Abstract
Background
Teleneurocritical care (TNCC) provides 24/7 virtual treatment of patients with neurological disease in the emergency department or intensive care unit. However, it is not known if TNCC is safe, effective, or associated with similar outcomes compared with in-person neurocritical care. We aim to determine the effect of daily inpatient consults from TNCC on the outcomes of patients with large vessel occlusive acute ischemic stroke treated by thrombectomy.
Methods
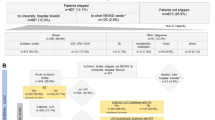
A multicenter, retrospective cohort of consecutive patients ≥ 18 years old with acute ischemic stroke from a large vessel occlusion treated by thrombectomy were identified from 2018 to 2021 within a telehealth network of an integrated not-for-profit health care system in the United States. The primary end point was good functional outcome, i.e., modified Rankin Scale 0–3, at the time of hospital discharge in patients receiving in-person neurocritical care versus TNCC.
Results
A total of 437 patients met inclusion criteria, 226 at the in-person hospital (median age 67, 53% women) and 211 at the two TNCC hospitals (median age 74, 49% women). The rate of successful endovascular therapy (modified Thrombolysis in Cerebral Infarction score 2b–3) was not different among hospitals. Good functional outcome at discharge was similar between in-person neurocritical care and TNCC (in-person 31.4% vs. TNCC 33.5%, odds ratio 0.88, 95% confidence interval 0.6–1.3; p = 0.64). Only National Institutes of Health stroke scale and age were multivariable predictors of outcome. There were no differences in mortality (9.3% vs. 13.2%, p = 0.19), intensive care unit length of stay (2.1 vs. 1.9 days, p = 0.39), or rate of symptomatic intracerebral hemorrhage (6.8% vs. 6.6%, p = 0.47) between in-person neurocritical care and TNCC.
Conclusions
Teleneurocritical care allows for equivalent favorable functional outcomes compared with in-person neurocritical care for patients with acute large vessel ischemic stroke receiving thrombectomy. The standardized protocols used by TNCC in this study, specifically the comprehensive 24/7 treatment of patients in the intensive care unit for the length of their stay, may be relevant for other health systems with limited in-person resources; however, additional study is required.


Similar content being viewed by others
References
Nguyen M, Waller M, Pandya A, Portnoy J. A review of patient and provider satisfaction with telemedicine. Curr Allergy Asthma Rep. 2020;20:72.
Harriott A, DeVita MA. The tele-ICU. Virtual Mentor. 2014;16:969–75.
Lilly CM, Cody S, Zhao H, et al. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011;305:2175–83.
Kahn JM, Rak KJ, Kuza CC, et al. Determinants of intensive care unit telemedicine effectiveness. An ethnographic study. Am J Respir Crit Care Med. 2019;199:970–9.
Kahn JM, Le TQ, Barnato AE, et al. ICU telemedicine and critical care mortality: a national effectiveness study. Med Care. 2016;54:319–25.
Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79:736–71.
Mackintosh N, Terblanche M, Maharaj R, et al. Telemedicine with clinical decision support for critical care: a systematic review. Syst Rev. 2016;5:176.
Evans NR, Sibson L, Day DJ, Agarwal S, Shekhar R, Warburton EA. Hyperacute stroke thrombolysis via telemedicine: a multicentre study of performance, safety and clinical efficacy. BMJ Open. 2022;12: e057372.
Murray NM, Hobbs K, Smith S, Puttgen A. Teleneurocritical care: lessons learned in standardizing care. Neurocrit Care. 2022;36:691–4.
Baratloo A, Rahimpour L, Abushouk AI, Safari S, Lee CW, Abdalvand A. Effects of telestroke on thrombolysis times and outcomes: a meta-analysis. Prehospital Emerg Care. 2018;22:472–84.
