endotracheal intubation, chest compression, adrenalin and surfactant therapy at birth; significantly lower admission body temperature; and significantly higher proportions of mechanical ventilation, HFV, TPN, EOS, LOS, pneumothorax, BPD, NEC grades ≥2, PDA and severe IVH. Neonates with ROP had significantly longer median duration of CPAP therapy [15 d (IQR: 5, 30) vs. 6 d (IQR: 2, 15), p <0.001], mechanical ventilation [8 d (IQR: 2, 22) vs. 2 d (IQR: 0.5, 6.0), p <0.001] and hospitalisation [87 d (IQR: 63, 115) vs. 54 d (IQR: 42, 73), p <0.001].
Of the 10436 neonates, 8986 (86.1%) had complete set of data of variables needed for multiple logistic regression analysis (no ROP, n = 7483, with ROP, n = 1503). After controlling for various potential confounders (Table 3), the significant independent factors associated with increased risk of ROP were ELBW, EPT, Indian ethnic group, vaginal delivery [Spontaneous vertex delivery (SVD) or breech], mechanical ventilation >5 d, HFV, TPN, LOS, BPD and IVH. Receiving oxygen therapy at birth and “Malaysian of other ethnicity” were associated with significantly lower risk. The p value of the Hosmer and Lemeshow test for this model was: 0.332; the p value of Omnibus test of model coefficient was <0.001. The area under receiver operation curve (ROC) of the regression equation is: 0.779 (95% CI: 0.765, 0.792; p <0.001).
Discussion
In this large Malaysian multicentre study of VLBW neonates of gestation <32 wk, 90.5% of survivors were screened, 16.1% had ROP, and 2.9% had severe ROP. Screening rates varied widely among NICUs. The bigger and more mature neonates had higher rate of missed screening, like study elsewhere [13].
The incidences of all stage ROP and severe ROP in Malaysian NICUs were lower than those reported in Turkey (16.1% vs. 42.0% and 2.1% vs. 11.1%) [14], Sweden (16.1% vs. 41.1%, 2.1% vs. 20.3%) [15], and Taiwan (16,1% vs. 42.5%) [16]. However, severe ROP were much more common in EPT and ELBW neonates in Malaysian NICUs than those in Australian-New Zealand network (37.7% vs. 9.6%) [4].
Besides neonatal demographic characteristics, and duration of oxygen therapy, the role of sepsis, various treatment procedures, and clinical conditions commonly causing fluctuation of oxygenation as potential risk factors associated with ROP were investigated in the present study. This is because both prolonged duration of oxygen therapy and conditions causing fluctuation of oxygenation were found to be significant risk factors in animal studies [17,18,19]. These factors were found to promote initial compromised retinal physiologic vascularity and delayed development during the first few weeks of life, and subsequent vaso-proliferation. In the present study, the results of multiple regression analysis confirmed these findings.
Unlike study elsewhere [20], PDA was only of borderline significance. Like studies elsewhere, decreasing gestational age, decreasing birthweight [2,3,4], vaginal delivery [21], TPN [16], LOS [22], IVH [23], and BPD [17] were significant independent factors associated with increased risk of ROP in present cohort. Greater fluctuation of oxygenation could be a possible mechanism for increasing risk of ROP during vaginal delivery than during LSCS.
The present study is the first to report on the effect of oxygen therapy during resuscitation at birth on ROP, and found this brief exposure was associated with significantly lower risk. The risk of ROP was significantly higher only in those receiving prolonged oxygen therapy ≥4 wk in neonates with BPD, as reported previously [16]. Unlike a large Korean neonatal network study [24], which reported mechanical ventilation longer than 2 wk was significant risk factor associated with severe ROP, the present study found ROP risk increased significantly even with shorter duration of >5 d.
Although univariate analysis in this study showed neonates with ROP had higher rates of exposure to endotracheal intubation at birth, multiple logistic regression analysis did not show statistical significance. One possible explanation was shorter duration of fluctuation of oxygenation associated with endotracheal intubation did not pose significant risk.
Both animal and clinical studies reported sepsis-associated inflammation possibly played an important role in ROP [25]. In the present study only LOS, but not EOS, was a significant independent factor associated with increased risk. One possible explanation for this discrepancy could be the small number of neonates with EOS in the present cohort which was under-powered to detect its role on ROP.
