Abstract
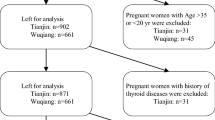
Pregnant women are more vulnerable to iodine deficiency and iodine excess. The study aimed to assess the changes in iodine nutrition and thyroid function of pregnant women exposed to different iodine sources resulting in various iodine intakes during pregnancy. From 2016 to 2017, 2004 healthy pregnant women aged 20–35 years from Shandong and Tianjin, China, were enrolled. Urinary iodine concentration (UIC), drinking water iodine content (WIC), thyroid-stimulating hormone (TSH), free triiodothyronine (FT3), free thyroid hormone (FT4), thyroglobulin (Tg), serum thyroid peroxidase antibody (TPOAb), and thyroglobulin antibody (TgAb) were measured. Pregnant women in both Shandong and Tianjin were iodine sufficient, but the median UIC in pregnant women was significantly higher in Shandong (244 μg/L) than that in Tianjin (159 μg/L). No differences were found in UIC over the course of gestation in Shandong. In Tianjin, the UIC decreased during 13–24 weeks and stabilized thereafter. Compared with Tianjin, TSH levels were higher and FT3 and FT4 levels were lower in Shandong. Both FT3 and FT4 significantly decreased during pregnancy in Shandong and Tianjin. TSH and Tg increased over the course of gestation in both Shandong and Tianjin. The iodine status of pregnant women in Tianjin and Shandong were sufficient, but different changing patterns in UIC and thyroid function during pregnancy were presented. More attention should be focused on iodine nutrition of pregnant women, even in iodine-sufficient areas.



Similar content being viewed by others
References
Glinoer D (2004) The regulation of thyroid function during normal pregnancy: importance of the iodine nutrition status. Best Pract Res Clin Endocrinol Metab 18(2):133–152. https://doi.org/10.1016/j.beem.2004.03.001
Abel MH, Caspersen IH (2017) Suboptimal maternal iodine intake is associated with impaired child neurodevelopment at 3 years of age in the Norwegian mother and child cohort study. J Nutr 147(7):1314–1324. https://doi.org/10.3945/jn.117.250456
Hynes KL, Otahal P, Hay I, Burgess JR (2013) Mild iodine deficiency during pregnancy is associated with reduced educational outcomes in the offspring: 9-year follow-up of the gestational iodine cohort. J Clin Endocrinol Metab 98(5):1954–1962. https://doi.org/10.1210/jc.2012-4249
Bath SC, Steer CD, Golding J, Emmett P, Rayman MP (2013) Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 382(9889):331–337. https://doi.org/10.1016/s0140-6736(13)60436-5
Mills JL, Buck Louis GM, Kannan K, Weck J, Wan Y, Maisog J, Giannakou A, Wu Q, Sundaram R (2018) Delayed conception in women with low-urinary iodine concentrations: a population-based prospective cohort study. Hum Reprod 33(3):426–433. https://doi.org/10.1093/humrep/dex379
Swanson CA, Zimmermann MB, Skeaff S, Pearce EN, Dwyer JT, Trumbo PR, Zehaluk C, Andrews KW, Carriquiry A, Caldwell KL, Egan SK, Long SE, Bailey RL, Sullivan KM, Holden JM, Betz JM, Phinney KW, Brooks SP, Johnson CL, Haggans CJ (2012) Summary of an NIH workshop to identify research needs to improve the monitoring of iodine status in the United States and to inform the DRI. J Nutr 142(6):1175s–1185s. https://doi.org/10.3945/jn.111.156448
Nishiyama S, Mikeda T, Okada T, Nakamura K, Kotani T, Hishinuma A (2004) Transient hypothyroidism or persistent hyperthyrotropinemia in neonates born to mothers with excessive iodine intake. Thyroid 14(12):1077–1083. https://doi.org/10.1089/thy.2004.14.1077
Sang Z, Wei W, Zhao N, Zhang G, Chen W, Liu H, Shen J, Liu J, Yan Y, Zhang W (2012) Thyroid dysfunction during late gestation is associated with excessive iodine intake in pregnant women. J Clin Endocrinol Metab 97(8):E1363–E1369. https://doi.org/10.1210/jc.2011-3438
Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB (2016) Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr 104(Suppl 3):918s–923s. https://doi.org/10.3945/ajcn.115.110429
Shi X, Han C, Li C, Mao J, Wang W, Xie X, Li C, Xu B, Meng T, Du J, Zhang S, Gao Z, Zhang X, Fan C, Shan Z, Teng W (2015) Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7190 pregnant women in China. J Clin Endocrinol Metab 100(4):1630–1638. https://doi.org/10.1210/jc.2014-3704
WHO/UNICEF/ICCIDD (2007) Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programs managers, 3rd edn. World Health Organization, Geneva http://www.ign.org/p142003094.html
Sang Z, Wang PP, Yao Z, Shen J, Halfyard B, Tan L, Zhao N, Wu Y, Gao S, Tan J, Liu J, Chen Z, Zhang W (2012) Exploration of the safe upper level of iodine intake in euthyroid Chinese adults: a randomized double-blind trial. Am J Clin Nutr 95(2):367–373. https://doi.org/10.3945/ajcn.111.028001
Sang Z, Chen W, Shen J, Tan L, Zhao N, Liu H, Wen S, Wei W, Zhang G, Zhang W (2013) Long-term exposure to excessive iodine from water is associated with thyroid dysfunction in children. J Nutr 143(12):2038–2043. https://doi.org/10.3945/jn.113.179135
Tan L, Sang Z, Shen J, Liu H, Chen W, Zhao N, Wei W, Zhang G, Zhang W (2015) Prevalence of thyroid dysfunction with adequate and excessive iodine intake in Hebei Province, People’s Republic of China. Public Health Nutr 18(9):1692–1697. https://doi.org/10.1017/s1368980014002237
Chen W, Zhang Y, Hao Y, Wang W, Tan L, Bian J, Pearce EN, Zimmermann MB, Shen J, Zhang W (2018) Adverse effects on thyroid of Chinese children exposed to long-term iodine excess: optimal and safe tolerable upper intake levels of iodine for 7- to 14-y-old children. Am J Clin Nutr 107(5):780–788. https://doi.org/10.1093/ajcn/nqy011
Liu P, Su X, Shen H, Meng F, Fan L, Liu S, Sun D (2015) National iodine deficiency disorders: an analysis of surveillance data in 2011, vol 34. https://doi.org/10.3760/cma.j.issn.2095-4255.2015.03.008
Yan Y, Dong Z, Dong L, Wang F, Yang X, Jin X, Lin L, Sun Y, Chen Z (2011) Trimester- and method-specific reference intervals for thyroid tests in pregnant Chinese women: methodology, euthyroid definition and iodine status can influence the setting of reference intervals. Clin Endocrinol 74(2):262–269. https://doi.org/10.1111/j.1365-2265.2010.03910.x
Rohner F, Zimmermann M, Jooste P, Pandav C, Caldwell K, Raghavan R, Raiten DJ (2014) Biomarkers of nutrition for development--iodine review. J Nutr 144(8):1322s–1342s. https://doi.org/10.3945/jn.113.181974
Shen H, Liu S, Sun D, Zhang S, Su X, Shen Y, Han H (2011) Geographical distribution of drinking-water with high iodine level and association between high iodine level in drinking-water and goitre: a Chinese national investigation. Br J Nutr 106(2):243–247. https://doi.org/10.1017/s0007114511000055
Wu Y, Li X, Chang S, Liu L, Zou S, Hipgrave DB (2012) Variable iodine intake persists in the context of universal salt iodization in China. J Nutr 142(9):1728–1734. https://doi.org/10.3945/jn.112.157982
Knight BA, Shields BM, He X, Pearce EN, Braverman LE, Sturley R, Vaidya B (2017) Iodine deficiency amongst pregnant women in South-West England. Clin Endocrinol 86(3):451–455. https://doi.org/10.1111/cen.13268
Trumpff C, De Schepper J, Tafforeau J, Van Oyen H, Vanderfaeillie J, Vandevijvere S (2013) Mild iodine deficiency in pregnancy in Europe and its consequences for cognitive and psychomotor development of children: a review. J Trace Elem Med Biol 27(3):174–183. https://doi.org/10.1016/j.jtemb.2013.01.002
Fuse Y, Ohashi T, Yamaguchi S, Yamaguchi M, Shishiba Y, Irie M (2011) Iodine status of pregnant and postpartum Japanese women: effect of iodine intake on maternal and neonatal thyroid function in an iodine-sufficient area. J Clin Endocrinol Metab 96(12):3846–3854. https://doi.org/10.1210/jc.2011-2180
