Abstract
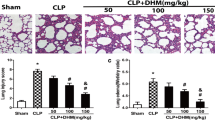
Previous reports have demonstrated that the newly identified lipid mediator protectin DX (PDX) could effectively attenuate multiple organ injuries in sepsis. The aim of our study was to clarify whether PDX could improve acute lung injury (ALI) induced by sepsis and elucidate the relevant potential mechanism. After inducing sepsis by the cecal ligation and puncture approach, mice were treated with a high or low dose of PDX. Pathological changes in the pulmonary tissue were analyzed by hematoxylin-eosin staining, and lung injury score was evaluated. Lung permeability and edema were assessed by lung wet/dry ratio, and protein and cellular load of the bronchoalveolar lavage fluid (BALF). Inflammatory cytokine levels in BALF were measured by ELISA and the expression of PPARγ in the lung tissue was analyzed by immunoblotting. The results suggested that PDX could diminish the inflammatory response in lung tissue after sepsis by upregulating PPARγ and inhibiting the phosphorylation and activation of NF-κB p65. PDX treatment lowered the levels of pro-inflammation cytokines IL-1β, IL-6, TNF-α, and MCP-1, and the levels of anti-inflammatory cytokine IL-10 was increased in the BALF. It also improved lung permeability and reduced lung injury. Furthermore, the protective effect of PDX on lung tissue could be reversed by GW9662, a specific PPAR-γ antagonist. Taken together, our study indicated that PDX could ameliorate the inflammatory response in ALI by activating the PPARγ/NF-κB pathway in a mouse model of sepsis.







Similar content being viewed by others
References
Ashbaugh D, Boyd Bigelow D, Petty T, Levine B. Acute respiratory distress in adults. Lancet. 1967;290:319–23.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800.
Acute Respiratory Distress Syndrome. JAMA. 2012; 307.
Kangelaris KN, Prakash A, Liu KD, Aouizerat B, Woodruff PG, Erle DJ, et al. Increased expression of neutrophil-related genes in patients with early sepsis-induced ARDS. Am J Physiol Lung C. 2015;308:L1102–13.
Morrell ED, Radella F II, Manicone AM, Mikacenic C, Stapleton RD, Gharib SA, et al. Peripheral and alveolar cell transcriptional programs are distinct in acute respiratory distress syndrome. Am J Resp Crit Care. 2018;197:528–32.
Bos LDJ, Scicluna BP, Ong DSY, Cremer O, van der Poll T, Schultz MJ. Understanding heterogeneity in biologic phenotypes of acute respiratory distress syndrome by leukocyte expression profiles. Am J Resp Crit Care. 2019;200:42–50.
Calfee CS, Delucchi KL, Sinha P, Matthay MA, Hackett J, Shankar-Hari M, et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018;6:691–8.
Maderna P, Godson C. Lipoxins: resolutionary road. Brit J Pharmacol. 2009;158:947–59.
Serhan CN, Chiang N. Endogenous pro-resolving and anti-inflammatory lipid mediators: a new pharmacologic genus. Br J Pharmacol. 2008;153(Suppl 1):S200–15.
Vincent J, Opal SM, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet. 2013;381:774–5.
Gong J, Wu ZY, Qi H, Chen L, Li HB, Li B, et al. Maresin 1 mitigates LPS-induced acute lung injury in mice. Brit J Pharmacol. 2014;171:3539–50.
Cao C, Yin C, Shou S, Wang J, Yu L, Li X, et al. Ulinastatin protects against LPS-induced acute lung injury by attenuating TLR4/NF-κB pathway activation and reducing inflammatory mediators. SHOCK. 2018;50:595–605.
White PJ, Mitchell PL, Schwab M, Trottier J, Kang JX, Barbier O, et al. Transgenic ω-3 PUFA enrichment alters morphology and gene expression profile in adipose tissue of obese mice: potential role for protectins. METABOLISM. 2015;64:666–76.
Korner A, et al. Resolution of inflammation and sepsis survival are improved by dietary Omega-3 fatty acids. Cell Death Differ. 2018;25:421–31.
Lagarde M, Calzada C, Guichardant M, Véricel E. Dose-effect and metabolism of docosahexaenoic acid: pathophysiological relevance in blood platelets. Prostaglandins Leukot Essent Fat Acids. 2013;88:49–52.
Liu M, Chen P, Véricel E, Lelli M, Béguin L, Lagarde M, et al. Characterization and biological effects of di-hydroxylated compounds deriving from the lipoxygenation of ALA. J Lipid Res. 2013;54:2083–94.
Liu M, Boussetta T, Makni-Maalej K, Fay M, Driss F, el-Benna J, et al. Protectin DX, a double lipoxygenase product of DHA, inhibits both ROS production in human neutrophils and cyclooxygenase activities. LIPIDS. 2014;49:49–57.
White PJ, St-Pierre P, Charbonneau A, Mitchell PL, St-Amand E, Marcotte B, et al. Protectin DX alleviates insulin resistance by activating a myokine-liver glucoregulatory axis. Nat Med. 2014;20:664–9.