Contrary to reports elsewhere [16], SGA was not a significant independent risk factor associated with ROP in the present cohort. The authors found Indian Malaysians had significantly higher risk, and Malaysians of other ethnicity had significantly lower risk of ROP than Chinese and Malay Malaysians. These differences could be due to genetic variants, as extremely preterm neonates with variants in the intronic region of the brain-derived neurotrophic factor (BDNF) had significantly higher risk associated with ROP and severe ROP [26, 27].
Studies elsewhere reported VLBW neonates of <32 wk gestation given fish-oil-rich lipids in TPN had significantly lower risk of ROP than those given soy-based lipid in TPN [28, 29]. In the present study, TPN was a significant independent factor associated with increased risk of ROP. As the MNNR database did not capture information on types of lipids used in TPN, the authors were unsure whether failure to use fish-oil based TPN was an explanation for TPN being a factor associated with increased risk of ROP in Malaysian neonates.
The following are the strengths of this study: it is a large sample-sized multicentre national study from a LMIC; a standardised format was used to collect the data prospectively; and >90% of VLBW/<32-wk-gestation livebirths in Malaysia were admitted to the 44 participating centres during this period.
The main limitations of this study were its inability to report on the roles of other potential risk associated with ROP (including total duration of oxygen therapy, neonatal anemia [30], blood transfusion), reasons for no screening in some neonates, and information on the zone status of ROP in the affected eyes. The MNNR did not include these variables in its database.
The principal new findings in this study are short duration of oxygen exposure at birth is associated with reduced risk, while prolonged duration of exposure to oxygen, invasive respiratory support and fluctuation of oxygenation are associated with increased risk of ROP.
Based on the findings of this study, the ROP screening rates of EPT and ELBW neonates in Malaysian NICUs need further improvement as these neonates have the highest incidence and risk of severe ROP. Avoidance of vaginal delivery, use of oxygen therapy for resuscitation at birth, reduction of duration of mechanical ventilation and HFV, use of fish-oil-based lipids in TPN, and prevention of LOS, IVH and BPD are strategies which may reduce the incidence and severity of ROP in these high-risk neonates.
Data Availability
The data that support the findings of this study are available from the Malaysian National Neonatal Registry, but restrictions are applied to the availability of these data which were used under permission for the current study.
References
Harrell SN, Brandon DH. Retinopathy of prematurity: the disease process, classifications, screening, treatment, and outcome. Neonatal Netw. 2007;26:371–8.
Rahi JS, Cable N; British Childhood Visual Impairment Study Group (BCVISG). Severe visual impairment and blindness in children in the UK. Lancet. 2003;362:1359–65.
Phleps DL. Retinopathy of prematurity: history, classification, and pathophysiology. NeoReviews. 2001;2:e153–66.
Darlow BA, Hutchinson JL, Henderson-Smart DJ, Donoghue DA, Simpson JM, Evans NJ; Australian and New Zealand Neonatal Network. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics. 2005;115:990–6.
Hellstrom A, Smith LE, Dammann O. Retinopathy of prematurity. Lancet. 2013;382:1445–57.
Razak A, Faden M. Association of small for gestational age with retinopathy of prematurity: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2020;105:270–8.
Shah VA, Yeo CL, Ling YLF, Ho LY. Incidence, risk factors of retinopathy of prematurity among very low birthweight infants in Singapore. Ann Acad Med Singap. 2005;34:169–78.
Ministry of Health of Malaysia. Clinical Practice Guidelines: Retinopathy of Prematurity. 2005. Available at: http://www.moh.gov.my. Accessed on 12 Dec 2022.
Ballard JL, Khhoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard score, expanded to include extremely premature infants. J Pediatr. 1991;119:417–23.
Bell MJ, Ternberg JL, Feigin RD, et al. Necrotising enterocolitis, therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular haemorrhage: a study of infants with birth weights less than 1500gm. J Pediatr. 1978;92:529–34.
Retinopathy of prematurity: guidelines for screening and treatment. The report of a joint working party of the royal college of ophthalmologists and the British association of perinatal medicine. Early Hum Dev. 1996;46:239–58.
