Abstract
At this moment the world is fighting with COVID-19 pandemic. Because of increasing number of critical cases, the ICU admissions are also increasing and overwhelming the hospital. These group of patients often required Tracheostomy for proper management and ventilation. As Surgeons we often required to examine and perform procedures in head and neck patients and are in high risk of exposure to aerosol and droplet contamination. We did a literature search for research regarding tracheostomy and its post procedure care during the ongoing COVID-19 pandemic. In this review various international guidelines and sources were put together, and we aim to summarize in a systematic way the available recommendations: indications, timing, technique and safety measures for tracheostomy for COVID-19 patients, from all over the world.
Similar content being viewed by others
Introduction
First described case of coronavirus was identified in the Hubei region of China in December 2019, since then Coronavirus has been spreading rapidly across countries. World Health Organization (WHO) declared the SARS-CoV-2 (COVID-19) a pandemic due to the increasing number of cases around the world on March 11th 2020. Most of the people who contracted COVID-19 presented with mild symptoms (80.9%), and according to WHO study approximately 14% patients develop severe disease [1, 2]. Patients who reach the severity of the disease and ICU requirement, the prognosis remains poor. Clinically patients affected by coronavirus shows symptoms associated with viral pneumonia, most commonly fever, cough, sore throat, myalgia, and fatigue [3,4,5]. Patients who develop severe disease are hypothesized to cause classic acute respiratory distress syndrome (ARDS) has led to the use of mechanical ventilation which is a matter of concern [6]. There are evidences that patients with mechanical ventilation have 100% mortality [7]. The timely intervention in the form of endotracheal intubation can be lifesaving but it has been seen that prolong ventilation and proper weaning can be difficult with endotracheal intubation. Hence in these patient tracheostomies becomes a necessary tool [8]. However it is an aerosol generating procedure and care must be taken to avoid contracting infection to the surgeon, critical care intensivist and other health care staffs. Surgical tracheostomy is relatively safer when done on sedated and intubated patient in ICU comparable to awake patient or percutaneous cricothyrotomy because droplet generation and air flow can be controlled [9].
Tracheostomy demand is currently increasing due to sudden spike in ICU admission with the increased need for ventilatory support as well as admission with sudden distress in the surgery emergency room. It is therefore of utmost importance to focus equally on both patient’s and health care team’s well-being during the COVID-19 pandemic that minimize risk of viral exposure. We intend to review the current guidelines and safety measures to be followed during tracheostomy in COVID-19 infected patients.
Methods
Authors performed a thorough literature review of tracheostomies in PubMed/MEDLINE, Google scholar, Scopus and Ovid Medline search using the terms tracheostomy and Coronavirus, COVID-19, SARS-CoV-2, SARS, MERS. Papers published between Jan 2000 and April 2020 were critically analysed. Specific considerations were given to timing, viral load, staff safety and technique, procedure and post-operative management of tracheostomy. Additionally, all publications referencing Coronavirus, COVID-19 and SARS-CoV-2 were screened for the similar content. All COVID-19-related guidelines published from various oto-rhino-laryngological societies was also reviewed to bring all together here.
Indication of Tracheostomy
The most important indication remains the prolonged endotracheal intubation to felicitate mechanical ventilation. There are numerous complications listed for prolonged intubation i.e. difficult weaning, fistulas etc. During COVID-19 pandemic it becomes even more important for the sudden respiratory distress caused due to thick secretion, poor effort of cough and threatened airway obstruction due to laryngeal edema [10]. Decision for tracheostomy should be taken by multidisciplinary team consisting Surgeon, Intensivist and/or Pulmonologist. The risk and benefits of the procedure to be explained to the relatives of the patient. The tracheostomy may not always be life saving as all those require the procedure may not survive but it comes at the cost of risk of infection to the health care staff and relative of the patient. Besides the challenging nature of the procedure in the COVID-19 patients, it is followed by long periods of functional dependency and rehabilitation. Selection criteria for tracheostomy are written out in Table 1 [11].
Time to tracheostomy is to be decided beforehand. American Academy of Otolaryngology-Head and Neck surgery currently recommends that tracheostomy should not be performed prior to 14 days of endotracheal intubation [12]. However there are no current guidelines regarding the optimal time of tracheostomy in COVID-19 patients but most of the European countries following local policy of 14 days before performing tracheostomy. CSO-HNS recommend against performing a tracheotomy in COVID-19 patients who are still infectious. This should only be considered if the endotracheal tube is proving insufficient to provide an adequate airway for the patients and same is also recommended by US and Canadian guidelines [12,13,14].
