Abstract
Background: Sarcoidosis is an inflammatory granulomatous multisystem disease with an unknown etiology. Neurosarcoidosis is a cryptogenic neuroinflammatory manifestation of sarcoidosis. Objective: This article aims at better understanding of one of the rarer diseases whose diagnosis may be difficult leading to delay in definitive management of the patient. Method: We describe a case of neurosarcoidosis with initial presentation similar to acute invasive fungal rhinosinusitis, whose diagnosis was challenging and delayed owing to the presenting symptoms. Conclusion: The diagnosis of neurosarcoidosis becomes challenging when it presents as isolated clinical neurological symptoms. We want to highlight the variable nature of neurosarcoidosis and its consideration as diagnosis after excluding other common infectious and inflammatory conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
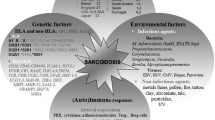
Sarcoidosis is a granulomatous inflammatory disease of unknown etiology, that typically affects young adults and involves multiple systems such as lungs, skin, and eyes. The incidence is estimated to be between 10 and 20 per 100,000 population [1].
Neurosarcoidosis is a rare entity that may cause cranial nerve palsies, aseptic meningitis, peripheral neuropathy, and myopathy, and has an incidence rate of 5–20% [2, 3]. It is pathologically characterized by the presence of non-necrotizing granulomas consisting of activated macrophages surrounded by T lymphocytes in compact clusters. Such granulomatous inflammation of the leptomeninges extends to the brain and spinal cord via Virchow-Robin spaces, which communicate with cervical lymph nodes that are thought to provide lymphatic drainage for the brain. The prominent size of these perivascular spaces at the base of the brain accounts for the preferential involvement of the basal meninges, cranial nerves, and hypothalamic-pituitary structures [4].
The diagnosis of Neurosarcoidosis has been based mainly on the clinical presentation and exclusion of other causes, since a histologic confirmation of non-caseating granulomas in the affected nervous tissue is met only in a minority of patients. A probable diagnosis can be made based on CSF studies suggesting inflammation (CSF- elevated protein, cells, immunoglobin G indices, or presence of oligoclonal bands), and on Magnetic resonance imaging (MRI) showing nervous system involvement [5].
The natural history of Neurosarcoidosis is poorly characterized due to its rarity, variability in diagnostic criteria, and the common use of corticosteroid or immunosuppressive therapy. Some of the case series observes that neurological symptoms and signs herald the diagnosis of sarcoidosis in 31–71%. In those with established sarcoidosis, neurosarcoidosis can develop years after disease onset [6, 7].
Treatment for neurosarcoidosis has been classified as a first line, second line, or third line, wherein, first line is the corticosteroid therapy, the second line involves immunosuppressive therapy [methotrexate, azathioprine, mycophenolate mofetil, cyclosporine A, or (hydroxyl) chloroquine], and finally the third line therapy with cyclophosphamide or immuno- modulatory medication [Tumor necrosis factor-alpha inhibitors (TNF-alpha) or B-cell targeted therapy] [2].
Here, we report one case of Neurosarcoidosis whose diagnosis was met with multiple challenges.
Case Report
A 36-year-old lady, with Type 2 Diabetes mellitus and hypertension and a previous history of COVID 19 infection two months before, and hospitalization (CORADS 5, CTSS 13/25), presented to our hospital with bilateral earache, right-sided facial and periorbital pain and swelling, for 10 days. On clinical examination at admission, she had bilateral facial nerve palsy [Right: Lower motor neuron (LMN) Grade IV House Brackmann (HB) grading and Left: LMN Grade III HB grading], right-sided ophthalmoplegia in all directions, decreased touch sensation(V1, V2 involvement) and right-sided Level 1b and 2 lymph nodes. No other cranial nerve involvement was noted. Diagnostic nasal endoscopy showed blackish discoloration with necrotic inferior turbinate in the right nasal cavity.