Li H, Ruan XZ, Powis SH, Fernando R, Mon WY, Wheeler DC, et al. EPA and DHA reduce LPS-induced inflammation responses in HK-2 cells: evidence for a PPAR-gamma-dependent mechanism. Kidney Int. 2005;67:867–74.
D B Jump SDC. Regulation of gene expression by dietary fat. ANNU REV NUTR. 1999.
Chawla A. Nuclear receptors and lipid physiology: opening the X-files. Science. 2001;294:1866–70.
Odegaard JI, Ricardo-Gonzalez RR, Goforth MH, Morel CR, Subramanian V, Mukundan L, et al. Macrophage-specific PPARγ controls alternative activation and improves insulin resistance. NATURE. 2007;447:1116–20.
Wall R, Ross RP, Fitzgerald GF, Stanton C. Fatty acids from fish: the anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr Rev. 2010;68:280–9.
Draper E, Reynolds CM, Canavan M, Mills KH, Loscher CE, Roche HM. Omega-3 fatty acids attenuate dendritic cell function via NF-κB independent of PPARγ. J Nutr Biochem. 2011;22:784–90.
Haworth O, Levy BD. Endogenous lipid mediators in the resolution of airway inflammation. Eur Respir J. 2007;30:980–92.
Rittirsch D, Huber-Lang MS, Flierl MA, Ward PA. Immunodesign of experimental sepsis by cecal ligation and puncture. Nat Protoc. 2009;4:31–6.
Xia H, et al. Protectin DX increases survival in a mouse model of sepsis by ameliorating inflammation and modulating macrophage phenotype. Sci Rep UK. 2017;7.
Matute-Bello G, Downey G, Moore BB, Groshong SD, Matthay MA, Slutsky AS, et al. An official American Thoracic Society workshop report: features and measurements of experimental acute lung injury in animals. Am J Resp Cell Mol. 2011;44:725–38.
Boomer JS, To K, Chang KC, Takasu O, Osborne DF, Walton AH, et al. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306:2594–605.
Cohen J. The immunopathogenesis of sepsis. NATURE. 2002;420:885–91.
Abraham E, Singer M. Mechanisms of sepsis-induced organ dysfunction. Crit Care Med. 2007;35:2408–16.
Russell CD, Schwarze J. The role of pro-resolution lipid mediators in infectious disease. IMMUNOLOGY. 2014;141:166–73.
Serhan CN, Gotlinger K, Hong S, Lu Y, Siegelman J, Baer T, et al. Anti-inflammatory actions of neuroprotectin D1/protectin D1 and its natural stereoisomers: assignments of dihydroxy-containing docosatrienes. J Immunol. 2006;176:1848–59.
Liao Z, Dong J, Wu W, Yang T, Wang T, Guo L, et al. Resolvin D1 attenuates inflammation in lipopolysaccharide-induced acute lung injury through a process involving the PPARγ/NF-κB pathway. Resp Res. 2012;13:110.
Rosen ED, Spiegelman BM. PPARγ: a nuclear regulator of metabolism, differentiation, and cell growth. J Biol Chem. 2001;276:37731–4.
Straus DS, Pascual G, Li M, Welch JS, Ricote M, Hsiang CH, et al. 15-deoxy-delta 12,14-prostaglandin J2 inhibits multiple steps in the NF-kappa B signaling pathway. Proc Natl Acad Sci U S A. 2000;97:4844–9.
Rossi A, Kapahi P, Natoli G, Takahashi T, Chen Y, Karin M, et al. Anti-inflammatory cyclopentenone prostaglandins are direct inhibitors of IkappaB kinase. NATURE. 2000;403:103–8.
Ikeda J, et al. PPARγ agonists attenuate palmitate-induced ER stress through up-regulation of SCD-1 in macrophages. PLoS One. 2015;10:e128546.
Funding
This study was supported by the grants from the National Natural Science Foundation of China (No.81701887; No.81671890) and the Scientific Research Projects of Hubei Education Department (B2016081).
Author information
Authors and Affiliations
Contributions
Haifa Xia and Yangyang Geng wrote this article and performed the experiments. Fuquan Wang, Jingxu Wang, Shiqian Huang, and Ming Chen established the animal models and collected samples. Yu Ming, Zhouyang Wu, and Shujun Sun analyzed the data and prepared the figures. Weimin Xiao and Shanglong Yao designed the experiments and revised the article. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Figure1
PDX reduced bacterial CFU counts in BALF after sepsis-induced ALI. Representative pictures of CFU counts in BALF in sham, CLP, LD-PDX, and HD-PDX groups. Data was presented as means ± SEM, n = 7. *P < 0.05 LD-PDX versus the CLP group; ##P < 0.01 HD-PDX versus the CLP group (JPG 78 kb)
Rights and permissions
About this article
Cite this article
Xia, H., Ge, Y., Wang, F. et al. Protectin DX ameliorates inflammation in sepsis-induced acute lung injury through mediating PPARγ/NF-κB pathway. Immunol Res 68, 280–288 (2020). https://doi.org/10.1007/s12026-020-09151-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-020-09151-7