Abstract
Purpose
To describe the volumetric changes that the pituitary gland (PG) undergoes during and after transsphenoidal surgery (TSS), and to evaluate if unfolding and/or pruning are related to endocrinological outcome measures.
Methods
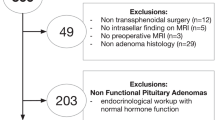
Retrospective evaluation of data prospectively collected of a cohort of patients undergoing TSS for a pituitary adenoma with the adjunctive use of high field 3 Tesla intraoperative MRI. All patients underwent a full endocrinological workup preoperatively, as well as at 6 weeks and 1 year postoperatively. A decrease in PG volume ≥15% between the intraoperative and 3-month, or between the 3-month and 12-month measurements, was considered early and late pruning, respectively.
Results
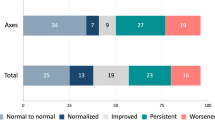
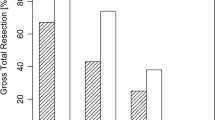
The PG unfolds significantly during TSS, and subsequently undergoes pruning up until 1 year postoperatively, in most cases returning to the preoperatively measured PG volume. A smaller baseline PG volume predicts intraoperative unfolding. Early pruning of the PG after surgery was associated with new functional deficits. Baseline pituitary compression also correlated to newly occurring deficits after surgery. A larger 1-year pituitary volume was associated with biochemical remission in secreting adenomas.
Conclusions
The PG shows dynamic change during and after TSS for pituitary adenoma. Small baseline and 3-month PG volumes, as well as early pruning were independently associated with new deficits. Our findings warrant prospective validation in a larger cohort with higher statistical power.





Similar content being viewed by others
References
P. Cappabianca, L.M. Cavallo, D. Solari, V. Stagno, F. Esposito, M. de Angelis, Endoscopic endonasal surgery for pituitary adenomas. World Neurosurg. 82, S3–S11 (2014). https://doi.org/10.1016/j.wneu.2014.07.019
C. Serra, J.-K. Burkhardt, G. Esposito, O. Bozinov, A. Pangalu, A. Valavanis, D. Holzmann, C. Schmid, L. Regli, Pituitary surgery and volumetric assessment of extent of resection: a paradigm shift in the use of intraoperative magnetic resonance imaging. Neurosurg. Focus 40, E17 (2016). https://doi.org/10.3171/2015.12.FOCUS15564
M. Losa, P. Mortini, R. Barzaghi, P. Ribotto, M.R. Terreni, S.B. Marzoli, S. Pieralli, M. Giovanelli, Early results of surgery in patients with nonfunctioning pituitary adenoma and analysis of the risk of tumor recurrence. J. Neurosurg. 108, 525–532 (2008). https://doi.org/10.3171/JNS/2008/108/3/0525
R.F. Dallapiazza, Y. Grober, R.M. Starke, E.R. Laws, J.A. Jane, Long-term results of endonasal endoscopic transsphenoidal resection of nonfunctioning pituitary macroadenomas. Neurosurgery 76, 42–52 (2015). https://doi.org/10.1227/NEU.0000000000000563.
A.R. Dehdashti, A. Ganna, K. Karabatsou, F. Gentili, Pure endoscopic endonasal approach for pituitary adenomas: early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery 62, 1006–1015 (2008). https://doi.org/10.1227/01.neu.0000325862.83961.12.