Bain LC, Dudley A, Gould JB, Lee HC. Factors associated with failure to screen newborns for retinopathy of prematurity. J Pediatr. 2012;161:819–23.
Bas AY, Demire N, Koc E, Isik DU, Hirfanoglu IM, Tunc T. Incidence, risk factors and severity of retinopathy of prematurity in Turkey (TR-ROP study): a prospective, multicentre study in 69 neonatal intensive care units. Br J Ophthalmol. 2018;102:1711–6.
Holmstrom G, Broberger U, Thomassen P. Neonatal risk factors for retinopathy of prematurity- a population-based study. Acta Ophthalmol Scan. 1998;76:204–7.
Li ML, Hsu SM, Chang YS, et al. Retinopathy of prematurity in southern Taiwan: a 10-year tertiary medical enter study. J Formosan Med Assoc. 2013;112:445–53.
Werdich XQ, McCollum GW, Rajaratnam VS, Penn JS. Variable oxygen and retinal VEGF levels: correlation with incidence and severity of pathology in a rat model of oxygen-induced retinopathy. Exp Eye Res. 2004;79:623–30.
York JR, Landers S, Kirby RS, Arbogast PG, Penn JS. Arterial oxygen fluctuation and retinopathy of prematurity in very-low-birth-weight infants. J Perinatol. 2004;24:82–7.
Hartnett ME, Lane RH. Effects of oxygen on the development and severity of retinopathy of prematurity. J AAPOS. 2013;17:229–34.
Sarikabadayi YU, Aydemir O, Ozen ZT, et al. Screening for retinopathy of prematurity in a large tertiary neonatal intensive care unit in Turkey: frequency and risk factors. Opthalmic Epidemiol. 2011;18:269–74.
Yau GSK, Lee JWY, Tam VTY, Liu CCL, Chu BCY, Yuen CYF. Incidence and risk factors for retinopathy of prematurity in extreme low birth weight Chinese infants. Int Opthalmol. 2015;35:365–73.
Nair PM, Ganesh A, Mitra S, Ganguly SS. Retinopathy of prematurity in VLBW and extremely LBW babies. Indian J Pediatr. 2003;70:303–6.
Procianoy RS, Garvia-Prats JA, Hittner HM, Adams JM, Rudolph AJ. An association between retinopathy of prematurity and intraventricular haemorrhage in very low birth weight infants. Acta Paediatr Scand. 1981;70:473–7.
Choi YB, Lee J, Park J, Jun YH. Impact of prolonged mechanical ventilation in very low birth weight infants: results from a national cohort study. J Pediatr. 2018;194:34–9.
Beaudry-Richard A, Nadeau-Vallee M, Prairie E, et al. Antenatal IL-1-dependent inflammation persists postnatally and causes retinal and sub-retinal vasculopathy in progeny. Sci Rep. 2018;8:11875.
Hartnett ME, Cotten CM. Genomics in the neonatal nursery: focus on ROP. Semin Perinatol. 2015;39:604–10.
Hartnett ME, Morrison MA, Smith S, et al. Genetic variants associated with severe retinopathy of prematurity in extremely low birth weight infants. Invest Ophthalmol Vis Sci. 2014;55:6194–203.
Tu CF, Lee CH, Chen HN, Tsao LY, Chen JY, Hsiao CC. Effects of fish oil-containing lipid emulsions on retinopathy of prematurity in very low birth weight infants. Pediatr Neonatol. 2020;61:224–30.
Beken S, Dilli D, Fattah ND, Kabatas EU, Zenciroglu A, Okumus N. The influence of fish-oil lipid emulsions on retinopathy of prematurity in very low birth weight infants: a randomised controlled trial. Early Hum Dev. 2014;90:27–31.
Fevireiro-Martins M, Santos AC, Marques-Neves C, Guimaraes H, Bicho M; On behalf of the GenE-Rop Study Group. Genetic modulation of the erythrocyte phenotype associated with retinopathy of prematurity- a multicenter Portuguese Cohort Study. Int J Mol Sci. 2023;24:11817.
