Abstract
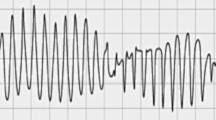
dl-Sotalol which can block both K+ channel and ß-adrenoceptor has been shown to prolong the J–Tpeakc of electrocardiogram in beagle dogs but tended to shorten it in microminipigs, although the drug prolonged the QT interval in both animals under physiologically maintained experimental condition. In order to estimate how the changes in the J–Tpeakc in the normal hearts would be reflected in the pathologic hearts, we compared proarrhythmic effects of dl-sotalol by using proarrhythmia models of beagle dogs and microminipigs, of which atrioventricular node had been ablated > 2 months and 8–9 weeks before, respectively (n = 4 for each species). dl-Sotalol in an oral dose of 10 mg/kg induced torsade de pointes in three out of four beagle dogs, which degenerated into ventricular fibrillation. In microminipigs, the same dose did not trigger torsade de pointes at all, whereas intermittent ventricular pauses were observed in each animal after the drug treatment. These results indicate that assessment of the J–Tpeakc along with the QT-interval prolongation in healthy subjects may provide reliable information of risk prediction for patients susceptible to the drug-induced torsade de pointes.



Similar content being viewed by others
References
Johannesen, L., Vicente, J., Mason, J. W., Erato, C., Sanabria, C., Waite-Labott, K., et al. (2016). Late sodium current block for drug-induced long QT syndrome: Results from a prospective clinical trial. Clinical Pharmacology & Therapeutics, 99, 214–223.
Chiba, K., Wada, T., Nakamura, Y., Cao, X., Hagiwara-Nagasawa, M., Izumi-Nakaseko, H., et al. (2017). Analysis of proarrhythmic potential of an atypical antipsychotic drug paliperidone in the halothane-anesthetized dogs. Journal of Pharmacological Sciences, 134, 239–246.
Cao, X., Nakamura, Y., Wada, T., Izumi-Nakaseko, H., Ando, K., & Sugiyama, A. (2016). Electropharmacological effects of amantadine on cardiovascular system assessed with J-Tpeak and Tpeak-Tend analysis in the halothane-anesthetized beagle dogs. The Journal of Toxicological Sciences, 41, 439–447.
Matsukura, S., Nakamura, Y., Hoshiai, K., Hayashi, T., Koga, T., Goto, A., et al. (2018). Effects of moxifloxacin on the proarrhythmic surrogate markers in healthy Filipino subjects: Exposure-response modeling using ECG data of thorough QT/QTc study. Journal of Pharmacological Sciences, 136, 234–241.
Vicente, J., Zusterzeel, R., Johannesen, L., Mason, J., Sager, P., Patel, V., et al. (2018). Mechanistic model-informed proarrhythmic risk assessment of drugs: Review of the “CiPA” initiative and design of a prospective clinical validation study. Clinical Pharmacology & Therapeutics, 103, 54–66.
Motokawa, Y., Nakamura, Y., Hagiwara-Nagasawa, M., Goto, A., Chiba, K., Lubna, N. J., et al. (2018). In vivo analysis of the anti-atrial fibrillatory, proarrhythmic and cardiodepressive profiles of dronedarone as a guide for safety pharmacological evaluation of antiarrhythmic drugs. Cardiovascular Toxicology, 18, 242–251.
Matsukura, S., Nakamura, Y., Cao, X., Wada, T., Izumi-Nakaseko, H., Ando, K., et al. (2017). Anti-atrial fibrillatory versus proarrhythmic potentials of amiodarone: A new protocol for safety evaluation in vivo. Cardiovascular Toxicology, 17, 157–162.
Harvey, R. D., & Grant, A. O. (2018). Agents used in cardiac arrhythmias. In B. G. Katzung (Ed.), Basic & clinical pharmacology (14th ed., pp. 212–227). New York: McGraw-Hill Education.
Yokoyama, H., Nakamura, Y., Saito, H., Nagayama, Y., Hoshiai, K., Wada, T., et al. (2017). Pharmacological characterization of microminipig as a model to assess the drug-induced cardiovascular responses for non-clinical toxicity and/or safety pharmacology studies. The Journal of Toxicological Sciences, 42, 93–101.
Ishizaka, T., Takahara, A., Iwasaki, H., Mitsumori, Y., Kise, H., Nakamura, Y., et al. (2008). Comparison of electropharmacological effects of bepridil and sotalol in halothane-anesthetized dogs. Circulation Journal, 72, 1003–1011.
Lynch, J. J. III, Wilson, A. W., Hernandez, L. E., Nelson, R. A., Marsh, K. C., Cox, B. F., et al. (2008). Dose-response effects of sotalol on cardiovascular function in conscious, freely moving cynomolgus monkeys. British Journal of Pharmacology, 154, 1439–1445.
Katagi, J., Nakamura, Y., Cao, X., Ohara, H., Honda, A., Izumi-Nakaseko, H., et al. (2016). Why can dl-sotalol prolong the QT interval in vivo despite its weak inhibitory effect on hERG K+ channels in vitro? Electrophysiological and pharmacokinetic analysis with the halothane-anesthetized guinea pig model. Cardiovascular Toxicology, 16, 138–146.
Sugiyama, A. (2008). Sensitive and reliable proarrhythmia in vivo animal models for predicting drug-induced torsades de pointes in patients with remodelled hearts. British Journal of Pharmacology, 154, 1528–1537.