P. Mortini, L.R. Barzaghi, L. Albano, P. Panni, M. Losa, Microsurgical therapy of pituitary adenomas. Endocrine 59, 72–81 (2018). https://doi.org/10.1007/s12020-017-1458-3
C. Serra, N. Maldaner, G. Muscas, V. Staartjes, A. Pangalu, D. Holzmann, M. Soyka, C. Schmid, L. Regli. The changing sella: internal carotid artery shift during transsphenoidal pituitary surgery. Pituitary. 1–7 (2017). https://doi.org/10.1007/s11102-017-0830-x
N. Fatemi, J.R. Dusick, C. Mattozo, D.L. McArthur, P. Cohan, J. Boscardin, C. Wang, R.S. Swerdloff, D.F. Kelly, Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63, 709–719 (2008). https://doi.org/10.1227/01.NEU.0000325725.77132.90
B.M. Arafah, D. Prunty, J. Ybarra, M.L. Hlavin, W.R. Selman, The dominant role of increased intrasellar pressure in the pathogenesis of hypopituitarism, hyperprolactinemia, and headaches in patients with pituitary adenomas. J. Clin. Endocrinol. Metab. 85, 1789–1793 (2000). https://doi.org/10.1210/jcem.85.5.6611
M. Fleseriu, I.A. Hashim, N. Karavitaki, S. Melmed, M.H. Murad, R. Salvatori, M.H. Samuels, Hormonal Replacement in hypopituitarism in adults: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 101, 3888–3921 (2016). https://doi.org/10.1210/jc.2016-2118
A. Giustina, P. Chanson, M.D. Bronstein, A. Klibanski, S. Lamberts, F.F. Casanueva, P. Trainer, E. Ghigo, K. Ho, S. Melmed, A consensus on criteria for cure of acromegaly. J. Clin. Endocrinol. Metab. 95, 3141–3148 (2010). https://doi.org/10.1210/jc.2009-2670
B.M.K. Biller, A.B. Grossman, P.M. Stewart, S. Melmed, X. Bertagna, J. Bertherat, M. Buchfelder, A. Colao, A.R. Hermus, L.J. Hofland, A. Klibanski, A. Lacroix, J.R. Lindsay, J. Newell-Price, L.K. Nieman, S. Petersenn, N. Sonino, G.K. Stalla, B. Swearingen, M.L. Vance, J.A.H. Wass, M. Boscaro, Treatment of adrenocorticotropin-dependent Cushing’s syndrome: a consensus statement. J. Clin. Endocrinol. Metab. 93, 2454–2462 (2008). https://doi.org/10.1210/jc.2007-2734
A.S.G. Micko, A. Wöhrer, S. Wolfsberger, E. Knosp, Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J. Neurosurg. 122, 803–811 (2015). https://doi.org/10.3171/2014.12.JNS141083
E. Steiner, G. Math, E. Knosp, G. Mostbeck, J. Kramer, C.J. Herold, MR-appearance of the pituitary gland before and after resection of pituitary macroadenomas. Clin. Radiol. 49, 524–530 (1994)
T.S. Dina, S.H. Feaster, E.R. Laws, D.O. Davis, MR of the pituitary gland postsurgery: serial MR studies following transsphenoidal resection. Am. J. Neuroradiol. 14, 763–769 (1993)
O. Rodríguez, B. Mateos, R. Pedraja, R. de la, Villoria, J.I. Hernando, A. Pastor, I. Pomposo, J. Aurrecoechea, Postoperative follow-up of pituitary adenomas after transsphenoidal resection: MRI and clinical correlation. Neuroradiology 38, 747–754 (1996). https://doi.org/10.1007/s002340050341
K.R. Cho, S.D. Hong, K.Y. Hur, S.T. Kim, H.J. Seol, J.-I. Lee, D.-S. Kong, D.-H. Nam, Serial re-expansion of pituitary gland is associated with endocrinologic recovery. World Neurosurg. 90, 496–503 (2016). https://doi.org/10.1016/j.wneu.2016.03.050
A. Jahangiri, J. Wagner, S.W. Han, M.T. Tran, L.M. Miller, M.W. Tom, L.R. Ostling, S. Kunwar, L. Blevins, M.K. Aghi, Rate and time course of improvement in endocrine function after more than 1000 pituitary operations. Neurosurgery 61, 163–166 (2014). https://doi.org/10.1227/NEU.0000000000000405
S.M. Webb, M. Rigla, A. Wägner, B. Oliver, F. Bartumeus, Recovery of hypopituitarism after neurosurgical treatment of pituitary adenomas. J. Clin. Endocrinol. Metab. 84, 3696–3700 (1999). https://doi.org/10.1210/jcem.84.10.6019
A. Jahangiri, J.R. Wagner, S.W. Han, M.T. Tran, L.M. Miller, R. Chen, M.W. Tom, L.R. Ostling, S. Kunwar, L. Blevins, M.K. Aghi, Improved versus worsened endocrine function after transsphenoidal surgery for nonfunctional pituitary adenomas: rate, time course, and radiological analysis. J. Neurosurg. 124, 589–595 (2015). https://doi.org/10.3171/2015.1.JNS141543
A.T. Nelson, H.S.G. Tucker, D.P. Becker, Residual anterior pituitary function following transsphenoidal resection of pituitary macroadenomas. J. Neurosurg. 61, 577–580 (1984). https://doi.org/10.3171/jns.1984.61.3.0577
M.E. Sughrue, E.F. Chang, R.A. Gabriel, M.K. Aghi, L.S. Blevins, Excess mortality for patients with residual disease following resection of pituitary adenomas. Pituitary 14, 276–283 (2011). https://doi.org/10.1007/s11102-011-0308-1
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
These authors contributed equally: Victor Staartjes, Sarah Stricker.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Staartjes, V.E., Stricker, S., Muscas, G. et al. Intraoperative unfolding and postoperative pruning of the pituitary gland after transsphenoidal surgery for pituitary adenoma: A volumetric and endocrinological evaluation. Endocrine 63, 231–239 (2019). https://doi.org/10.1007/s12020-018-1758-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1758-2