Demaerschalk BM, Raman R, Ernstrom K, Meyer BC. Efficacy of telemedicine for stroke: pooled analysis of the Stroke team remote evaluation using a digital observation camera (STRokE DOC) and STRokE DOC Arizona telestroke trials. Telemed J E Health. 2012;18:230–7.
Nelson RE, Saltzman GM, Skalabrin EJ, Demaerschalk BM, Majersik JJ. The cost-effectiveness of telestroke in the treatment of acute ischemic stroke. Neurology. 2011;77:1590–8.
Nelson RE, Okon N, Lesko AC, Majersik JJ, Bhatt A, Baraban E. The cost-effectiveness of telestroke in the Pacific Northwest region of the USA. J Telemed Telecare. 2016;22:413–21.
Poisson SN, Josephson SA. Quality measures in stroke. Neurohospitalist. 2011;1:71–7.
Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American heart association/American stroke association. Stroke. 2021;52:e364–7.
Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2019;50:e344-418.
Weimar C, Konig IR, Kraywinkel K, Ziegler A, Diener HC. German stroke study C. Age and National institutes of health stroke Scale score within 6 hours after onset are accurate predictors of outcome after cerebral ischemia: development and external validation of prognostic models. Stroke. 2004;35:158–62.
Konig IR, Ziegler A, Bluhmki E, et al. Predicting long-term outcome after acute ischemic stroke: a simple index works in patients from controlled clinical trials. Stroke. 2008;39:1821–6.
Koton S, Bornstein NM, Tsabari R, Tanne D, Investigators N. Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology. 2010;74:1511–6.
Schlegel D, Kolb SJ, Luciano JM, et al. Utility of the NIH stroke scale as a predictor of hospital disposition. Stroke. 2003;34:134–7.
Kim SM, Hwang SW, Oh EH, Kang JK. Determinants of the length of stay in stroke patients. Osong Public Health Res Perspect. 2013;4:329–41.
Moran JL, Nakagawa K, Asai SM, Koenig MA. 24/7 neurocritical care nurse practitioner coverage reduced door-to-needle time in stroke patients treated with tissue plasminogen activator. J Stroke Cerebrovasc Dis. 2016;25:1148–52.
Sung SF, Huang YC, Ong CT, Chen YW. A parallel thrombolysis protocol with nurse practitioners as coordinators minimized door-to-needle time for acute ischemic stroke. Stroke Res Treat. 2011;2011: 198518.
Camicia M, Lutz B, Summers D, Klassman L, Vaughn S. Nursing’s role in successful stroke care transitions across the continuum: from acute care into the community. Stroke. 2021;52:e794-805.
Ryu WS, Hong KS, Jeong SW, et al. Association of ischemic stroke onset time with presenting severity, acute progression, and long-term outcome: a cohort study. PLoS Med. 2022;19: e1003910.
Witrick B, Zhang D, Switzer JA, Hess DC, Shi L. The association between stroke mortality and time of admission and participation in a telestroke network. J Stroke Cerebrovasc Dis. 2020;29: 104480.
Wechsler LR, Demaerschalk BM, Schwamm LH, et al. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American heart association/American stroke association. Stroke. 2017;48:e3-25.
Davis TM, Barden C, Dean S, et al. American telemedicine association guidelines for TeleICU operations. Telemed J E Health. 2016;22:971–80.
Funding
There were no funding sources for this study.
Author information
Authors and Affiliations
Contributions
NMM, KH, SS, SM, DR, KT, KM, RH, and AP developed the conceptual idea for the article and edited and revised its final versions. NMM wrote and edited the initial drafts of the article. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest for any authors.
Ethical Approval
Adherence confirmed to ethical guidelines, this is an institutional review board–approved study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Murray, N.M., Marshall, S., Hoesch, R. et al. Teleneurocritical Care for Patients with Large Vessel Occlusive Ischemic Stroke Treated by Thrombectomy. Neurocrit Care 38, 650–656 (2023). https://doi.org/10.1007/s12028-022-01632-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01632-x