Abstract
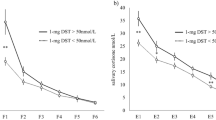
Salivary cortisol (SC) has been increasingly used as a surrogate biomarker of free cortisol (FC) for the assessment of hypothalamo-pituitary-adrenal (HPA) axis, but there are not enough data regarding its use during ACTH stimulation tests. Therefore, we aimed to determine the responses of SC, calculated free cortisol (cFC) and free cortisol index (FCI) to ACTH stimulation tests in healthy adults. Forty-four healthy volunteers (24 men and 20 women) were included in the study. Low-dose (1 µg) and standard-dose (250 µg) ACTH stimulation tests were performed on two consecutive days. Basal and stimulated total cortisol (TC) and cortisol-binding globulin (CBG) levels and SC levels were measured during both doses of ACTH stimulation tests. cFC (by Coolens’ equation) and FCI levels were calculated from simultaneously measured TC and CBG levels. The minimum SC, cFC, FCI levels after low-dose ACTH stimulation test were 0.21, 0.33, 16.06 µg/dL, and after standard-dose ACTH were 0.85, 0.46, 26.11 µg/dL, respectively, in healthy individuals who all had TC responses higher than 20 µg/dL. Peak CBG levels after both doses of ACTH stimulation tests were found to be higher in women than in men. So, by its effect, peak cFC and FCI levels were found to be lower in female than in male group. Neither TC nor SC levels were affected by gender. cFC and FCI levels depend on CBG levels and they are affected by gender. Cut-off levels for SC, cFC, FCI levels after both low- and standard-dose ACTH stimulation are presented. Studies including patients with adrenal insufficiency would be helpful to see the diagnostic value of these suggested cut-off levels.
Similar content being viewed by others
References
I.E. Widmer, J.J. Puder, C. Konig, H. Pargger, H.R. Zerkowski, J. Girard, B. Muller, Cortisol response in relation to the severity of stress and illness. J. Clin. Endocrinol. Metab. 90, 4579–4586 (2005)
F. Tanriverdi, Z. Karaca, K. Unluhizarci, F. Kelestimur, The hypothalamo-pituitary-adrenal axis in chronic fatigue syndrome and fibromyalgia syndrome. Stress 10, 13–25 (2007)
J.F. Dunn, B.C. Nisula, D. Rodbard, Transport of steroid hormones: binding of 21 endogenous steroids to both testosterone-binding globulin and corticosteroid binding globulin in human plasma. J. Clin. Endocrinol. Metab. 53, 58–68 (1981)
T.G. Brien, Human corticosteroid binding globulin. Clin. Endocrinol. 14, 193–212 (1981)
A.H. Hamrahian, T.S. Oseni, B.M. Arafah, Measurements of serum free cortisol in critically ill patients. N. Engl. J. Med. 350, 1629–1638 (2004)
B.M. Arafah, F.J. Nishiyama, H. Tlaygeh, R. Hejal, Measurement of salivary cortisol concentration in the assessment of adrenal function in critically ill subjects: a surrogate marker of the circulating free cortisol. J. Clin. Endocrinol. Metab. 92, 2965–2971 (2007)
P. Poomthavorn, R. Lertbunrian, A. Preutthipan, A. Sriphrapradang, P. Khlairit, P. Mahachoklertwattana, Serum free cortisol index, free cortisol, and total cortisol in critically ill children. Inten. Care Med. 35, 1281–1285 (2009)
J. Coolens, L., Van Baelen, H., Heyns, W.: Clinical use of unbound plasma cortisol as calculated from total cortisol and corticosteroid-binding globulin. J. Steroid Biochem. 26, 197–202 (1987)
W.S. Gozansky, J.S. Lynn, M.L. Laudenslager, W.M. Kohrt, Salivary cortisol determined by enzyme immunoassay is preferable to serum total cortisol for assessment of dynamic hypothalamic-pituitary-adrenal axis activity. Clin. Endocrinol. 63, 336–341 (2005)
Y. Marcus-Perlman, K. Tordjman, Y. Greenman, R. Limor, G. Shenkerman, E. Osher, N. Stern, Low-dose ACTH (1 microg) salivary test: a potential alternative to the classical blood test. Clin. Endocrinol. 64, 215–218 (2006)
M.S. Lo, M.L. Ng, B.S. Azmy, B.A. Khalid, Clinical applications of salivary cortisol measurements. Singapore Med. J. 33, 170–173 (1992)
L.N. Contreras, A.L. Arregger, G.G. Persi, N.S. Gonzalez, E.M. Cardoso, A new less-invasive and more informative low-dose ACTH test: salivary steroids in response to intramuscular corticotrophin. Clin. Endocrinol. 61, 675–682 (2004)
T. Deutschbein, M. Broecker-Preuss, J. Flitsch, A. Jaeger, R. Althoff, M.K. Walz, K. Mann, S. Petersenn, Salivary cortisol as a diagnostic tool for Cushing’s syndrome and adrenal insufficiency: improved screening by an automatic immunoassay. Eur. J. Endocrinol. 166, 613–618 (2012)
K. Simunkova, R. Hampl, M. Hill, J. Doucha, L. Starka, K. Vondra, Salivary cortisol in low dose (1 microg) ACTH test in healthy women: comparison with serum cortisol. Physiol. Res. 56, 449–453 (2007)
K. Simunkova, L. Starka, M. Hill, L. Kriz, R. Hampl, K. Vondra, Comparison of total and salivary cortisol in a low-dose ACTH (Synacthen) test: influence of three-month oral contraceptives administration to healthy women. Physiol. Res. 57, 193–199 (2008)
W. Arlt, Adrenal insufficiency. Clin Med. 8(2), 211–215 (2008)
Z. Karaca, A. Lale, F. Tanriverdi, M. Kula, K. Unluhizarci, F. Kelestimur, The comparison of low and standard dose ACTH and glucagon stimulation tests in the evaluation of hypothalamo-pituitary-adrenal axis in healthy adults. Pituitary 14, 134–140 (2011)
A. Beishuizen, L.G. Thijs, I. Vermes, Patterns of corticosteroid-binding globulin and the free cortisol index during septic shock and multitrauma. Inten. Care Med. 27, 1584–1591 (2001)
E. Topkas, P. Keith, G. Dimeski, J. Cooper-White, C. Punyadeera, Evaluation of saliva collection devices for the analysis of proteins. Clin. Chim. Acta 413, 66–70 (2012)
C.W. Le Roux, G.A. Chapman, W.M. Kong, W.S. Dhillo, J. Jones, J. Alaghband-Zadeh, Free cortisol index is better than serum total cortisol in determining hypothalamic-pituitary-adrenal status in patients undergoing surgery. J. Clin. Endocrinol. Metab. 88, 2045–2048 (2003)
J.G. Lewis, M.G. Lewis, P. Elder, An enzyme-linked immunosorbent assay for corticosteroid-binding globulin using monoclonal and polyclonal antibodies: decline in CBG following synthetic ACTH. Clin. Chim. Acta 328, 121–128 (2003)
N.L. Barlow, J. Holme, R.A. Stockley, P.M. Clark, An evaluation of measured and calculated serum free cortisol in a group of patients with known adrenal suppression. Ann. Clin. Biochem. 47, 200–204 (2010)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elbuken, G., Tanriverdi, F., Karaca, Z. et al. Comparison of salivary and calculated free cortisol levels during low and standard dose of ACTH stimulation tests in healthy volunteers. Endocrine 48, 439–443 (2015). https://doi.org/10.1007/s12020-014-0378-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0378-8