Abstract
Background and aims
The objectives were to evaluate the role of optic nerve sheath diameter (ONSD) to detect raised intracranial pressure (ICP) in pediatric acute liver failure (PALF), study the variations in ONSD with ICP-lowering measures and to evaluate its prognostic role.
Methods
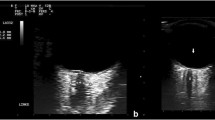
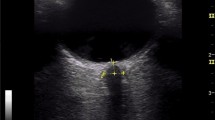
PALF with clinical evidence of raised ICP were enrolled as cases, while those without raised ICP were control group A. ONSD was measured at admission and repeated regularly. It was also measured at time of each new episode of raised ICP and 2 h after the management of such episode.
Results
31 PALF with raised ICP were included as cases and 15 without as control group A. ONSD was significantly higher in cases: 5 mm (IQR: 4.7–5.4) as compared to control group A: 3.8 mm (IQR: 3.3–4). ONSD greater than 4.55 mm at baseline diagnosed clinically raised ICP with 87.5% sensitivity and 100% specificity. The mean ONSD was 5.44 ± 0.49 mm during a total of 90 events of acute raised ICP. Clinical responders had a decrease in ONSD by 0.59 ± 0.24 mm by 2 h, whereas non-responders showed a decrease of 0.18 ± 0.23 mm, p < 0.0005. ONSD persisting more than 4.6 mm by 24 h of management predicted poor outcome with sensitivity and specificity of 83.3% and 72.7%.
Conclusion
ONSD is a simple, bedside, inexpensive, reproducible and repeatable modality to assess ongoing change in ICP in PALF. ONSD more than 4.55 mm suggests raised ICP. The goal should be to bring ONSD down to less than 4.6 mm within 24 h by aggressive anti-ICP therapy to achieve favourable outcome.
Graphical abstract





Similar content being viewed by others
Data availability
Yes, with first author.
References
Squires JE, McKiernan P, Squires RH. Acute liver failure: an update. Clin Liver Dis. 2018;22(4):773–805. https://doi.org/10.1016/j.cld.2018.06.009.
Squires RH Jr, Shneider BL, Bucuvalas J, et al. Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr. 2006;148(5):652–8. https://doi.org/10.1016/j.jpeds.2005.12.051.
Alam S, Khanna R, Sood V, Lal BB, Rawat D. Profile and outcome of first 109 cases of paediatric acute liver failure at a specialized paediatric liver unit in India. Liver Int. 2017;37:1508–14.
Rajanayagam J, Coman D, Cartwright D, Lewindon PJ. Pediatric acute liver failure: etiology, outcomes, and the role of serial pediatric end-stage liver disease scores. Pediatr Transplant. 2013;17(4):362–8. https://doi.org/10.1111/petr.12083.
Stravitz RT, Kramer AH, Davern T, et al. Intensive care of patients with acute liver failure: recommendations of the U.S. Acute liver failure study group. Crit Care Med. 2007;35(11):2498–508. https://doi.org/10.1097/01.CCM.0000287592.94554.5F.
Wendon J, Lee W. Encephalopathy and cerebral edema in the setting of acute liver failure: pathogenesis and management. Neurocrit Care. 2008;9:97.
Kamat P, Kunde S, Vos M, et al. Invasive intracranial pressure monitoring is a useful adjunct in the management of severe hepatic encephalopathy associated with pediatric acute liver failure. Pediatr Crit Care Med. 2012;13:e33.
Ng VL, Li R, Loomes KM, et al. Outcomes of children with and without hepatic encephalopathy from the pediatric acute liver failure study group. J Pediatr Gastroenterol Nutr. 2016;63:357.
Lal BB, Sood V, Snehavardhan P, Khanna R, Pasupuleti SSR, Siloliya M, Kumar G, Alam S. A novel, bedside, etiology specific prognostic model (Peds-HAV) in hepatitis A induced pediatric acute liver failure. Hepatol Int. 2020;14(4):483–90. https://doi.org/10.1007/s12072-020-10050-0.
Vaquero J, Fontana RJ, Larson AM, et al. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transpl. 2005;11(12):1581–9. https://doi.org/10.1002/lt.20625.
Robba C, Cardim D, Czosnyka M, et al. Ultrasound non-invasive intracranial pressure assessment in paediatric neurocritical care: a pilot study. Childs Nerv Syst. 2020;36(1):117–24. https://doi.org/10.1007/s00381-019-04235-8.
Kendir OT, Yilmaz HL, Ozkaya AK, et al. Determination of cerebral edema with serial measurement of optic nerve sheath diameter during treatment in children with diabetic ketoacidosis: a longitudinal study. J Pediatr Endocrinol Metab. 2019;32(9):943–9. https://doi.org/10.1515/jpem-2019-0016.
