Abstract
Background
Cerebral autoregulation (CA) impairment is associated with neurological complications among children supported by extracorporeal membrane oxygenation (ECMO). Severe variations of arterial CO2 (PaCO2) and O2 (PaO2) tension after ECMO onset are common and associate with mortality and poor neurological outcome. The impact of gas exchange on CA among critically ill patients is poorly studied.
Methods
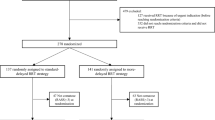
Retrospective analysis of data collected prospectively from 30 children treated with veno-arterial or veno-venous ECMO in the PICU of Nantes University Hospital, France. A correlation coefficient between the variations of regional cerebral oxygen saturation (rSO2) and the variations of mean arterial blood pressure (MAP) was calculated as an index of CA (cerebral oxygenation reactivity index, COx). Cox–MAP plots were investigated allowing determining lower limit of autoregulation (LLA) and upper limit of autoregulation (ULA) limits of autoregulation. Age-based normal blood pressure was used to adjust the MAP, LLA, and ULA data from each patient and then reported as percentage (nMAP, nLLA, and nULA, respectively). RSO2, COx, nMAP, nLLA, and nULA values were averaged over one hour before each arterial blood gas (ABG) sample during ECMO run.
Results
Thirty children (median age 4.8 months [Interquartile range (IQR) 0.7–39.1], median weight 5 kg [IQR 4–15]) experiencing 31 ECMO runs were included in the study. Three hundred and ninety ABGs were analyzed. The highest values of COx were observed on day 1 (D1) of ECMO. The relationship between COx and PaCO2 was nonlinear, but COx values tended to be lower in case of hypercapnia compared to normocapnia. During the whole ECMO run, a weak but significant correlation between PaCO2 and nULA was observed (R = 0.432, p = 0.02). On D1 of ECMO, this correlation was stronger (R = 0.85, p = 0.03) and a positive correlation between nLLA and PaCO2 was also found (R = 0.726, p < 0.001). A very weak negative correlation between PaO2 and nULA was observed within the whole ECMO run and on D1 of ECMO (R = −0.07 p = 0.04 and R = −0.135 p = <0.001, respectively). The difference between nULA and nLLA representing the span of the autoregulation plateau was positively correlated with PaCO2 and negatively correlated with PaO2 (R = 0.224, p = 0.01 and R = −0.051, p = 0.004, respectively).
Conclusions
We observed a complex relationship between PaCO2 and CA, influenced by the level of blood pressure. Hypercapnia seems to be globally protective in normotensive or hypertensive condition, while, in case of very low MAP, hypercapnia may disturb CA as it increases LLA. These data add additional arguments for very cautiously lower PaCO2, especially after ECMO start.





Similar content being viewed by others
Change history
26 April 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12028-023-01728-y
References
Dalton HJ, Reeder R, Garcia-Filion P, et al. Factors associated with bleeding and thrombosis in children receiving extracorporeal membrane oxygenation. Am J RespirCrit Care Med. 2017;196(6):762–71.
Lidegran MK, Mosskin M, Ringertz HG, et al. Cranial CT for diagnosis of intracranial complications in adult and pediatric patients during ECMO: clinical benefits in diagnosis and treatment. AcadRadiol. 2007;14(1):62–71.
Cavayas YA, Munshi L, Del Sorbo L, et al. The early change in PaCO2 after extracorporeal membrane oxygenation initiation is associated with neurological complications. Am J RespirCrit Care Med. 2020;201(12):1525–35.
Bembea MM, Lee R, Masten D, et al. Magnitude of arterial carbon dioxide change at initiation of extracorporeal membrane oxygenation support is associated with survival. J Extra CorporTechnol. 2013;45(1):26–32.
Diehl A, Burrell AJC, Udy AA, et al. Association between arterial carbon dioxide tension and clinical outcomes in venoarterial extracorporeal membrane oxygenation. Crit Care Med. 2020;48(7):977–84.
Luyt C-E, Bréchot N, Demondion P, et al. Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med. 2016;42(5):897–907.
Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev. 1990;2(2):161–92.
Rivera-Lara L, Zorrilla-Vaca A, Geocadin R, et al. Predictors of outcome with cerebral autoregulation monitoring: a systematic review and meta-analysis. Crit Care Med. 2017;45(4):695–704.
Burton VJ, Gerner G, Cristofalo E, et al. A pilot cohort study of cerebral autoregulation and 2-year neurodevelopmental outcomes in neonates with hypoxic-ischemic encephalopathy who received therapeutic hypothermia. BMC Neurol. 2015;15:209.
Lee JK, Brady KM, Chung S-E, et al. A pilot study of cerebrovascular reactivity autoregulation after pediatric cardiac arrest. Resuscitation. 2014;85(10):1387–93.
Aries MJH, Czosnyka M, Budohoski KP, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40(8):2456–63.
