Abstract
Objective
The use of antithyroid drug (ATD) therapy in patients with Graves’ disease (GD) hyperthyroidism has been increasing, but ATD therapy is associated with a higher relapse rate. We aimed to evaluate clinical factors for predicting relapse of GD after ATD therapy.
Methods
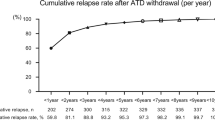
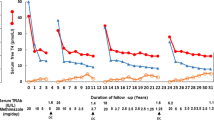
Patients (n = 149) with newly diagnosed GD who achieved remission of hyperthyroidism after ATD therapy (≥6 months) were followed up for >18 months after ATD withdrawal. We evaluated the predictive factors of relapse during a median of 6.9 years of follow-up.
Results
Disease relapse occurred in 52 patients (34.9%). By multivariate analyses, a duration of the minimum maintenance dose therapy (MMDT) of <6 months was a significant factor in disease relapse (hazard ratio [HR], 2.58; 95% confidence interval [CI], 1.47–4.52; p < 0.001), and a T3/free T4 (fT4) ratio > 120 at ATD withdrawal was significantly more frequent in patients with relapse (HR 2.43; 95% CI, 1.36–4.34; p = 0.002). In the prediction-of-relapse model, the likelihood of relapse was greater in the high-risk group, which had a short MMDT duration and a T3/fT4 ratio ≥120 (HR, 5.81; 95% CI, 2.52–13.39; p < 0.001) and the intermediate-risk group, which had a short MMDT duration or a T3/fT4 ratio < 120 (HR, 2.77; 95% CI, 1.26–6.13; p < 0.001), than in the low-risk group, which had a long MMDT duration and a T3/fT4 ratio < 120.
Conclusion
An MMDT longer than 6 months and a high T3/fT4 ratio at ATD withdrawal were independent predictors of relapse in patients who achieved initial remission after ATD for GD. These factors could be used to determine the optimal time to withdraw ATD during the treatment of GD hyperthyroidism.


Similar content being viewed by others
References
D.S. Ross, H.B. Burch, D.S. Cooper, M.C. Greenlee, P. Laurberg, A.L. Maia, S.A. Rivkees, M. Samuels, J.A. Sosa, M.N. Stan, 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 26(10), 1343–1421 (2016)
J.P. Brito, S. Schilz, N. Singh Ospina, R. Rodriguez-Gutierrez, S. Maraka, L.R. Sangaralingham, V.M. Montori, Antithyroid drugs—the most common treatment for Graves’ disease in the United States: a nationwide population-based study. Thyroid 26(8), 1144–1145 (2016)
E. Mohlin, H.F. Nyström, M. Eliasson, Long-term prognosis after medical treatment of Graves’ disease in a northern Swedish population 2000-2010. Eur. J. Endocrinol. 170, 419–427 (2013)
H.B. Burch, K.D. Burman, D.S. Cooper, A 2011 survey of clinical practice patterns in the management of Graves’ disease. J. Clin. Endocrinol. Metab. 97(12), 4549–4558 (2012)
D. Villagelin, J.H. Romaldini, R.B. Santos, A.B. Milkos, L.S. Ward, Outcomes in relapsed Graves’ disease patients following radioiodine or prolonged low dose of methimazole treatment. Thyroid 25(12), 1282–1290 (2015)
K.H. Yi, J.H. Moon, I.-J. Kim, H.-S. Bom, J. Lee, W.Y. Chung, J.H. Chung, Y.K. Shong, The diagnosis and management of hyperthyroidism consensus-report of the Korean Thyroid Association. J. Korean Thyroid Assoc. 6(1), 1–11 (2013)
S. Yamashita, N. Amino, Y.K. Shong. The American Thyroid Association and American Association of Clinical Endocrinologists hyperthyroidism and other causes of thyrotoxicosis guidelines: viewpoints from Japan and Korea. (Mary Ann Liebert, Inc, 140 Huguenot Street, 3rd Floor New Rochelle, NY 10801 USA), 2011)