COVID-19 Infection Status
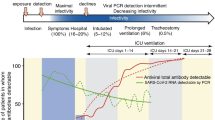
Since majority of guidelines recommend against tracheostomy in COVID-19 positive patients, the infectious status of these patients become important. Viral load in the body cannot be correlated with severity of the symptoms and vice versa [15]. Coronavirus is normally most abundant around the time of symptom onset. Once symptom occurs, viral load decreases over the following 3–4 days, this was shown in RT-PCR studies for coronavirus. Typically, lower respiratory track samples are PCR positive long after patients turn upper respiratory track sample PCR negative. Patients with severe disease has significantly higher viral RNA load which decreases more slowly than in those with mild disease [16,17,18]. Apart from all these facts one more thing to remember is a negative report should not assure that exposure risk has passed as sensitivity of the COVID-19 PCR test is around 71% [19]. Majority of country including India has limited resources in these pandemic time which precludes multiple testing in single patient. Considering all the evidences tracheostomy in COVID-19 positive patients are exception than rule and to be performed with caution.
Procedure and Staff Safety
Reducing the exposure to the health care workers is of utmost importance. All the patients should be presumed to be COVID positive and necessary precautions should always be taken. According to the present guidelines full Personal Protective Equipment (PPE) for all aerosol-generating procedures including FFP3 mask, eye protection, fluid-repellent disposable surgical gown and gloves should be used [20]. Procedure can be performed in the bedside in ICU or operation theatre however if possible the operative place should be negative pressure ventilated [21, 22]. It is a practical challenge to transfer a high risk patient from ICU to operative room and care should be taken to manage the shifting without delay and with minimal handling. Awake tracheostomy and cricothyroidotomy should be avoided as far as possible and the procedure should be performed by most experienced personal [23]. Percutaneous techniques are advanced techniques and currently no data are available to establish superiority of one approach over the other in terms of infectious transmission and safety. Single-use bronchoscopes with a sealed ventilator circuit are preferable when doing percutaneous tracheostomies.
While performing open tracheostomy the patient should be paralysed with neuromuscular blockade and neuromuscular monitoring should be done adequately. This helps in reducing cough and movements while doing the procedure. All the important drugs should be kept in the vicinity. The number of staffs inside the theatre should be minimised and every person should be clear with their role to avoid confusion inside operation theatre. This should be discussed beforehand and rehearsed. The high-volume centres performing many Tracheostomy on a regular basis are in better position to minimise overall time of procedure and risk of transmission by properly dividing their respective roles.
Non fenestrated cuffed tracheostomy tube is preferred so that cuff can be inflated adequately to avoid aerosol/air leak. Proper care should be taken to avoid injuring the cuff while doing the procedure. Procedure should be performed in bloodless field, with minimal use of diathermy and smoke buster if available. Trachea should be visualised and entry should be made under vision. Bipolar cautery is used to arrest any bleeding during the procedure. Ventilation should be paused during the entry of trachea if possible [24]. Ventilation should be resumed after checking the cuff and inflated beyond the tracheal cut with no air leak. Ideally the position of the tracheostomy tube should be confirmed with EtCo2 by the anaesthetist [25]. Initially cuffs should be inflated and pressures to be checked every 12 h, maintained at 20–30 cm H2O pressures. Tracheostomy position should also be confirmed in 30 degree head up as nursed in ICU. Some surgeons use a Broncoscope to guide the trachea but this step should be avoided as it increases the risk of aerosol exposure.
Percutaneous tracheostomy is routinely performed in most of the ICU set up across the world. However, there are no guidelines regarding the safety measures of the same. The single-stage ‘Rhino’ dilator technique is the most common percutaneous technique in the UK, and avoids multiple entries and may theoretically reduce aerosol production [26]. After confirming the position tracheostomy should be fixed with sutures and tapes. After the procedure proper doffing in dedicated area and sanitization of the theatre should be done.
