Abstract
Introduction
Otomycosis is a fungus-causing superficial infection of the external auditory canal that is common in otolaryngology practice. Though it is a worldwide infection, but is more prevalent in warm and humid regions. There has been rise in the occurrence of otomycosis in the last few years because of the extensive usage of antibiotic eardrops. Other influencing reasons for the occurrence of otomycosis is swimming, an immunocompromised host (e.g.: DM, AIDs) pregnancy, post-canal wall down mastoidectomy, tympanic membrane perforation, hearing aids and self-inflicted injuries.
Methods
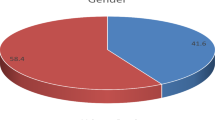
Approval from the institutional ethics committee and penned informed agreement from all patients involved in the examination were obtained. 40 patients were included in the study, starting from 1stAugust to 30th September 2021, which emphasized on otomycosis infection with central tympanic membrane perforation. Physical findings such as whitish ear discharge and the presence of hyphae in the EAC, the ear drum, the middle ear mucosa were used to diagnose otomycosis.
Result
20 patients of patched group and 20 patients of non-patched group did not visit for follow up. Data here is for patients who followed-up for 3 weeks. Any significant observation regarding statistical variation in the age, size of perforation, mycological analysis and pure tone audiometry among the two groups were not seen.
Conclusion
To conclude, we state that treatment with clotrimazole solution in patched group is safe in managing otomycosis with tympanic membrane perforation. Otomycosis is a fungus causing surface infection of the external auditory canal that otolaryngologists routinely diagnose by medical examination. In acute otomycosis, overgrowth of the fungus in the external auditory canal is due to increased humidity.


Similar content being viewed by others
References
Paulose KO, Al Khalifa S, Shenoy P, Sharma RK (1989) Mycotic infection of the ear (otomycosis): a prospective study. J Laryngol Otol 103:30–35
Pradhan B, Tuladhar NR, Amatya RM (2003) Prevalence of otomycosis in outpatient department of otolaryngology in Tribhuvan University Teaching Hospital, Kathmandu, Nepal. Ann OtolRhinolLaryngol 112:384–387
Jackman A, Ward R, April M, Bent J (2005) Topical antibiotic induced otomycosis. Int J PediatrOtorhinolaryngol 69:857–860
Kaya AD, Kiraz N (2007) In vitro susceptibilities of Aspergillus spp. causing otomycosis to amphotericin B, voriconazole and itraconazole. Mycoses 50:447–450
Araiza J, Canseco P, Bonifaz A (2006) Otomycosis: clinical and mycological study of 97 cases. Rev LaryngolOtolRhinol (Bord) 127:251–254
Ho T, Vrabec JT, Yoo D, Coker NJ (2006) Otomycosis: clinical features and treatment implications. Otolaryngol Head Neck Surg 135(5):787–791
Kurnatowski P, Filipiak A (2001) Otomycosis: prevalence, clinical symptoms, therapeutic procedure. Mycoses 44(11–12):472–479
Hurst WB (2001) Outcome of 22 cases of perforated tympanic membrane caused by otomycosis. J Laryngol Otol 115(11):879–880
Kumar KR (1984) Silent perforation of tympanic membrane and otomycosis. Indian J Otolaryngol 36(4):161–162
Viswanatha B, Sumatha D, Vijayashree MS (2012) Otomycosis in immunocompetent and immunocompromised patients: comparative study and literature review. Ear Nose Throat J 91(3):114–121
Pata YS, Oztürk C, Akbaş Y, Unal M, Görür K, Ozcan C (2004) Microbiology of cerumen in patients with recurrent otitis externa and cases with open mastoidectomy cavities. J Laryngol Otol 118:260–262
Özcan C, Ünal M, Görür K, Öztürk C, Delialioğlu N (2000) Otomycosis: a clinicomycological study and efficacy of alcohol boric solution in treatment. KBB Klinikleri 2:71–75
Song JE, Haberkamp TJ, Patel R, Redleaf MI (2014) Fungal otisis externa as a cause of tympanic membrane perforation: a case series. Ear Nose Throat J 93:332–336
Vennewald I, Klemm E (2010) Otomycosis: diagnosis and treatment. Clin Dermatol 28(2):202–211
Başal Y, Günel C, Eryılmaz A, Tuğrul I, Toka A, Kaçar F et al (2015) The effects of topical Burow’s and Castellani’s Solutions on the middle ear mucosa of rats. J Int Adv Otol 11:253–256
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh gill, G., Panchal, V. & Bakshi, R. Fungal otitis externa and tympanic membrane perforation. Indian J Otolaryngol Head Neck Surg 75 (Suppl 1), 1–5 (2023). https://doi.org/10.1007/s12070-022-03132-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03132-y