E. Mohlin, H. Filipsson Nystrom, M. Eliasson, Long-term prognosis after medical treatment of Graves’ disease in a northern Swedish population 2000-2010. Eur. J. Endocrinol. 170(3), 419–427 (2014). https://doi.org/10.1530/eje-13-0811
F. Azizi, L. Ataie, M. Hedayati, Y. Mehrabi, F. Sheikholeslami, Effect of long-term continuous methimazole treatment of hyperthyroidism: comparison with radioiodine. Eur. J. Endocrinol. 152(5), 695–701 (2005)
P. Abraham, A. Avenell, S. McGeoch, L.F. Clark, J.S. Bevan, Antithyroid drug regimen for treating Graves’ hyperthyroidism. Cochrane Database Syst. Rev. CD003420 (2010)
A. Allahabadia, J. Daykin, R.L. Holder, M.C. Sheppard, S.C. Gough, J.A. Franklyn, Age and gender predict the outcome of treatment for Graves’ hyperthyroidism. The. J. Clin. Endocrinol. Metab. 85(3), 1038–1042 (2000)
P. Vitti, T. Rago, L. Chiovato, S. Pallini, F. Santini, E. Fiore, R. Rocchi, E. Martino, A. Pinchera, Clinical features of patients with Graves’ disease undergoing remission after antithyroid drug treatment. Thyroid 7(3), 369–375 (1997)
T. Chowdhury, P. Dyer, Clinical, biochemical and immunological characteristics of relapsers and non‐relapsers of thyrotoxicosis treated with anti‐thyroid drugs. J. Intern. Med. 244(4), 293–297 (1998)
D. Glinoer, P. De Nayer, M. Bex, Effects of l-thyroxine administration, TSH-receptor antibodies and smoking on the risk of recurrence in Graves’ hyperthyroidism treated with antithyroid drugs: a double-blind prospective randomized study. Eur. J. Endocrinol. 144(5), 475–483 (2001)
B. Nedrebo, P.I. Holm, S. Uhlving, J. Sorheim, S. Skeie, G.E. Eide, E.S. Husebye, E.A. Lien, S. Aanderud, Predictors of outcome and comparison of different drug regimens for the prevention of relapse in patients with Graves’ disease. Eur. J. Endocrinol. 147(5), 583–589 (2002)
A.K. Eckstein, H. Lax, C. Lösch, D. Glowacka, M. Plicht, K. Mann, J. Esser, N.G. Morgenthaler, Patients with severe Graves’ ophthalmopathy have a higher risk of relapsing hyperthyroidism and are unlikely to remain in remission. Clin. Endocrinol. 67(4), 607–612 (2007)
C. Cappelli, E. Gandossi, M. Castellano, C. Pizzocaro, B. Agosti, A. Delbarba, I. Pirola, E. De Martino, E.A. Rosei, Prognostic value of thyrotropin receptor antibodies (TRAb) in Graves’ disease: a 120 months prospective study. Endocr. J. 54(5), 713–720 (2007)
P. Laurberg, G. Wallin, L. Tallstedt, M. Abraham-Nordling, G. Lundell, O. Tørring, TSH-receptor autoimmunity in Graves’ disease after therapy with anti-thyroid drugs, surgery, or radioiodine: a 5-year prospective randomized study. Eur. J. Endocrinol. 158(1), 69–75 (2008)
C. Carella, G. Mazziotti, F. Sorvillo, M. Piscopo, M. Cioffi, P. Pilla, R. Nersita, S. Iorio, G. Amato, L. Braverman, Serum thyrotropin receptor antibodies concentrations in patients with Graves’ disease before, at the end of methimazole treatment, and after drug withdrawal: evidence that the activity of thyrotropin receptor antibody and/or thyroid response modify during the observation period. Thyroid 16(3), 295–302 (2006)
H.S. Choi, W.S. Yoo, Free thyroxine, anti-thyroid stimulating hormone receptor antibody titers, and absence of goiter were associated with responsiveness to methimazole in patients with new onset Graves’ disease. Endocrinol. Metab. 32(2), 281–287 (2017)