Post Tracheostomy Care
Post tracheostomy care is as important as performing the procedure and one should not lower the guards just after the tracheostomy is done. Tracheostomy should be managed by experienced staff trained in management of tracheostomy inside ICU and exposure to other health care personal to be minimised [27]. Usage of closed circuit is advised at all times. Handling such as deflating the cuff and dressing should be reduced as far as possible. Tube change can be delayed to atleast 7 days [11]. Humidification and disposable inner cannula can be used to safeguard against tube occlusion from respiratory secretions, it can reduce the requirement of suctioning and cleaning [28]. A simple heat and moisture exchange (HME) filter, which provides adequate humidification and does not generate aerosols is also recommended. Sometimes the secretions are thick, so water based humidification is required but their use should be assessed on patient to patient basis. Nebulisers is helpful in secretion clearance by reducing the tenacity but require additional handling of ventilator circuits which can be avoided if possible and can waterlog HME filters; they should therefore be used only after careful consideration [29]. Above all patients inside ICU should be consulted in full PPE, facemask and shield.
Discussion
Currently both open surgical as well as percutaneous techniques are used for tracheostomy worldwide but clear advantage of one over the other is not proven. There are studies suggesting equal efficacy of both and some suggest open surgical technique is better [30,31,32,33]. In our set up and with the expertise available we prefer open surgical technique for tracheostomy in both emergency and ICU. In our experience proper staff training regarding the handling of COVID positive patients and taking care of personal protection is utmost important, full PPE, face shield, N95 mask and gloves should be used and this was suggested in other studies as well [24, 34]. The team leader’s role is understated, he should guide the team in sequential way and lead to safety of the team members. A senior consultant of head and neck surgeon should lead the way [35].
Conclusions and future directions
The number of cases are unstable till date and critically ill patients can swiftly overwhelm hospitals, particularly because many severe patients require extended periods of hospital stay with ventilator support. Among them many will require tracheostomy to facilitate recovery. There are numerous ever-changing guidelines for COVID patients which leave the health care professional to choose among wide array of management. Here in this article we try to put everything together regarding how to take care of tracheostomy patients in the COVID-19 era. While taking care of the tracheostomy patients, safety of the health care professionals is most important. There are still many grey areas as infectivity period, optimal technique of tracheostomy to reduce the aerosol production. There is continuous process of Collecting data about indications, clinical outcomes and safety for healthcare providers are ongoing for tracheostomies performed during COVID-19 outbreak, it will help building more robust evidence-based recommendations for future.
References
World Health Organization (2020) Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected. https://who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected
The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (2020) The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)-China. China CDC Weekly
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y et al (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395:507–513
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX et al (2020) Clinical characteristics of coronavirus disease 2019 in China. Engl J Med 382:1708–1720
Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J et al (2020) A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395:514–523
Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L et al (2020) COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med 46(6):1099–1102
Wang Y, Lu X, Chen H, Chen T, Su N, Huang F et al (2020) Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med 201(11):1430–1434
Vargas M, Sutherasan Y, Antonelli M, Brunetti I, Corcione A, Laffey JG et al (2015) Tracheostomy procedures in the intensive care unit: an international survey. Crit Care 19:291–301
Pichi B, Mazzola F, Bonsembiante A, Petruzzi G, Zocchi J, Moretto S et al (2020) CORONA-steps for tracheotomy in COVID-19 patients: a staff-safe method for airway management. Oral Oncol 105:104682
McGrath BA, Wallace S, Goswamy J (2020) Laryngeal oedema associated with COVID-19 complicating airway management. Anaesthesia 75(7):972
Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, Jacob T et al (2020) Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol 277(8):2173–2184