Ono M, Brady K, Easley RB, et al. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J Thorac Cardiovasc Surg. 2014;147(1):483–9.
Crippa IA, Subirà C, Vincent JL, et al. Impaired cerebral autoregulation is associated with brain dysfunction in patients with sepsis. Crit Care. 2018;22(1):327.
Joram N, Beqiri E, Pezzato S, et al. Continuous monitoring of cerebral autoregulation in children supported by extracorporeal membrane oxygenation: a pilot study. Neurocrit Care. 2020;8. https://doi.org/10.1007/s12028-020-01111-1.
Tian F, Morriss MC, Chalak L, et al. Impairment of cerebral autoregulation in pediatric extracorporeal membrane oxygenation associated with neuroimaging abnormalities. Neurophotonics. 2017;4(4):041410. https://doi.org/10.1117/1.NPh.4.4.041410.
Zamora CA, Oshmyansky A, Bembea M, et al. Resistive index variability in anterior cerebral artery measurements during daily transcranial duplex sonography. J Ultrasound Med. 2016;35(11):2459–65.
Busch DR, Baker WB, Mavroudis CD, et al. Noninvasive optical measurement of microvascular cerebral hemodynamics and autoregulation in the neonatal ECMO patient. Pediatr Res. 2020;88(6):925–33.
Tian F, Farhat A, Morriss MC, et al. Cerebral hemodynamic profile in ischemic and hemorrhagic brain injury acquired during pediatric extracorporeal membrane oxygenation [internet]. PediatrCrit Care Med. 2020;21(10):879–85.
Harper AM, Glass HI. Effect of alterations in the arterial carbon dioxide tension on the blood flow through the cerebral cortex at normal and low arterial blood pressures. J Neurol Neurosurg Psychiatry. 1965;28(5):449–52.
Battisti-Charbonney A, Fisher J, Duffin J. The cerebrovascular response to carbon dioxide in humans: cerebrovascular response to CO2. J Physiol. 2011;589(12):3039–48.
Yoon S, Zuccarello M, Rapoport RM. pCO2 and pH regulation of cerebral blood flow. Front Physiol. 2012;3:365.
Wyatt JS, Edwards AD, Cope M, et al. Response of cerebral blood volume to changes in arterial carbon dioxide tension in preterm and term infants. Pediatr Res. 1991;29(6):553–7.
Aaslid R, Lindegaard KF, Sorteberg W, et al. Cerebral autoregulation dynamics in humans. Stroke. 1989;20(1):45–52.
Piechnik SK, Yang X, Czosnyka M, et al. The continuous assessment of cerebrovascular reactivity: a validation of the method in healthy volunteers. AnesthAnalg. 2020;89(4):944–9.
Nusbaum DM, Brady KM, Kibler KK, et al. Acute hypercarbia increases the lower limit of cerebral blood flow autoregulation in a porcine model. Neurol Res. 2016;38(3):196–204.
Czosnyka M, Harris NG, Pickard JD, et al. CO2 cerebrovascular reactivity as a function of perfusion pressure—a modelling study. Acta Neurochir. 1993;121(3–4):159–65.
Steiner LA, Balestreri M, Johnston AJ, et al. Effects of moderate hyperventilation on cerebrovascular pressure–reactivity after head injury. Acta Neurochir Suppl. 2005;95:17–20.
Brenner M, Stein D, Hu P, et al. Association between early hyperoxia and worse outcomes after traumatic brain injury. Arch Surg. 2012;147(11):1042–6.
Ferguson LP, Durward A, Tibby SM. Relationship between arterial partial oxygen pressure after resuscitation from cardiac arrest and mortality in children. Circulation. 2012;126(3):335–42.
Cashen K, Reeder R, Dalton HJ, et al. Hyperoxia and hypocapnia during pediatric extracorporeal membrane oxygenation: associations with complications, mortality, and functional status among survivors. PediatrCrit Care Med. 2018;19(3):245–53.
Guerra-Wallace MM, Casey FL, Bell MJ, et al. Hyperoxia and hypoxia in children resuscitated from cardiac arrest. PediatrCrit Care Med. 2013;14(3):e143–8.
Bennett KS, Clark AE, Meert KL, et al. Early oxygenation and ventilation measurements after pediatric cardiac arrest: lack of association with outcome. Crit Care Med. 2013;41(6):1534–42.
Brady KM, Lee JK, Kibler KK, et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke. 2007;38(10):2818–25.
Depreitere B, Güiza F, Van den Berghe G, et al. Pressure autoregulation monitoring and cerebral perfusion pressure target recommendation in patients with severe traumatic brain injury based on minute-by-minute monitoring data. J Neurosurg. 2014;120(6):1451–7.
Liu X, Maurits NM, Aries MJH, et al. Monitoring of optimal cerebral perfusion pressure in traumatic brain injured patients using a multi-window weighting algorithm. J Neurotrauma. 2017;34(22):3081–8.