She was started on Tab Acyclovir 800 mg QID on a high suspicion of Ramsay Hunt Syndrome [8]. In the ongoing epidemic of Acute invasive.
fungal rhinosinusitis, a tissue sample from right inferior turbinate for Potassium hydroxide (KOH) mount was sent, which was reported as negative for fungal elements. Simultaneously, a nerve conduction study was performed which showed reduced CMAP of the Right facial nerve branch to Orbital oculi and Nasalis. A comparative study with the left side showed < 10% CMAP amplitude on the right side as compared to the left side. An MRI was done which showed T2 hyperintense contents filling the right maxillary sinus and enhancing soft tissue thickening with edema in the right periorbital region. Right 5th, 7th nerves and para cavernous dura were found to be enhancing. Soft tissue thickening with edema was noted in the right periorbital region and the right superior rectus muscle was bulky with inflammation in the retro-orbital fat.
With a clinical-radiological suspicion of Acute invasive fungal rhinosinusitis, the patient was started on Inj. Amphotericin B(Liposomal) 4 mg/kg and Tab Posaconazole 300 mg daily dose. A follow-up scan (Contrast-enhanced MRI) was performed 10 days after starting therapy which was also suggestive of Acute invasive fungal rhinosinusitis with a more pronounced perineural spread along right maxillary, ophthalmic and oculomotor nerves. Enhancement was also seen along the cisternal segment of the right 5th and intracanalicular segment of bilateral 7th nerves (Fig 1).
The patient showed subjective improvement in her symptoms (facial edema and pain), but no radiological improvement was noticed in the serial scans. Hence she was planned for right maxillary sinus debridement via Caldwell-Luc approach, followed by Transcutaneous retro-orbital Amphotericin B (TRAB) injections for intra-orbital involvement. Intraoperatively, polypoidal tissue and mucosal lining from the maxillary sinus were removed and sent for KOH and histopathology, both of which reported negative for fungal elements. However, antifungals were continued based on subjective improvement.
By this time, the patient had received a total of 21 days of Tab Acyclovir, eight weeks of Inj. Liposomal Amphotericin B (5130 mg) and 9400 mg of Tab Posaconazole. Although subjective improvement in the facial swelling was noted, radiological progression of the disease was noted. Having found no tissue evidence of mucormycosis from the sinonasal region and no radiological improvement in the disease progression after commencement of antifungals, a decision to look for an alternate diagnosis was made. Ultrasound-guided fine-needle aspiration cytology (FNAC ) of the right-sided neck node was done which was inconclusive. In view of polyneuritis, Angiotensin-converting enzyme (ACE) levels were checked which were found to be mildly raised- 53U/L (Normal up to 52U/L). A biopsy from the right-sided prefrontal swelling was taken (Fig 2) The site for biopsy was marked under ultrasound guidance and a tissue involving the skin and subcutaneous tissue was taken and sent for HPE which showed neural elements containing non-caseating, compact epithelioid granulomas restricted to the nerve fibers with moderate perineurial and intraneural lymphocytic inflammatory infiltrate and nerve fiber destruction and occasional multinucleated giant cells. The lymphoid cells mantling the nerves showed an admixture of CD5 positive T cells and CD79a positive B cells. After exclusion of other granulomatous diseases using special stains such as Fite Faraco for lepra bacilli, Zeihl- Nelson for Acid-fast bacilli, and Grocott’s methenamine silver and Periodic acid Schiff for fungal profiles were all negative, a diagnosis of neurosarcoidosis was made. [Insert Fig. 2. Histopathological picture of the biopsy tissue].
Discussion
Neurosarcoidosis is a rare illness, having heterogeneous clinical presentation with varying results of ancillary investigations, and considerable inter-individual differences in treatment response. It may present with cranial or peripheral neuropathy or myopathy, spinal cord inflammation, or chronic meningitis. The mortality rate among such patients is estimated to be around 5% and up to one-third of affected patients don’t show any clinical improvement on treatment even with newer modalities such as TNF alpha antagonists [5].
Here, we have discussed one of our patients whose diagnosis could only be reached through histopathological assessment of the nerves affected, despite multiple radiological and biochemical investigations over a period of two months she was admitted in our institute. Facial nerve palsy (30–40%) followed by optic neuropathy, both bilateral, is the most common neurologic manifestations reported in most patients. Less commonly, the trigeminal nerve may be affected, resulting in facial numbness or trigeminal neuralgia, which was also seen in our patient [4].
In the ongoing acute invasive fungal rhinosinusitis epidemic, a patient presenting with symptoms very similar to this infection, evaluation, and treatment was started on similar lines. The antifungals were continued considering the subjective improvement in the symptoms. The need for an alternative diagnosis was felt when radiological progression was seen in serial scans over a period of eight weeks.
