Abstract
Purpose
We examined endocrine manifestations in a cohort of paediatric patients with IC-GCTs at diagnosis and during follow-up, integrating clinical, radiological, histopathological and laboratory data.
Methods
Diabetes insipidus (DI), growth hormone deficiency (GHD), hypothyroidism, adrenal insufficiency, precocious puberty (PP)/hypogonadism were diagnosed clinically and biochemically. The prevalence of endocrine manifestations was compared to survival rates.
Results
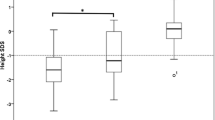
Our population included 55 children (37 males, 18 females) diagnosed with IC-GCT with a median follow-up of 78.9 months from diagnosis (range 0.5–249.9). At tumour diagnosis, 50.9% patients displayed endocrinopathies: among them, 85.7% were affected by DI, 57.1% central adrenal insufficiency, 50% central hypothyroidism, 28.5% GHD, 10.7% hypogonadotrophic hypogonadism, 10.7% PP. These patients presented predominantly with suprasellar germinoma. If not diagnosed previously, endocrine disorders arose 15.15 months (1.3–404.2) after end of treatment (EOT) in 16.4% patients. At least one endocrinopathy was identified in 67.3% of subjects at last follow-up visit, especially GHD and adrenal insufficiency. DI, hypothyroidism, and adrenal insufficiency occurred earlier than other abnormalities and frequently preceded tumour diagnosis. Subjects with and without endocrine manifestations who survived beyond 12 months after EOT did not show significant difference in overall survival and progression-free survival (p = 0.28 and p = 0.88, respectively).
Conclusion
Endocrinopathies were common presenting symptoms in our population. If present at diagnosis, they often persisted hence after. The spectrum of endocrinopathies expanded during follow-up up to 33.7 years after EOT. Although they did not seem to affect survival rate in our cohort, close lifelong surveillance is mandatory to provide the best care for these patients.



Similar content being viewed by others
References
H. Gittleman, G. Cioffi, T. Vecchione-Koval, Q.T. Ostrom, C. Kruchko, D.S. Osorio, et al. Descriptive epidemiology of germ cell tumors of the central nervous system diagnosed in the United States from 2006 to 2015. J Neurooncol (2019). https://doi.org/10.1007/s11060-019-03173-4
H. Takami, K. Fukuoka, S. Fukushima, T. Nakamura, A. Mukasa, N. Saito, et al. Integrated clinical, histopathological, and molecular data analysis of 190 central nervous system germ cell tumors from the iGCT Consortium. Neuro Oncol (2019). https://doi.org/10.1093/neuonc/noz139
Y. Narita, S. Shibui, Trends and outcomes in the treatment of gliomas based on data during 2001–2004 from the brain tumor registry of Japan. Neurol Med Chir (Tokyo) (2015). https://doi.org/10.2176/nmc.ra.2014-0348
D.N. Louis, H. Ohgaki, O.D. Wiestler, W.K. Cavenee, P.C. Burger, A. Jouvet, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol (2007). https://doi.org/10.1007/s00401-007-0243-4
H. Ogino, Y. Shibamoto, T. Takanaka, K. Suzuki, S.I. Ishihara, T. Yamada, et al. CNS germinoma with elevated serum human chorionic gonadotropin level: Clinical characteristics and treatment outcome. Int J Radiat Oncol Biol Phys (2005). https://doi.org/10.1016/j.ijrobp.2004.10.026
Khatua S., Fangusaro J., Dhall G., Boyett J., Wu S., Bartels U. GC-17THE CHILDREN’S ONCOLOGY GROUP (COG) CURRENT TREATMENT APPROACH FOR CHILDREN WITH NEWLY DIAGNOSED CENTRAL NERVOUS SYSTEM (CNS) LOCALIZED GERMINOMA (ACNS1123 STRATUM 2). Neuro Oncol (2016). https://doi.org/10.1093/neuonc/now072.17
J. Fangusaro, S. Wu, S. MacDonald, E. Murphy, D. Shaw, U. Bartels, et al. Phase II trial of response-based radiation therapy for patients with localized CNS nongerminomatous germ cell tumors: A children’s oncology group study. J Clin Oncol (2019). https://doi.org/10.1200/JCO.19.00701
G. Calaminus, R. Kortmann, J. Worch, J.C. Nicholson, C. Alapetite, M.L. Garrè, et al. SIOP CNS GCT 96: Final report of outcome of a prospective, multinational nonrandomized trial for children and adults with intracranial germinoma, comparing craniospinal irradiation alone with chemotherapy followed by focal primary site irradiation for pat. Neuro Oncol (2013). https://doi.org/10.1093/neuonc/not019
