Abstract
Background/Objective
Intracerebral hemorrhage (ICH) patients commonly have concomitant white matter lesions (WML) which may be associated with poor outcome. We studied if WML affects hematoma expansion (HE) and post-stroke functional outcome in a post hoc analysis of patients from randomized controlled trials.
Methods
In ICH patients from the clinical trials MISTIE II and CLEAR III, WML grade on diagnostic computed tomography (dCT) scan (dCT, < 24 h after ictus) was assessed using the van Swieten scale (vSS, range 0–4). The primary outcome for HE was > 33% or > 6 mL ICH volume increase from dCT to the last pre-randomization CT (< 72 h of dCT). Secondary HE outcomes were: absolute ICH expansion, > 10.4 mL total clot volume increase, and a subgroup analysis including patients with dCT < 6 h after ictus using the primary HE definition of > 33% or > 6 mL ICH volume increase. Poor functional outcome was assessed at 180 days and defined as modified Rankin Scale (mRS) ≥ 4, with ordinal mRS as a secondary endpoint.
Results
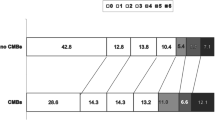
Of 635 patients, 55% had WML grade 1–4 at dCT (median 2.2 h from ictus) and 13% had subsequent HE. WML at dCT did not increase the odds for primary or secondary HE endpoints (P ≥ 0.05) after adjustment for ICH volume, intraventricular hemorrhage volume, warfarin/INR > 1.5, ictus to dCT time in hours, age, diabetes mellitus, and thalamic ICH location. WML increased the odds for having poor functional outcome (mRS ≥ 4) in univariate analyses (vSS 4; OR 4.16; 95% CI 2.54–6.83; P < 0.001) which persisted in multivariable analyses after adjustment for HE and other outcome risk factors.
Conclusions
Concomitant WML does not increase the odds for HE in patients with ICH but increases the odds for poor functional outcome.
Clinical Trial Registration
http://www.clinicaltrials.gov trial-identifiers: NCT00224770 and NCT00784134.


Similar content being viewed by others
References
Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32:891–7.
Hansen BM, Nilsson OG, Anderson H, Norrving B, Säveland H, Lindgren A. Long term (13 years) prognosis after primary intracerebral haemorrhage: a prospective population based study of long term mortality, prognostic factors and causes of death. J Neurol Neurosurg Psychiatry. 2013;84:1150–5.
Davis SM, Broderick J, Hennerici M, et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66:1175–81.
Steiner T, Diringer MN, Schneider D, et al. Dynamics of intraventricular hemorrhage in patients with spontaneous intracerebral hemorrhage: risk factors, clinical impact, and effect of hemostatic therapy with recombinant activated factor VII. Neurosurgery. 2006;59:767–73.
Brouwers HB, Chang Y, Falcone GJ, et al. Predicting hematoma expansion after primary intracerebral hemorrhage. JAMA Neurol. 2014;71:158–64.
Huynh TJ, Aviv RI, Dowlatshahi D, et al. Validation of the 9-point and 24-point hematoma expansion prediction scores and derivation of the PREDICT A/B scores. Stroke. 2015;46:3105–10.
Wang X, Arima H, Al-Shahi Salman R, et al. Clinical prediction algorithm (BRAIN) to determine risk of hematoma growth in acute intracerebral hemorrhage. Stroke. 2015;46:376–81.
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9:689–701.
Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12:822–38.
Gouw AA, Seewann A, van der Flier WM, et al. Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry. 2011;82:126–35.
Awad IA, Johnson PC, Spetzler RF, Hodak JA. Incidential subcortical lesions identified on magentic resonance imaging in the elderly. II. Postmortem pathological correlations. Stroke. 1986;17:1090–7.
Lou M, Al-Hazzani A, Goddeau RP Jr, et al. Relationship between white-matter hyperintensities and hematoma volume and growth in patients with intracerebral hemorrhage. Stroke. 2010;41:34–40.
Sykora M, Herweh C, Steiner T. The association between leukoaraiosis and poor outcome in intracerebral hemorrhage is not mediated by hematoma growth. J Stroke Cerebrovasc Dis. 2017;26:1328–33.
Morotti A, Shoamanesh A, Oliveira-Filho J, et al. White matter hyperintensities and blood pressure lowering in acute intracerebral hemorrhage: a secondary analysis of the ATACH-2 trial. Neurocrit Care. 2019. https://doi.org/10.1007/s12028-019-00761-0.
Folsom AR, Yatsuya H, Mosley TH Jr, Psaty BM, Longstreth WT Jr. Risk of intraparenchymal hemorrhage with magnetic resonance imaging-defined leukoaraiosis and brain infarcts. Ann Neurol. 2012;71:552–9.
Kim BJ, Lee SH, Ryu WS, et al. Extents of white matter lesions and increased intraventricular extension of intracerebral hemorrhage. Crit Care Med. 2013;41:1325–31.
Lee SH, Kim BJ, Ryu WS, et al. White matter lesions and poor outcome after intracerebral hemorrhage: a nationwide cohort study. Neurology. 2010;74:1502–10.
Uniken Venema SM, Marini S, Lena UK, et al. Impact of cerebral small vessel disease on functional recovery after intracerebral hemorrhage. Stroke. 2019. https://doi.org/10.1161/STROKEAHA.119.025061.
