Abstract
In the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pandemic, the physician finds difficulty in differentiating the symptoms due to cardiac disease from that of SARS-CoV-2. We would like to present one such mystified situation (hemosiderosis versus SARS-CoV-2 pneumonia) we encountered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case report
A 37-year-old female, with a known history of rheumatic mitral stenosis for the past 10 years, presented with complaints of progressive breathlessness, chest pain, and palpitation on minimal exertion.
While evaluating for surgical fitness, on computed tomography, the coronavirus disease 2019 Reporting and Data System (CO-RADS) score of 5 (Fig. 1) and chest roentgenogram (Fig. 2A) findings were suggestive of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), while reverse transcriptase-polymerase chain reaction (RT-PCR) was negative (Fig. 1). Surgery was deferred to a later date. While evaluating 15 days later, RT-PCR was still negative and both the immunoglobulin G (IgG) and immunoglobulin M (IgM) SARS-CoV-2 antibodies were also negative.
She underwent mitral valve replacement successfully. A postoperative chest roentgenogram was evident for the presence of hemosiderosis (Fig. 2B). Dissecting retrograde, we concluded that hemosiderosis with failure features was mocked with SARS-CoV-2 features.
Patchy areas of ground-glass opacity or consolidation in selected lung zones may be earlier radiological features of secondary pulmonary hemosiderosis, which may be reversible, once pulmonary venous hypertension is relieved. A study conducted in nine centers of the UK [1] revealed a higher mortality rate (24.5% vs 3.5%, p < 0.0001) and longer postoperative stay (11 days vs 6 days, p = 0.001). In this pandemic, weighing benefit versus risk, it is better to wait, when there is no concrete evidence to rule out SARS-CoV-2.
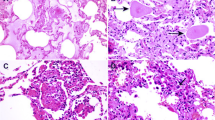
The two pulmonary conditions which have nearly a similar pattern to hemosiderosis are nonspecific interstitial pneumonitis and cryptogenic organizing pneumonia [2]. In nonspecific interstitial pneumonitis, there will be a predominant lower zone involvement and a hallmark subpleural sparing in the computed tomography (CT). In cryptogenic organizing pneumonia, the characteristic feature will be the reverse halo sign but it will be seen only in 20% of the patients. Perilobular thickening and migratory opacities are helpful differentiating features.
References
Sanders J, Akowuah E, Cooper J, et al. Cardiac surgery outcome during the COVID-19 pandemic: a retrospective review of the early experience in nine UK centres. J Cardiothorac Surg. 2021;16:43. https://doi.org/10.1186/s13019-021-01424-y.
Parekh M, Donuru A, Balasubramanya R, Kapur S. Review of the chest CT differential diagnosis of ground-glass opacities in the COVID era. Radiology. 2020;297:E289–302. https://doi.org/10.1148/radiol.2020202504.
Funding
None.
Author information
Authors and Affiliations
Contributions
Vijayanand Palanisamy—concept/drafting the article. Pradeep Ramkoomar—revision. Shilpa Shree—drafting. Mithun Sundararaaja Ravikumar—revision. All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors and that all authors are in agreement with the manuscript. All authors of this research paper have directly participated in the planning, execution, or analysis of this study.
Corresponding author
Ethics declarations
Institutional review board approval
Institutional review board approval has been obtained for the publishing of patient profile and this article.
Informed consent
Obtained to publish this report.
Statement of human and animal rights
Not Applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Palanisamy, V., Ramkoomar, P., Shree, S. et al. Pandemic created clinical eclipse: hemosiderosis versus COVID-19 pneumonia. Indian J Thorac Cardiovasc Surg 38, 218–219 (2022). https://doi.org/10.1007/s12055-021-01284-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-021-01284-0