Beqiri E, Smielewski P, Robba C, et al. Feasibility of individualised severe traumatic brain injury management using an automated assessment of optimal cerebral perfusion pressure: the COGiTATE phase II study protocol [Internet]. BMJ Open. 2019;9(9):e030727.
Pejovic B, Peco-Antic A, Marinkovic-Eric J. Blood pressure in non-critically ill preterm and full-term neonates. Pediatr Nephrol. 2007;22(2):249–57.
Dionne JM, Abitbol CL, Flynn JT. Hypertension in infancy: diagnosis, management and outcome. Pediatr Nephrol. 2012;27(1):17–32.
Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904.
Donnelly J, Czosnyka M, Sudhan N, et al. Increased blood glucose is related to disturbed cerebrovascular pressure reactivity after traumatic brain injury. Neurocrit Care. 2015;22(1):20–5.
Zhang Y, Liu X, Steiner L, et al. Correlation between cerebral autoregulation and carbon dioxide reactivity in patients with traumatic brain injury. ActaNeurochirSuppl. 2016;122:205–9.
Heggen JA, Fortenberry JD, Tanner AJ, et al. Systemic hypertension associated with venovenous extracorporeal membrane oxygenation for pediatric respiratory failure. J Pediatr Surg. 2004;39(1):1626–31.
van Heijst A, Liem D, Hopman J, et al. Oxygenation and hemodynamics in left and right cerebral hemispheres during induction of veno-arterial extracorporeal membrane oxygenation. J Pediatr. 2004;144(2):223–8.
Dineen NE, Brodie FG, Robinson TG, et al. Continuous estimates of dynamic cerebral autoregulation during transient hypocapnia and hypercapnia. J Appl Physiol. 2010;108(3):604–13.
Minhas JS, Panerai RB, Robinson TG. Modelling the cerebral haemodynamic response in the physiological range of PaCO2. PhysiolMeas. 2018;39(6):065001.
Minhas JS, Panerai RB, Swienton D, et al. Feasibility of improving cerebral autoregulation in acute intracerebral hemorrhage (BREATHE-ICH) study: results from an experimental interventional study. Int J Stroke. 2020;15(6):627–37.
Klinger G, Beyene J, Shah P, Perlman M. Do hyperoxaemia and hypocapnia add to the risk of brain injury after intrapartum asphyxia? Arch Dis Child Fetal Neonatal Ed. 2005;90(1):49–52.
Perez M, Robbins ME, Revhaug C, et al. Oxygen radical disease in the newborn, revisited: oxidative stress and disease in the newborn period. Free Radic Biol Med. 2019;142:61–72.
Hayes R, Shekar K, Fraser J. Is hyperoxaemia helping or hurting patients during extracorporeal membrane oxygenation? Review of a complex problem. Perfusion. 2013;28(3):184–93.
de Jonge E, Peelen L, Keijzers PJ, et al. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care. 2008;12(6):R156.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Contributions
The study concept and design were given by NJ, PB, AC and PLL. Data acquisition was performed by NJ, EB, SP, AM, JML, AC, PB, MC and PS. Data analysis was performed by NJ, EB, MC and PS. NJ prepared the first draft of the manuscript. Interpretation of the data was done by NJ, EB, SP, AM, CR, JML, AC, PB, MC, PLL and PS. All authors provided critical feedback of the manuscript and approved the final version.
Source of Support
None.
Conflict of interest
Dr. Joram has nothing to disclose. Dr. Beqiri has nothing to disclose. Dr. Pezzato has nothing to disclose. Dr. Moscatelli has nothing to disclose. Dr. Robba has nothing to disclose. Dr. Liet has nothing to disclose. Dr. Chenouard has nothing to disclose. Dr. Bourgoin has nothing to disclose. Dr. Czosnyka reports personal fees from Cambridge Enterprise Ltd, UK, during the conduct of the study. Dr. Léger has nothing to disclose. Dr. Smielewski reports and receives part of licensing fees for the brain monitoring software ICM+ (Cambridge Enterprise Ltd, Cambridge, UK) used in this project.
Ethical Approval
The study was approved by the local Ethics Committee (Date 07/25/2018). Information of the parents was provided before inclusion. The only criterion for non-inclusion was a parental refusal.
Clinical Trial Registration
ClinicalTrials.gov (NCT04282525, February 21, 2020) https://clinicaltrials.gov/ct2/results?cond=&term=NCT04282525&cntry=&state=&city=&dist=
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original article has been updated to correct the author name Andrea Moscatelli.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joram, N., Beqiri, E., Pezzato, S. et al. Impact of Arterial Carbon Dioxide and Oxygen Content on Cerebral Autoregulation Monitoring Among Children Supported by ECMO. Neurocrit Care 35, 480–490 (2021). https://doi.org/10.1007/s12028-021-01201-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01201-8