Kung AW, Lao TT, Chau MT, Tam SC, Low LC (2000) Goitrogenesis during pregnancy and neonatal hypothyroxinaemia in a borderline iodine sufficient area. Clin Endocrinol 53(6):725–731
Caldwell KL, Pan Y, Mortensen ME, Makhmudov A, Merrill L, Moye J (2013) Iodine status in pregnant women in the National Children’s Study and in U.S. women (15-44 years), National Health and Nutrition Examination Survey 2005-2010. Thyroid 23(8):927–937. https://doi.org/10.1089/thy.2013.0012
Kedir B, Berhane Y, Worku A (2014) Subclinical iodine deficiency among pregnant women in Haramaya District, Eastern Ethiopia: a community-based study. J Nutr Metab 2014(3):878926–878928. https://doi.org/10.1155/2014/878926
Habimana L, Twite KE, Wallemacq P, De Nayer P, Daumerie C, Donnen P, Kalenga MK, Robert A (2013) Iodine and iron status of pregnant women in Lubumbashi, Democratic Republic of Congo. Public Health Nutr 16(8):1362–1370. https://doi.org/10.1017/s1368980012005484
Azizi F, Aminorroya A, Hedayati M, Rezvanian H, Amini M, Mirmiran P (2003) Urinary iodine excretion in pregnant women residing in areas with adequate iodine intake. Public Health Nutr 6(1):95–98. https://doi.org/10.1079/PHN2002366
Smyth PP, Wijeyaratne CN, Kaluarachi WN, Smith DF, Premawardhana LD, Parkes AB, Jayasinghe A, de Silva DG, Lazarus JH (2005) Sequential studies on thyroid antibodies during pregnancy. Thyroid 15(5):474–477. https://doi.org/10.1089/thy.2005.15.474
De Zoysa E, Hettiarachchi M, Liyanage C (2016) Urinary iodine and thyroid determinants in pregnancy: a follow up study in Sri Lanka. BMC Pregnancy Childbirth 16(1):303. https://doi.org/10.1186/s12884-016-1093-7
Dworkin HJ, Jacquez JA, Beierwaltes WH (1966) Relationship of iodine ingestion to iodine excretion in pregnancy. J Clin Endocrinol Metab 26(12):1329–1342. https://doi.org/10.1210/jcem-26-12-1329
Chen W, Sang Z, Tan L, Zhang S, Dong F, Chu Z, Wei W, Zhao N, Zhang G, Yao Z, Shen J, Zhang W (2015) Neonatal thyroid function born to mothers living with long-term excessive iodine intake from drinking water. Clin Endocrinol 83(3):399–404. https://doi.org/10.1111/cen.12625
Han C, Li C, Mao J, Wang W, Xie X, Zhou W, Li C, Xu B, Bi L, Meng T, Du J, Zhang S, Gao Z, Zhang X, Yang L, Fan C, Teng W, Shan Z (2015) High body mass index is an indicator of maternal hypothyroidism, hypothyroxinemia, and thyroid-peroxidase antibody positivity during early pregnancy. Biomed Res Int 2015:351831–351837. https://doi.org/10.1155/2015/351831
Stricker R, Echenard M, Eberhart R, Chevailler MC, Perez V, Quinn FA, Stricker R (2007) Evaluation of maternal thyroid function during pregnancy: the importance of using gestational age-specific reference intervals. Eur J Endocrinol 157(4):509–514. https://doi.org/10.1530/eje-07-0249
Lambert-Messerlian G, McClain M, Haddow JE, Palomaki GE, Canick JA, Cleary-Goldman J, Malone FD, Porter TF, Nyberg DA, Bernstein P, D’Alton ME (2008) First- and second-trimester thyroid hormone reference data in pregnant women: a FaSTER (First- and Second-Trimester Evaluation of Risk for aneuploidy) esearch Consortium study. Am J Obstet Gynecol 199(1):62.e61–62.e66. https://doi.org/10.1016/j.ajog.2007.12.003
Xing J, Yuan E, Li J, Zhang Y, Meng X, Zhang X, Rong S, Lv Z, Tian Y, Jia L (2016) Trimester- and assay-specific thyroid reference intervals for pregnant women in China. Int J Endocrinol 2016:3754213. https://doi.org/10.1155/2016/3754213
Liu J, Yu X, Xia M, Cai H, Cheng G, Wu L, Li Q, Zhang Y, Sheng M, Liu Y, Qin X (2017) Development of gestation-specific reference intervals for thyroid hormones in normal pregnant Northeast Chinese women: what is the rational division of gestation stages for establishing reference intervals for pregnancy women? Clin Biochem 50(6):309–317. https://doi.org/10.1016/j.clinbiochem.2016.11.036