Tekin Orgun L, Atalay HT, Arhan E, Aydın K, Serdaroglu A. Optic nerve ultrasonography in monitoring treatment efficacy in pediatric idiopathic intracranial hypertension. Childs Nerv Syst. 2020. https://doi.org/10.1007/s00381-019-04497-2 (published online ahead of print, 2020 Jan 15).
Beare NA, Kampondeni S, Glover SJ, et al. Detection of raised intracranial pressure by ultrasound measurement of optic nerve sheath diameter in African children. Trop Med Int Health. 2008;13(11):1400–4. https://doi.org/10.1111/j.1365-3156.2008.02153.x.
Fontanel L, Pensiero S, Ronfani L, Rosolen V, Barbi E. Optic nerve sheath diameter ultrasound: optic nerve growth curve and its application to detect intracranial hypertension in children. Am J Ophthalmol. 2019;208:421–8. https://doi.org/10.1016/j.ajo.2019.07.014.
Moretti R, Pizzi B, Cassini F, Vivaldi N. Reliability of optic nerve ultrasound for the evaluation of patients with spontaneous intracranial hemorrhage. Neurocrit Care. 2009;11(3):406–10. https://doi.org/10.1007/s12028-009-9250-8.
Das MC, Srivastava A, Yadav RK, Yachha SK, Poddar U. Optic nerve sheath diameter in children with acute liver failure: a prospective observational pilot study. Liver Int. 2020;40(2):428–36. https://doi.org/10.1111/liv.14259.
Helmke K, Burdelski M, Hansen HC. Detection and monitoring of intracranial pressure dysregulation in liver failure by ultrasound. Transplantation. 2000;70(2):392–5. https://doi.org/10.1097/00007890-200007270-00029.
Fleming S, Thompson M, Stevens R, et al. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet. 2011;377:1011.
Flynn JT, Kaelber DC, Baker-Smith CM, AAP Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904.
Atterbury CE, Maddrey WC, Conn HO. Neomycin- sorbitol and lactulose in the treatment of acute portal- systemic encephalopathy. A controlled, double- blind clinical trial. Am J Dig Dis. 1978;23:398–406.
Stevens RD, Huff JS, Duckworth J, Papangelou A, Weingart SD, Smith WS. Emergency neurological life support: intracranial hypertension and herniation. Neurocrit Care. 2012;17(Suppl 1):S60–5. https://doi.org/10.1007/s12028-012-9754-5.
Ballantyne J, Hollman AS, Hamilton R, et al. Transorbital optic nerve sheath ultrasonography in normal children. Clin Radiol. 1999;54(11):740–2. https://doi.org/10.1016/s0009-9260(99)91176-5.
Moretti R, Pizzi B. Ultrasonography of the optic nerve in neurocritically ill patients. Acta Anaesthesiol Scand. 2011;55(6):644–52. https://doi.org/10.1111/j.1399-6576.2011.02432.x.
Kim YK, Seo H, Yu J, Hwang GS. Noninvasive estimation of raised intracranial pressure using ocular ultrasonography in liver transplant recipients with acute liver failure: a report of two cases. Korean J Anesthesiol. 2013;64(5):451–5. https://doi.org/10.4097/kjae.2013.64.5.451.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
PV, BBL, VS, RK and SA conceptualized the study and designed the protocol. PV, BBL and VS collected the data; PV and YP took ONSD measurements. BBL, PV and SA analyzed the data and formulated the initial draft. All authors read the first draft and critically reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Priti Vijay, Bikrant Bihari Lal, Vikrant Sood, Rajeev Khanna, Yashwant Patidar and Seema certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Ethics Committee of Institute of Liver and Biliary Sciences, New Delhi, India (IEC/2018/60/NA02).
Consent to participate
Informed, written consent was obtained from parents of all individual participants included in the study.
Consent for publication
Obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12072_2021_10139_MOESM5_ESM.tif
Supplementary Figure 2: Inter-observer correlation of ONSD between two observers. Abbreviations: ICC: Inter-class correlation coefficient, ONSD: Optic nerve sheath diameter, PO Primary observer, SO secondary observer (TIF 1739 KB)
Rights and permissions
About this article
Cite this article
Vijay, P., Lal, B.B., Sood, V. et al. Dynamic Optic Nerve Sheath Diameter (ONSD) guided management of raised intracranial pressure in pediatric acute liver failure. Hepatol Int 15, 502–509 (2021). https://doi.org/10.1007/s12072-021-10139-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10139-0