M. Rotondi, C. Cappelli, B. Pirali, I. Pirola, F. Magri, R. Fonte, M. Castellano, E.A. Rosei, L. Chiovato, The effect of pregnancy on subsequent relapse from Graves’ disease after a successful course of antithyroid drug therapy. J. Clin. Endocrinol. Metab. 93(10), 3985–3988 (2008). https://doi.org/10.1210/jc.2008-0966
Y.A. Kim, S.W. Cho, H.S. Choi, S. Moon, J.H. Moon, K.W. Kim, D.J. Park, K.H. Yi, Y.J. Park, B.Y. Cho, The second antithyroid drug treatment is effective in relapsed Graves’ disease patients: a median 11-year follow-up study. Thyroid 27(4), 491–496 (2017)
U. Feldt-Rasmussen, H. Schleusener, P. Carayon, Meta-analysis evaluation of the impact of thyrotropin receptor antibodies on long term remission after medical therapy of Graves’ disease. J. Clin. Endocrinol. Metab. 78(1), 98–102 (1994)
D. Strich, G. Karavani, S. Edri, D. Gillis, TSH enhancement of FT4 to FT3 conversion is age dependent. Eur. J. Endocrinol. 175, 49–54 (2016). EJE-16-0007
H. Kwon, W.G. Kim, E.K. Jang, M. Kim, S. Park, M.J. Jeon, T.Y. Kim, J.-S. Ryu, Y.K. Shong, W.B. Kim, Usefulness of measuring thyroid stimulating antibody at the time of antithyroid drug withdrawal for predicting relapse of Graves disease. Endocrinol. Metab. 31(2), 300–310 (2016)
E. Peterson, P. De, R. Nuttall, BMI, diet and female reproductive factors as risks for thyroid cancer: a systematic review. PLoS ONE 7(1), e29177 (2012). https://doi.org/10.1371/journal.pone.0029177
M.P. Mourits, M.F. Prummel, W.M. Wiersinga, L. Koornneef, Clinical activity score as a guide in the management of patients with Graves’ ophthalmopathy. Clin. Endocrinol. 47(1), 9–14 (1997)
L. Bartalena, L. Baldeschi, A.J. Dickinson, A. Eckstein, P. Kendall-Taylor, C. Marcocci, M.P. Mourits, P. Perros, K. Boboridis, A. Boschi, Consensus statement of the European group on Graves’ orbitopathy (EUGOGO) on management of Graves’ orbitopathy. Thyroid 18(3), 333–346 (2008)
World Health Organization, Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers (Geneva: World Health Organization, 2007).
S.M. ChoBY, L. YiKH, M.H. KohCS, Evaluationofserum basalthyrotropinlevelsand thyrotopinreceptorantibodyactivitiesasprognostic markers for discontinuation of antithyroid drug treatmentinpatientswithGraves’ disease. Clin. Endocrinol. 36, 585–590 (1992)
T. Konishi, Y. Okamoto, M. Ueda, Y. Fukuda, I. Harusato, Y. Tsukamoto, N. Hamada, Drug discontinuation after treatment with minimum maintenance dose of an antithyroid drug in Graves’ disease: a retrospective study on effects of treatment duration with minimum maintenance dose on lasting remission. Endocr. J. 58(2), 95–100 (2011)
M.J. Jeon, W.G. Kim, E.K. Jang, Y.M. Choi, Y.-M. Lee, T.-Y. Sung, J.H. Yoon, K.-W. Chung, S.J. Hong, J.H. Baek, Thyroglobulin level in fine-needle aspirates for preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma: two different cutoff values according to serum thyroglobulin level. Thyroid 25(4), 410–416 (2015)
W.B. Kim, Clinical applications of thyrotropin binding inhibitor immunoglobulin (TBII) assays. J. Korean Endocr. Soc. 23(3), 174–178 (2008)
R.V. García-Mayor, C. Paramo, R.L. Cano, L.P. Mendez, J. Galofre, A. Andrade, Antithyroid drug and Graves’ hyperthyroidism. Significance of treatment duration and TRAb determination on lasting remission. J. Endocrinol. Investig. 15(11), 815–820 (1992)
P. Laurberg, Remission of Graves’ disease during anti-thyroid drug therapy. Time to reconsider the mechanism? Eur. J. Endocrinol. 155(6), 783–786 (2006)
