Abstract
Purpose of review
The evolution of endpoints used to assess disease activity and treatment efficacy in inflammatory bowel disease (IBD) has accompanied changes in clinical trial methodology and the therapeutic landscape.
Recent findings
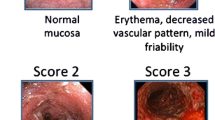
Composite and co-primary endpoints for patient-reported outcomes (without physician’s global assessment) and endoscopic improvement (excluding friability) are used to define clinical remission and clinical response in contemporary clinical trials for ulcerative colitis and Crohn’s disease. Histologic-endoscopic mucosal healing has emerged as a therapeutic goal and validated histological indexes are increasingly integrated into clinical trials. Central reading of endoscopy is recognized as the gold standard for endoscopic assessment in clinical trials to minimize observer bias and inter-observer variability.
Summary
Determination of treatment efficacy in IBD has evolved to incorporate both patient-reported outcome measures and central reading of endoscopy +/- histology as composite endpoints in contemporary clinical trials.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Turner D et al., “STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD,” Gastroenterology, 2021/02/19/ 2021, doi: 10.1053/j.gastro.2020.12.031. An evidence-based international expert consensus recommendations from the International Organization for the Study of Inflammatory Bowel Diseases (IOIBD) for treat-to-target strategies in adults and children with IBD.
•• Le Berre C et al., “Selecting endpoints for disease-modification trials in inflammatory bowel disease: the SPIRIT consensus from the IOIBD,” Gastroenterology, 2021/01/06/ 2021, doi: 10.1053/j.gastro.2020.10.065. An evidence-based international expert consensus recommendations from the International Organization for the Study of Inflammatory Bowel Diseases (IOIBD) for the selection of endpoints to be used in future IBD-disease modification trials.
Ungaro R, Colombel JF, Lissoos T, and Peyrin-Biroulet L, “A treat-to-target update in ulcerative colitis: a systematic review,” (in eng), Am J Gastroenterol, vol. 114, no. 6, pp. 874-883, Jun 2019, doi: 10.14309/ajg.0000000000000183.
Abreu MT and Sandborn WJ, “Defining endpoints and biomarkers in inflammatory bowel disease: moving the needle through clinical trial design,” (in eng), Gastroenterology, vol. 159, no. 6, pp. 2013-2018.e7, Dec 2020, doi: 10.1053/j.gastro.2020.07.064.
B. E. Sands et al., “The impact of raising the bar for clinical trials in ulcerative colitis,” (in eng), J Crohns Colitis, vol. 13, no. 9, pp. 1217-1226, Sep 19 2019, doi: 10.1093/ecco-jcc/jjz038.
Food and Drug Administration. (2016). FDA-2016-D-2319, Ulcerative Colitis: Clinical Trial Endpoints Guidance for Industry Draft Guidance. [Online] Available: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/ulcerative-colitis-clinical-trial-endpoints-guidance-industry
•• European Medicines Agency. (2018). Guideline on the development of new medicinal products for the treatment of ulcerative colitis. [Online] Available: https://www.ema.europa.eu/en/development-new-medicinal-products-treatment-ulcerative-colitis. Guidance for the design of clincial studies (including primary/secondary endpoints, labelling claims) for ulcerative colitis from the European Union’s regulatory agency for the scientific evaluation, supervisition, and approval of medicines in the European Union.
•• European Medicines Agency. (2018). Guideline on the development of new medicinal products for the treatment of Crohn’s disease. [Online] Available: https://www.ema.europa.eu/en/clinical-investigation-medicinal-products-management-crohns-disease. Guidance for the design of clincial studies (including primary/secondary endpoints, labelling claims) for Crohn’s disease from the European Union’s regulatory agency for the scientific evaluation, supervisition, and approval of medicines in the European Union.
Catt H, Hughes D, Kirkham JJ, Bodger K. Systematic review: outcomes and adverse events from randomised trials in Crohn’s disease (in eng). Aliment Pharmacol Ther. Apr 2019;49(8):978–96. https://doi.org/10.1111/apt.15174.
Ma C et al., “Heterogeneity in definitions of efficacy and safety endpoints for clinical trials of Crohn’s disease: a systematic review,” (in eng), Clin Gastroenterol Hepatol, vol. 16, no. 9, pp. 1407-1419.e22, Sep 2018, doi: 10.1016/j.cgh.2018.02.051.
• Ma C et al., “An international consensus to standardize integration of histopathology in ulcerative colitis clinical trials,” (in eng), Gastroenterology, Feb 18 2021, doi: 10.1053/j.gastro.2021.02.035. An evidence-based international conensus from expert gastroenterlogists and gastrointestinal pathologists on the standardized biopsy collection protocols and optimal histologic indices (including thresholds) for evaluating for histologic response and remission in clincial trials.