Kostecka-Matyja M, Fedorowicz A, Bar-Andziak E, Bednarczuk T, Buziak-Bereza M, Dumnicka P, Gorska M, Krasnodebska M, Niedzwiedzka B, Pach D, Ruchala M, Siewko K, Solnica B, Sowinski J, Szelachowska M, Trofimiuk-Muldner M, Wachowiak-Ochmanska K, Hubalewska-Dydejczyk A (2017) Reference values for TSH and free thyroid hormones in healthy pregnant women in Poland: a prospective, multicenter study. Eur Thyroid J 6(2):82–88. https://doi.org/10.1159/000453061
Glinoer D, de Nayer P, Bourdoux P, Lemone M, Robyn C, van Steirteghem A, Kinthaert J, Lejeune B (1990) Regulation of maternal thyroid during pregnancy. J Clin Endocrinol Metab 71(2):276–287. https://doi.org/10.1210/jcem-71-2-276
Liesenkotter KP, Gopel W, Bogner U, Stach B, Gruters A (1996) Earliest prevention of endemic goiter by iodine supplementation during pregnancy. Eur J Endocrinol 134(4):443–448
Soldin OP, Tractenberg RE, Hollowell JG, Jonklaas J, Janicic N, Soldin SJ (2004) Trimester-specific changes in maternal thyroid hormone, thyrotropin, and thyroglobulin concentrations during gestation: trends and associations across trimesters in iodine sufficiency. Thyroid 14(12):1084–1090. https://doi.org/10.1089/thy.2004.14.1084
Moleti M, Lo Presti VP, Campolo MC, Mattina F, Galletti M, Mandolfino M, Violi MA, Giorgianni G, De Domenico D, Trimarchi F, Vermiglio F (2008) Iodine prophylaxis using iodized salt and risk of maternal thyroid failure in conditions of mild iodine deficiency. J Clin Endocrinol Metab 93(7):2616–2621. https://doi.org/10.1210/jc.2008-0352
Zimmermann MB, Aeberli I, Andersson M, Assey V, Yorg JA, Jooste P, Jukic T, Kartono D, Kusic Z, Pretell E, San Luis TO Jr, Untoro J, Timmer A (2013) Thyroglobulin is a sensitive measure of both deficient and excess iodine intakes in children and indicates no adverse effects on thyroid function in the UIC range of 100-299 mug/L: a UNICEF/ICCIDD study group report. J Clin Endocrinol Metab 98(3):1271–1280. https://doi.org/10.1210/jc.2012-3952
Zhang X, Li C, Mao J, Wang W, Xie X, Peng S, Wang Z, Han C, Zhang X, Wang D, Fan C, Shan Z, Teng W (2017) Gestation-specific changes in maternal thyroglobulin during pregnancy and lactation in an iodine-sufficient region in China: a longitudinal study. Clin Endocrinol 86(2):229–235. https://doi.org/10.1111/cen.13175
Acknowledgements
We express our sincere thanks to all participants in our study, healthcare personnel at Tanggu Maternity Hospital, Gaoqing Center for Disease Control and Prevention and Child Health Hospital of Gaoqing for the assistance they offered in collecting biological samples in our study. Also, we acknowledge the Key Laboratory of Hormone and Development (Ministry of Health), Metabolic Diseases Hospital, and the Tianjin Institute of Endocrinology, Tianjin Medical University, for the measurement of urine and water sample, and the endocrinology department in Tianjin Medical University General Hospital for evaluating thyroid function and supporting professional advice.
Funding
This work was financially supported by the Key projects of Chinese National Natural Science Foundation (Grant no. 81330064) and Tianjin Science and Technology Committee Project Foundation (Grant no. 14ZCZDSY00022).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All research protocols were approved by the Medical Ethics Committee of Tianjin Medical University, and all procedures performed in the study were in accordance with the ethical standards of the committee and with the 1964 Helsinki declaration. All participants provided written informed consent after research protocols were carefully explained to them.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Chen, Y., Chen, W., Du, C. et al. Iodine Nutrition and Thyroid Function in Pregnant Women Exposed to Different Iodine Sources. Biol Trace Elem Res 190, 52–59 (2019). https://doi.org/10.1007/s12011-018-1530-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1530-8