None of the diagnostic modalities for neurosarcoidosis including radiological scans such as MRI, CSF and serum inflammatory markers, FDG-PET, gallium scan, and chest imaging, have been found to have good accuracy for diagnosis [5]. Similarly, clear guidance for the treatment of such patients is lacking. Most centers prescribe corticosteroids and shift to second and third-line drugs which are mainly TNF alpha antagonists.
Two scenarios have been described from a Bayesian perspective to suspect a case of neurosarcoidosis: (1) the development of a neurological problem in a patient known to have sarcoidosis and (2) a patient presenting with a neurological syndrome considered ‘typical’ for neurosarcoidosis. Also, patients with cryptogenic neuro-inflammatory disease in whom common mimics such as IgG4 – related disease and POEMS syndrome have been excluded should also be investigated for Neurosarcoidosis [9]. Another criteria describing the likelihood of this disease entity has been described by Zajicek [10].
Enhancement on contrast-enhanced magnetic resonance imaging (MRI), as evidence of break-down of the blood–brain barrier, is a highly sensitive marker of neuro-inflammatory disease. Symptomatic muscle involvement should lead to targeted biopsy. Electrophysiological studies for peripheral nerves function is recommended. Where tissue is amenable to biopsy and the risk-benefit balance is favorable, nervous system tissue biopsy is recommended to confirm the diagnosis [9].
The natural history of neurosarcoidosis is poorly defined, but spontaneous remission is recognized. Response to corticosteroids is the norm, but long-term outcomes are variable. A second-line immunosuppressant such as hydroxychloroquine, azathioprine, cyclophosphamide or methotrexate can be added. The successful use of cranial irradiation has been reported for difficult disease. As macrophage-derived TNF-alpha plays a critical role in granuloma formation, anti-TNF-alpha therapies are hypothesized to be efficacious in NS. Successful outcomes in corticosteroid-refractory NS have been reported for infliximab [9].
Conclusion
Here we report one of its kind case masquerading as acute invasive fungal rhinosinusitis. Diagnosing a rare entity as neurosarcoidosis, amidst the ongoing mucormycosis epidemic, especially when the symptoms and signs are similar to the ones seen in such affected patients, needs meticulous follow-ups and an open perspective. Symptomatic relief with routine medications leads to further difficulty in reaching the diagnosis. However, with an unbiased mind and a receptive outlook, such rare diseases can also be diagnosed and treated appropriately without much delay.
References
Thomas KW, Sarcoidosis. (2003) JAMA 289:3300
Nozaki K, Judson MA, Neurosarcoidosis (2013) Curr Treat Options Neurol 15:492–504
Segal BM (2013) Neurosarcoidosis: diagnostic approaches and therapeutic strategies. Curr Opin Neurol 26:307–313
Tavee JO, Stern BJ, Neurosarcoidosis (2014) Contin Lifelong Learn Neurol 20:545–559
Fritz D, van de Beek D, Brouwer MC (2016) Clinical features, treatment and outcome in neurosarcoidosis: systematic review and meta-analysis. BMC Neurol 16:220
Stern BJ, Krumholz A, Johns C et al (1985) Sarcoidosis and its neurological manifestations. Arch Neurol 42:909–917
Joseph FG, Scolding NJ (2009) Neurosarcoidosis: a study of 30 new cases. J Neurol Neurosurg Psychiatry 80:297–304
Syal R, Tyagi I, Goyal A (2004) Bilateral Ramsay Hunt syndrome in a diabetic patient. BMC Ear Nose Throat Disord 4:3
Ibitoye RT, Wilkins A, Scolding NJ (2017) Neurosarcoidosis: a clinical approach to diagnosis and management. J Neurol 264:1023–1028
Zajicek JP (1999) Central nervous system sarcoidosisdiagnosis and management. QJM 92:103–117
Funding
No funding received for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Consent for publication
Informed consent has been obtained from the patient for publication of the case report and accompanying images.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, P., Saxena, S., Sharma, V. et al. Neurosarcoidosis – A diagnostic challenge?. Indian J Otolaryngol Head Neck Surg 75, 2544–2547 (2023). https://doi.org/10.1007/s12070-023-03801-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03801-6