Thomsen, M. B., Verduyn, S. C., Stengl, M., Beekman, J. D., de Pater, G., van Opstal, J., et al. (2004). Increased short-term variability of repolarization predicts d-sotalol-induced torsades de pointes in dogs. Circulation, 110, 2453–2459.
Verduyn, S. C., Vos, M. A., van der Zande, J., Kulcsàr, A., & Wellens, H. J. (1997). Further observations to elucidate the role of interventricular dispersion of repolarization and early afterdepolarizations in the genesis of acquired torsade de pointes arrhythmias: A comparison between almokalant and d-sotalol using the dog as its own control. Journal of the American College of Cardiology, 30, 1575–1584.
Sugiyama, A., Nakamura, Y., Akie, Y., Saito, H., Izumi, Y., Yamazaki, H., et al. (2011). Microminipig, a non-rodent experimental animal optimized for life science research: In vivo proarrhythmia models of drug-induced long QT syndrome: Development of chronic atrioventricular block model of microminipig. Journal of the American College of Cardiology, 115, 122–126.
Sugiyama, A., Ishida, Y., Satoh, Y., Aoki, S., Hori, M., Akie, Y., et al. (2002). Electrophysiological, anatomical and histological remodeling of the heart to AV block enhances susceptibility to arrhythmogenic effects of QT-prolonging drugs. The Japanese Journal of Pharmacology, 88, 341–350.
Takahara, A., Sugiyama, A., Ishida, Y., Satoh, Y., Wang, K., Nakamura, Y., et al. (2006). Long-term bradycardia caused by atrioventricular block can remodel the canine heart to detect the histamine H1 blocker terfenadine-induced torsades de pointes arrhythmias. British Journal of Pharmacology, 147, 634–641.
Fridericia, L. S. (1920). Die Systolendauer im Elektrokardiogramm bei normalen Menschen und bei Herzkranken (in German). Acta Medica Scandinavica, 53, 469–486.
Satoh, T., & Zipes, D. P. (1996). Rapid rates during bradycardia prolong ventricular refractoriness and facilitate ventricular tachycardia induction with cesium in dogs. Circulation, 94, 217–227.
Goto, A., Izumi-Nakaseko, H., Hagiwara-Nagasawa, M., Chiba, K., Ando, K., Naito, A. T., et al. (2018). Analysis of torsadogenic and pharmacokinetic profile of E-4031 in dogs bridging the gap of information between in vitro proarrhythmia assay and clinical observation in human subjects. Journal of Pharmacological Sciences, 137, 237–240.
Lubna, N. J., Nakamura, Y., Hagiwara-Nagasawa, M., Goto, A., Chiba, K., Kitta, K., et al. (2018). Electropharmacological characterization of microminipigs as a laboratory animal using anti-influenza virus drug oseltamivir. The Journal of Toxicological Sciences, 43, 507–512.
Matsukura, S., Nakamura, Y., Cao, X., Wada, T., Izumi-Nakaseko, H., Ando, K., et al. (2017). Characterization of microminipigs as an in vivo experimental model for cardiac safety pharmacology. Journal of Pharmacological Sciences, 133, 103–109.
Sugiyama, A., Satoh, Y., Ishida, Y., Yoneyama, M., Yoshida, H., & Hashimoto, K. (2002). Pharmacological and electrophysiological characterization of junctional rhythm during radiofrequency catheter ablation of the atrioventricular node: possible involvement of neurotransmitters from autonomic nervous system. Circulation Journal, 66, 696–701.
Motomura, S., Iijima, T., Taira, N., & Hashimoto, K. (1975). Effects of neurotransmitters injected into the posterior and the anterior septal artery on the automaticity of the atrioventricular junctional area of the dog heart. Circulation Research, 37, 146–155.
Wada, T., Ohara, H., Nakamura, Y., Cao, X., Izumi-Nakaseko, H., Ando, K., et al. (2017). Efficacy of precordial percussion pacing assessed in a cardiac standstill microminipig model. Circulation Journal, 81, 1137–1143.
Acknowledgements
The authors thank Dr. Yuji Nakamura, Dr. Yasuki Akie, Mr. Hiroyuki Saito and Mrs. Yuri Ichikawa for their technical assistance.
Funding
This study was supported in part by Japan agency for medical research and development (AMED Grant #AS2116907E; #18mk0104117j0001) and Japan society for the promotion of science (JSPS KAKENHI Grant Number JP16K08559).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors indicated no potential conflict of interest.
Ethical Approval
All experiments were planned based upon the rules and regulations of the Committee for Research at Yamanashi Research Center of Clinical Pharmacology (#2009-04) and Toho University Animal Care and User Committee (#17-52-323), and performed in accordance with the Guidelines for the Care and Use of Laboratory Animals of both facilities.
Additional information
Handling Editor: Yu-Ming Kang.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goto, A., Hagiwara-Nagasawa, M., Kambayashi, R. et al. Measurement of J–Tpeakc along with QT-Interval Prolongation May Increase the Assay Sensitivity and Specificity for Predicting the Onset of Drug-Induced Torsade de Pointes: Experimental Evidences Based on Proarrhythmia Model Animals. Cardiovasc Toxicol 19, 357–364 (2019). https://doi.org/10.1007/s12012-019-09506-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-019-09506-z