G. Calaminus, D. Frappaz, R.D. Kortmann, B. Krefeld, F. Saran, T. Pietsch, et al. Outcome of patients with intracranial non-germinomatous germ cell tumors - Lessons from the SIOP-CNS-GCT-96 trial. Neuro Oncol (2017). https://doi.org/10.1093/neuonc/nox122
Y. Sawamura, J. Ikeda, H. Shirato, M. Tada, H. Abe, Germ cell tumours of the central nervous system: treatment consideration based on 111 cases and their long-term clinical outcomes. Eur J Cancer (1998). https://doi.org/10.1016/S0959-8049(97)10045-4
M. Matsutani, K. Sano, K. Takakura, T. Fujimaki, O. Nakamura, N. Funata, et al. Primary intracranial germ cell tumors: a clinical analysis of 153 histologically verified cases. J Neurosurg (1997). https://doi.org/10.3171/jns.1997.86.3.0446
J.P. Kilday, S. Laughlin, S. Urbach, E. Bouffet, U. Bartels, Diabetes insipidus in pediatric germinomas of the suprasellar region: characteristic features and significance of the pituitary bright spot. J Neurooncol (2015). https://doi.org/10.1007/s11060-014-1619-7
R.V. Sethi, R. Marino, A. Niemierko, N.J. Tarbell, T.I. Yock, MacDonald S.M. Delayed diagnosis in children with intracranial germ cell tumors. J Pediatr (2013). https://doi.org/10.1016/j.jpeds.2013.06.024
G.T. Armstrong, Q. Liu, Y. Yasui, J.P. Neglia, W. Leisenring, L.L. Robison, et al. Late mortality among 5-year survivors of childhood cancer: A summary from the childhood cancer survivor study. J Clin Oncol (2009). https://doi.org/10.1200/JCO.2008.21.1425
S. Cheng, J.P. Kilday, N. Laperriere, L. Janzen, J. Drake, E. Bouffet, et al. Outcomes of children with central nervous system germinoma treated with multi-agent chemotherapy followed by reduced radiation. J Neurooncol (2016). https://doi.org/10.1007/s11060-015-2029-1
A. Takada, N. Ii, M. Hirayama, H. Toyoda, T. Matsubara, Y. Toyomasu, et al. Long-term follow-up of intensive chemotherapy followed by reduced-dose and reduced-field irradiation for intracranial germ cell tumor. J Neurosurg Pediatr (2019). https://doi.org/10.3171/2018.9.PEDS18181
K. Odagiri, M. Omura, M. Hata, N. Aida, T. Niwa, I. Ogino, et al. Treatment outcomes, growth height, and neuroendocrine functions in patients with intracranial germ cell tumors treated with chemoradiation therapy. Int J Radiat Oncol Biol Phys (2012). https://doi.org/10.1016/j.ijrobp.2011.12.084
W. Chemaitilly, Z. Li, S. Huang, K.K. Ness, K.L. Clark, D.M. Green, et al. Anterior hypopituitarism in adult survivors of childhood cancers treated with cranial radiotherapy: A report from the st jude lifetime cohort study. J Clin Oncol (2015). https://doi.org/10.1200/JCO.2014.56.7933
W. Chemaitilly, C.A. Sklar Childhood cancer treatments and associated endocrine late effects: a concise guide for the pediatric endocrinologist. Horm Res Paediatr (2019). https://doi.org/10.1159/000493943
C. Balmaceda, G. Heller, M. Rosenblum, B. Diez, J.G. Villablanca, S. Kellie, et al. Chemotherapy without irradiation - A novel approach for newly diagnosed CNS germ cell tumors: Results of an international cooperative trial. J Clin Oncol (1996). https://doi.org/10.1200/JCO.1996.14.11.2908
J.C. Buckner, P.P. Peethambaram, W.A. Smithson, R.V. Groover, P.J. Schomberg, D.W. Kimmel, et al. Phase II trial of primary chemotherapy followed by reduced-dose radiation for CNS germ cell tumors. J Clin Oncol (1999) https://doi.org/10.1200/jco.1999.17.3.933
J. Hayden, M.J. Murray, U. Bartels, T. Ajithkumar, B. Muthusamy, A. Penn, et al. Symptom interval and treatment burden for patients with malignant central nervous system germ cell tumours. Arch Dis Child (2020). https://doi.org/10.1136/archdischild-2019-317245
M.R. Fetell, B.M. Stein, Neuroendocrine aspects of pineal tumors. Neurol Clin (1986). https://doi.org/10.1016/s0733-8619(18)30953-8
I.J. Lin, S.G. Shu, H.Y. Chu, C.S. Chi, Primary intracranial germ-cell tumor in children. Zhonghua Yi Xue Za Zhi (Taipei) 60(5), 259–264 (1997)
J.I. Kitay, Pineal lesions and precocious puberty: A review. J Clin Endocrinol Metab (1954). https://doi.org/10.1210/jcem-14-6-622
K. Nogueira, B. Liberman, F. Rodrigues Pimentel-Filho, J. Goldman, M.E.R. Silva, J.O. Vieira, et al. hCG-secreting pineal teratoma causing precocious puberty: Report of two patients and review of the literature. J Pediatr Endocrinol Metab (2002). https://doi.org/10.1515/JPEM.2002.15.8.1195