Caprio FZ, Maas MB, Rosenberg NF, et al. Leukoaraiosis on magnetic resonance imaging correlates with worse outcomes after spontaneous intracerebral hemorrhage. Stroke. 2013;44:642–6.
Sato S, Delcourt C, Heeley E, et al. Significance of cerebral small-vessel disease in acute intracerebral hemorrhage. Stroke. 2016;47:701–7.
Won YS, Chung PW, Kim YB, et al. Leukoaraiosis predicts poor outcome after spontaneous supratentorial intracerebral hemorrhage. Eur Neurol. 2010;64:253–7.
Tveiten A, Ljøstad U, Mygland Å, Naess H. Leukoaraiosis is associated with short- and long-term mortality in patients with intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2013;22:919–25.
Grips E, Sedlaczek O, Bäzner H, Fritzinger M, Daffertshofer M, Hennerici M. Supratentorial age-related white matter changes predict outcome in cerebellar stroke. Stroke. 2005;36:1988–93.
Galluzzi S, Lanni C, Pantoni L, Filippi M, Frisoni GB. White matter lesions in the elderly: pathophysiological hypothesis on the effect on brain plasticity and reserve. J Neurol Sci. 2008;273:3–9.
Hanley DF, Thompson RE, Muschelli J, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 2016;15:1228–37.
Vespa P, Hanley D, Betz J, et al. ICES (intraoperative stereotactic computed tomography-guided endoscopic surgery) for brain hemorrhage: a multicenter randomized controlled trial. Stroke. 2016;47:2749–55.
Hanley DF, Lane K, McBee N, et al. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: results of the randomised, multicentre, multiregion, placebo-controlled CLEAR III trial. Lancet. 2017;389:603–11.
van Swieten JC, Hijdra A, Koudstaal PJ, van Gijn J. Grading white matter lesions on CT and MRI: a simple scale. J Neurol Neurosurg Psychiatry. 1990;53:1080–3.
Brouwers HB, Greenberg SM. Hematoma expansion following acute intracerebral hemorrhage. Cerebrovasc Dis. 2013;35:195–201.
Rodriguez-Luna D, Boyko M, Subramaniam S, et al. Magnitude of Hematoma Volume Measurement Error in Intracerebral Hemorrhage. Stroke. 2016;47:1124–6.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the glasgow outcome scale and the extended glasgow outcome scale: guidelines for their use. J Neurotrauma. 1998;15:573–85.
Wartenberg KE, Mayer SA. Ultra-early hemostatic therapy for intracerebral hemorrhage: future directions. Front Neurol Neurosci. 2015;37:107–29.
Hansen BM, Ullman N, Norrving B, Hanley DF, Lindgren A. Applicability of clinical trials in an unselected cohort of patients with intracerebral hemorrhage. Stroke. 2016;47:2634–7.
Wahlund LO, Barkhof F, Fazekas F, et al. A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke. 2001;32:1318–22.
Venkatasubramanian C, Mlynash M, Finley-Caulfield A, et al. Natural history of perihematomal edema after intracerebral hemorrhage measured by serial magnetic resonance imaging. Stroke. 2011;42:73–80.
Acknowledgments
Funding
CLEAR III (U01NS062851) and MISTIE II (R01NS046309) were supported by Grants awarded to Dr. Hanley by the National Institutes of Health National Institute of Neurological Disorders and Stroke. Genentech donated alteplase. Dr. Hanley is supported by the National Institutes of Health (U01NS080824 and U24TR001609). Dr. Lindgren is supported by the Swedish Heart and Lung Foundation, Skåne University Hospital; the Freemasons Lodge of Instruction EOS, Lund University; and the Swedish Stroke Association. Dr. Norrving is supported by Stiftelsen Färs and Frosta Sparbank.
Author information
Authors and Affiliations
Consortia
Contributions
BMH and NU contributed to study conception and design, acquisition of data, analysis and interpretation of data, and drafting and critical revision of the manuscript. JM, RD, RA, and RET contributed to analysis and interpretation of data, and critical revisions to the manuscript. BN, IA, MZ, WCZ, and AL contributed to study conception and design, interpretation of data, and critical revisions to the manuscript. DFH contributed to study conception and design, acquisition of data, analysis and interpretation of data, and critical revision to the manuscript. All authors approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Hanley reports Grants from NIH/NINDS, non-financial support from Genentech, during the conduct of the study and personal fees from BrainScope, Neurotrope, Op2Lysis, Portola Pharmaceuticals, and medicolegal, outside the submitted work. Dr. Lindgren reports personal fees from Bayer, BMS/Pfizer, Astra Zeneca, Portola, outside the submitted work. Dr. Norrving reports personal fees for DMC work in the Navigate-ESUS trial (Bayer) and in the SOCRATES and THALES trials (Astra Zeneca). The other authors report no conflicts.
Ethical Approval
We confirm adherence to ethical guidelines and indicate ethical approvals (IRB) and use of informed consent, as appropriate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hansen, B.M., Ullman, N., Muschelli, J. et al. Relationship of White Matter Lesions with Intracerebral Hemorrhage Expansion and Functional Outcome: MISTIE II and CLEAR III. Neurocrit Care 33, 516–524 (2020). https://doi.org/10.1007/s12028-020-00916-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-00916-4