Acknowledgements
The authors would like to thank the Director General of Ministry of Health of Malaysia for his permission to publish this paper. They would also like to thank the site coordinators of participating hospitals for contribution to the data in this study: Zuraidah Abdul Latif (Ampang Hospital), Zainah Shaikh Hedra (Sultanah Nora Ismail Hospital, Batu Pahat), Anand Mohan A/L Mohana Lal (Bintulu Hospital), Baizura Jamaluddin (Kajang Hospital), Prakash Rao A/L Rama Rao (Keningau Hospital), Siew Hong Neoh (Tunku Azizah Hospital), Hasri Hafidz (Tuanku Ampuan Najihah Hospital, Kuala Pilah), Zainab Ishak (Kulim Hospital), Poy-Lee Leow (Melaka Hospital), Chiong Hung Kiew (Miri Hospital), Mehala Devi Baskaran (Pulau Pinang Hospital), Maslina Mohamad (Putrajaya Hospital), Chee Sing Wong (Raja Permaisuri Bainun Hospital, Ipoh), Rozitah Razman (Raja Perempuan Zainab II Hospital, Kota Bharu), Maneet Kaur (Sabah Women and Children’s Hospital), Ann Cheng Wong (Sarawak General Hospital), Choo Hau Lim (Seberang Jaya Hospital), Maizatul Akmar (Serdang Hospital), Seok Chiong Chee (Selayang Hospital), Sheila Gopal Krishnan (Seri Manjung Hospital), Agnes Huei- Hwen Foo (Duchess of Kent Hospital, Sandakan), Intan Nor Chahaya Shukor (Segamat Hospital), Chae Hee Chieng (Sibu Hospital), Chong Meng Choo (Sultan Abdul Halim Hospital, Sungai Petani), Eric Boon-Kuang Ang (Sultanah Bahiyah Hospital, Alor Setar), Shiau Chuen Diong (Sultan Haji Ahmad Shah Hospital, Temerloh), Hui Ling Chow (Sultanah Aminah Hospital, Johor Bahru), Angeline Seng- Lian Wan (Sultanah Fatimah Specialist Hospital, Muar), Sharifah Huda Engku Alwi (Sultanah Nur Zahirah Hospital, Kuala Terengganu), Kwee Ching See (Sungai Buloh Hospital), Rohani Abdul Jalil (Taiping Hospital), Agnes Suganthi (Teluk Intan Hospital), Mei Ling Lee (Tengku Ampuan Afzan Hospital, Kuantan), Ee Lee Ang (Tengku Ampuan Rahimah Hospital, Klang), Abdul Nasir Mohamed Abdul Kadher (Tuanku Fauziah Hospital, Kangar), Pauline Poh-Ling Choo (Tuanku Ja'afar Hospital, Seremban), Lee Ser Chia (Sultan Ismail Hospital, Johor Bharu), Azanna Ahmad Kamar (University of Malaya Medical Center), Ananda Dharmalingam (Gleneagles Hospital Kuala Lumpur), Ismail Haron (KPJ Puteri Specialist Hospital), Sulockchana Alagan (Kluang Hospital), Noraini Ab Rahman (Kuala Krai Hospital), Nur Rashidah Mohd Zaini (Shah Alam Hospital), Noor Hayati Mohd Sharif (Slim River Hospital).
Funding
This work was supported by the Perinatal Society of Malaysia.
Author information
Authors and Affiliations
Contributions
NYB conceptualised and designed the study, analysed and interpreted the data and drafted the article; ELA, EBKA and NYB extracted and cleaned the data, critically reviewed and revised the manuscript, and approved the version to be published. NYB will act as guarantor for this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12098_2023_4997_MOESM1_ESM.docx
Supplementary Fig. S1 STROBE diagram of patient recruitment. MNNR Malaysian National Neonatal Registry, NICU Neonatal intensive care unit, ROP Retinopathy of prematurity (DOCX 261 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boo, N.Y., Ang, E.L. & Ang, E.BK. Retinopathy of Prematurity in Very Low Birthweight Neonates of Gestation Less Than 32 weeks in Malaysia. Indian J Pediatr (2024). https://doi.org/10.1007/s12098-023-04997-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12098-023-04997-9