T. Ando, R. Latif, T.F. Davies, Concentration-dependent regulation of thyrotropin receptor function by thyroid-stimulating antibody. J. Clin. Investig. 113(11), 1589–1595 (2004)
S. Costagliola, N.G. Morgenthaler, R. Hoermann, K. Badenhoop, J. Struck, D. Freitag, S. Poertl, W. Weglöhner, Jr.M. Hollidt, B: Quadbeck, Second generation assay for thyrotropin receptor antibodies has superior diagnostic sensitivity for Graves’ disease. J. Clin. Endocrinol. Metab. 84(1), 90–997 (1999)
X.G. Vos, N. Smit, E. Endert, J.G. Tijssen, W.M. Wiersinga, Frequency and characteristics of TBII-seronegative patients in a population with untreated Graves’ hyperthyroidism: a prospective study. Clin. Endocrinol. 69(2), 311–317 (2008). https://doi.org/10.1111/j.1365-2265.2008.03192.x
A.C. Bianco, D. Salvatore, B. Gereben, M.J. Berry, P.R. Larsen, Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr. Rev. 23(1), 38–89 (2002)
P. Laurberg, Mechanisms governing the relative proportions of thyroxine and 3, 5, 3′-triiodothyronine in thyroid secretion. Metabolism 33(4), 379–392 (1984)
P. Laurberg, Thyroxine and 3, 5, 3′-triiodothyronine content of thyroglobulin in thyroid needle aspirates in hyperthyroidism and hypothyroidism. J. Clin. Endocrinol. Metab. 64(5), 969–974 (1987).
P. Laurberg, H. Vestergaard, S. Nielsen, S.E. Christensen, T. Seefeldt, K. Helleberg, K.M. Pedersen, Sources of circulating 3, 5, 3′-triiodothyronine in hyperthyroidism estimated after blocking of type 1 and type 2 iodothyronine deiodinases. J. Clin. Endocrinol. Metab. 92(6), 2149–2156 (2007)
A. Carlé, N. Knudsen, I.B. Pedersen, H. Perrild, L. Ovesen, L.B. Rasmussen, P. Laurberg, Determinants of serum T4 and T3 at the time of diagnosis in nosological types of thyrotoxicosis: a population-based study. Eur. J. Endocrinol. 169(5), 537–545 (2013)
J. Takamatsu, K. Kuma, T. Mozai, Serum triiodothyronine to thyroxine ratio: a newly recognized predictor of the outcome of hyperthyroidism due to Graves’ disease. J. Clin. Endocrinol. Metab. 62(5), 980–983 (1986).
B.L. Solomon, J.E. Evaul, K.D. Burman, L. Wartofsky, Remission rates with antithyroid drug therapy: continuing influence of iodine intake?. Ann. Intern. Med. 107(4), 510–512 (1987).
F. Azizi, Environmental iodine intake affects the response to methimazole in patients with diffuse toxic goiter. J. Clin. Endocrinol. Metab. 61(2), 374–377 (1985).
S.M. Park, Y.Y. Cho, J.Y. Joung, S.Y. Sohn, S.W. Kim, J.H. Chung, Excessive iodine intake does not increase the recurrence rate of Graves’ disease after withdrawal of the antithyroid drug in an iodine-replete area. Eur. thyroid J. 4(1), 36–42 (2015)
T. Hiraiwa, M. Ito, A. Imagawa, J. Takamatsu, K. Kuma, A. Miyauchi, T. Hanafusa, Restriction of dietary Iodine does not ameliorate the early effect of anti-thyroid drug therapy for Graves’ disease in an area of excessive iodine intake. J. Endocrinol. Investig. 29(4), 380–384 (2006)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of Asan Medical Center, Seoul, Korea, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, S., Song, E., Oh, HS. et al. When should antithyroid drug therapy to reduce the relapse rate of hyperthyroidism in Graves’ disease be discontinued?. Endocrine 65, 348–356 (2019). https://doi.org/10.1007/s12020-019-01987-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01987-w