G.A. Hale, N.M. Marina, D. Jones-Wallace, C.A. Greenwald, J.J. Jenkins, B.N. Rao, et al. Late effects of treatment for germ cell tumors during childhood and adolescence. J Pediatr Hematol Oncol (1999). https://doi.org/10.1097/00043426-199903000-00007
S. Scoccianti, B. Detti, D. Gadda, D. Greto, I. Furfaro, F. Meacci, et al. Organs at risk in the brain and their dose-constraints in adults and in children: A radiation oncologist’s guide for delineation in everyday practice. Radiother Oncol (2015). https://doi.org/10.1016/j.radonc.2015.01.016
J.C. Marsh, B.T. Gielda, A.M. Herskovic, R.A. Abrams, Cognitive sparing during the administration of whole brain radiotherapy and prophylactic cranial irradiation: Current concepts and approaches. J Oncol (2010). https://doi.org/10.1155/2010/198208
H.W.C. Leung, A.L.F. Chan, M.B. Chang, Brain dose-sparing radiotherapy techniques for localized intracranial germinoma: Case report and literature review of modern irradiation. Cancer/Radiotherapie (2016). https://doi.org/10.1016/j.canrad.2016.02.007
L. Kahalley, M.F. Okcu, M.D. Ris, D. Grosshans, A. Paulino, M.M. Chintagumpala, et al. IQ change within three years of radiation therapy in pediatric brain tumor patients treated with proton beam radiation therapy versus photon radiation therapy. J Clin Oncol (2013). https://doi.org/10.1200/jco.2013.31.15_suppl.10009
C.A. Sklar, Z. Antal, W. Chemaitilly, L.E. Cohen, C. Follin, L.R. Meacham, et al. Hypothalamic–pituitary and growth disorders in survivors of childhood cancer: An endocrine society* clinical practice guideline. J Clin Endocrinol Metab (2018). https://doi.org/10.1210/jc.2018-01175
K. Chiba, Y. Aihara, T. Kawamata, Clinical experience of growth hormone replacement for pediatric intracranial germ cell tumor. Child’s Nerv Syst (2020). https://doi.org/10.1007/s00381-020-04549-y
S. Edate, A. Albanese, Management of electrolyte and fluid disorders after brain surgery for pituitary/suprasellar tumours. Horm Res Paediatr (2015). https://doi.org/10.1159/000370065
A. Kumanogoh, S. Kasayama, H. Kouhara, M. Koga, N. Arita, T. Hayakawa, T. Kishimoto, B. Sato, Effects of therapy on anterior pituitary functions in patients with primary intracranial germ cell tumor. Endocr J (1994). https://doi.org/10.1507/endocrj.41.287
A.R. Cohen, J.A. Wilson, A. Sadeghi-Nejad, Gonadotropin-secreting pineal teratoma causing precocious puberty. Neurosurgery (1991). https://doi.org/10.1227/00006123-199104000-00021
C.A. Sklar, F.A. Conte, S.L. Kaplan, M.M. Grumbach, Human chorionic gonadotropin-secreting pineal tumors relation to pathogenesis and sex limitation of sexual precocity. J Clin Endocrinol Metab (1981). https://doi.org/10.1210/jcem-53-3-656
M.J. Abuzzahab, C.L. Roth, A.H. Shoemaker, Hypothalamic obesity: prologue and promise. Horm. Res Paediatr. 91(2), 128–136 (2019). https://doi.org/10.1159/000496564
M.J. Murray, S. Bailey, K. Heinemann, J. Mann, U.K. Göbel, F. Saran, et al. Treatment and outcomes of UK and German patients with relapsed intracranial germ cell tumors following uniform first-line therapy. Int J Cancer (2017). https://doi.org/10.1002/ijc.30755
Acknowledgements
The authors thank Dr. Kavitha Srivatsa, Specialty Doctor, Paediatric Oncology, The Royal Marsden NHS Foundation Trust, London, UK, for her kind help in data acquisition.
Author contributions
C.P. and A.A. contributed to the study conception and design. Data collection and analysis were performed by C.P. and V.B.A. The first draft of the manuscript was written by C.P. A.A. and F.C. commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest. F.C. is partly funded by the Giant Pledge via the Royal Marsden Cancer Charity. The Paediatric Neuro-Oncology and Drug Development Units receive charitable funding from the Hall-Hunter Foundation via the Royal Marsden Cancer Charity.
Ethics approval
This study was performed in accordance with the ethical standards of the local institutional Ethics Committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Partenope, C., Pozzobon, G., Weber, G. et al. Endocrine manifestations of paediatric intracranial germ cell tumours: from diagnosis to long-term follow-up. Endocrine 77, 546–555 (2022). https://doi.org/10.1007/s12020-022-03121-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03121-9