American Academy of Otolaryngology and Head and Neck Surgery (2020) AAO position statement: tracheotomy recommendations during the COVID-19 pandemic. https://www.entnet.org/content/aao-position-statement-tracheotomy-recommendations-during-covid-19-pandemic
CSO-HNS Executive Committee (2020) Guidance for health care workers performing aerosol generating medical procedures during the COVID-19 pandemic
Canadian Society of Otolaryngology-Head and Neck Surgery (2020) Recommendations from the CSO-HNS taskforce on performance of tracheotomy during the COVID-19 pandemic. https://www.entcanada.org/wp-content/uploads/COVID-19-Guidelines-CSOHNS-Task-Force-Mar-23-2020.pdf
Cereda D, Tirani M, Rovida F, Demicheli V, Ajelli M, Poletti P et al (2020) The early phase of the COVID-19 outbreak in Lombardy, Italy. Submitted 20 Mar 2020. https://arxiv.org/abs/2003.09320
Zou L, Ruan F, Huang M (2020) SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 382:1177–1179
Zhao J, Yuan Q, Wang H, Liu W, Liao X, Su Y et al (2020) Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clin Infect Dis. https://doi.org/10.2139/ssrn.3546052
Chen C, Gao G, Xu Y, Pu L, Wang Q, Wang L et al (2020) SARS-CoV-2-positive sputum and feces after conversion of pharyngeal samples in patients with COVID-19. Ann Intern Med 172(12):832–834
Bartolini A (1981) Regional arm-brain mean transit time in the diagnostic evaluation of patients with cerebral vascular disease. Stroke 12(2):241–245
Public Health England (2020) COVID-19. Guidance for infection prevention and control in healthcare settings. Version 1.1,27/3/20 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/876577/Infection_prevention_and_control_guidance_for_pandemic_coronavirus.pdf#page=27. Accessed 2 April 2020
Ti LK, Ang LS, Foong TW, Ng BSW (2020) What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anesth 67(6):756–758
Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY et al (2020) Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth 67(6):732–745
Cheung JC, Ho LT, Cheng JV, Cham EYK, Lam KN (2020) Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med 8(4):e19
Harrison L, Ramsden J, Winter S (2020) Guidance for surgical tracheostomy and tracheostomy tube change during the COVID-19 pandemic. Tracheostomy guidance during the COVID-19 pandemic. ENT UK. Royal College of Surgeons. https://www.entuk.org/tracheostomyguidance-during-covid-19-pandemic
Jacobs T (2020) Framework for open tracheostomy in COVID-19 patients. ENT UK. The Royal College of Surgeons. https://www.entuk.org/sites/default/files/files/COVID%2520tracheostomy%2520guidance_compressed.pdf
Krishnan K, Elliot SC, Mallick A (2005) The current practice of tracheostomy in the United Kingdom: a postal survey. Anaesthesia 60(4):360–364
Kelly FE, Hommers C, Jackson R, Cook TM (2013) Algorithm for management of tracheostomy emergencies on intensive care. Anaesthesia 68(2):217–219
Chan JYK, Wong EWY, Lam W (2019) Novel Coronavirus epidemic: an experience in Hong Kong. JAMA Otolaryngol Head Neck Surg. https://doi.org/10.1001/jamaoto.2020.0488
David AP, Russell MD, El-Sayed IH, Russell MS (2020) Tracheostomy guidelines developed at a large academic medical center during the COVID-19 pandemic. Head Neck 42(6):1291–1296
COVID 19: Considerations for optimum surgeon protection before, during, and after operation (2020). American College of Surgeons. https://www.facs.org/covid-19/clinical-guidance/surgeon-protection. Accessed April 2020
Schultz P, Morvan JB, Fakhry N, Morinière S, Vergez S, Lacroix C et al (2020) French consensus regarding precautions during tracheostomy and post-tracheostomy care in the context of COVID-19 pandemic. Eur Ann Otorhinolatyngol Head Neck Dis 137(3):167–169
The Australian and New Zealand Intensive Care Society (ANZICS) (2020) COVID-19 Guidelines. https://www.health.nsw.gov.au/Infectious/diseases/Documents/anzics-covid-19-guidelines.pdf. Accessed 2 April 2020
Tracheostomy Guidelines during COVID-19. (2019) Henry Ford Health System. Official copy at https://henryfordall.policystat.com/policy/7840482/
Guidance for Health Care Workers Performing Aerosol Generating Medical Procedures during the COVID-19 Pandemic—Endorsed by the CSO-HNS Executive Committee (2020). Canadian Society of Otolaryngology. https://www.entcanada.org/wp-content/uploads/Protocol-for-COVID-and-AGMP-3-iw-mailer.pdf. Accessed Mar 2020
Lim CM, Png LH, Wen SD, Wong J, Ng SY, Toh ST. Tracheotomy in the era of COVID-19 pandemic Department of Otorhinolaryngology-Head and Neck Surgery, Singapore General Hospital Guideline
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mandal, A., Nandi, S., Chhebbi, M. et al. A Systematic Review on Tracheostomy in COVID-19 Patients: Current Guidelines and Safety Measures. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 2738–2742 (2022). https://doi.org/10.1007/s12070-020-02152-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02152-w