• Magro F et al., “ECCO position paper: harmonization of the approach to ulcerative colitis histopathology,” (in eng), J Crohns Colitis, vol. 14, no. 11, pp. 1503-1511, Nov 7 2020, doi: 10.1093/ecco-jcc/jjaa110. An evidence-based expert consensus from the European Crohn’s and Colitis Organisation on the procedures, definitions, and scoring systems for assessing ulcerative colitis histopathology in clinical trials and clinical practice.
Schroeder KW, Tremaine WJ, and Ilstrup DM, “Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study,” (in eng), N Engl J Med, vol. 317, no. 26, pp. 1625-9, Dec 24 1987, doi: 10.1056/nejm198712243172603.
Feagan BG et al., “A15 efficacy and safety of filgotinib as induction therapy for patients with moderately to severely active ulcerative colitis: results from the phase 2b/3 selection study,” Journal of the Canadian Association of Gastroenterology, vol. 4, no. Supplement_1, pp. 18-20, 2021, doi: 10.1093/jcag/gwab002.014.
Feagan BGL, Jr EV, Danese S, Vermeire S, Sandborn WJ, Ritter T, Mehta R, Seidler U, Seibold F, Beales I, Kim HK, McNally J, Yun C, Zhao S, Liu X, Tasset C, Besuyen R, Watanabe M, Schreiber S, Rogler G, Hibi T, Peyrin-Biroulet L., “Abstracts: LB20 Efficacy and safety of filgotinib as induction therapy for patients with moderately to severely active ulcerative colitis: Results from the Phase IIB/III SELECTION study,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
Peyrin-Biroulet L et al., “A17 efficacy and safety of filgotinib as maintenance therapy for patients with moderately to severely active ulcerative colitis: results from the phase 2b/3 selection study,” Journal of the Canadian Association of Gastroenterology, vol. 4, no. Supplement_1, pp. 21-23, 2021, doi: 10.1093/jcag/gwab002.016.
Peyrin-Biroulet LL, Jr EV, Danese S, Vermeire S, Sandborn WJ, Fogel R, Nijhawan S, Kempinski R, Filip R, Hospodarskyy I, McNally J, Yun C, Zhao S, Liu X, Tasset C, Besuyen R, Watanabe M, Schreiber S, Rogler G, Hibi T, Feagan BG, “Abstracts: LB19 efficacy and safety of filgotinib as maintenance therapy for patients with moderately to severely active ulcerative colitis: results from the Phase IIB/III SELECTION study,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
Atreya R, et al. Cobitolimod for moderate-to-severe, left-sided ulcerative colitis (CONDUCT): a phase 2b randomised, double-blind, placebo-controlled, dose-ranging induction trial, (in eng). Lancet Gastroenterol Hepatol. Dec 2020;5(12):1063–75. https://doi.org/10.1016/s2468-1253(20)30301-0.
Sandborn WJ, et al. Efficacy and safety of etrasimod in a phase 2 randomized trial of patients with ulcerative colitis (in eng). Gastroenterology. Feb 2020;158(3):550–61. https://doi.org/10.1053/j.gastro.2019.10.035.
Vermeire S et al., “Long-term safety and efficacy of etrasimod for ulcerative colitis: results from the open-label extension of the OASIS study,” (in eng), J Crohns Colitis, Jan 21 2021, doi: https://doi.org/10.1093/ecco-jcc/jjab016.
Sandborn WJ et al., “Efficacy and safety of mirikizumab in a randomized phase 2 study of patients with ulcerative colitis,” (in eng), Gastroenterology, vol. 158, no. 3, pp. 537-549.e10, Feb 2020, doi: 10.1053/j.gastro.2019.08.043.
Sandborn WJ et al., “Efficacy and safety of continued treatment with mirikizumab in a phase 2 trial of patients with ulcerative colitis,” (in eng), Clin Gastroenterol Hepatol, Sep 18 2020, doi: https://doi.org/10.1016/j.cgh.2020.09.028.
Danese SFBG, Wolf DC, Hanauer SB, Jovanovic I, Ghosh S, Petersen A, Hua SY, Lee JH, Charles L, Chitkara D, Sandborn WJ, D’Haens D, “Abstracts LB10 Ozanimod as maintenance therapy in patients with moderate-to-severe ulcerative colitis: results from the Phase III, randomized, double-blind, placebo-controlled True North study,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
Feagan BG, et al. Ozanimod induction therapy for patients with moderate to severe Crohn’s disease: a single-arm, phase 2, prospective observer-blinded endpoint study. The Lancet Gastroenterology & Hepatology. 2020;5(9):819–28.
Sandborn WJHGR, Wolf DC, Hanauer SB, Jovanovic I, Ghosh S, Petersen A, Hua SY, Lee JH, Charles L, Usiskin K, Danese S, Feagan BG, “Abstracts LB02 ozanimod as induction therapy in moderate-to-severe ulcerative colitis: results from the phase III, randomized, double-blind, placebo-controlled True North study,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
Sandborn WJ et al., “Efficacy of upadacitinib in a randomized trial of patients with active ulcerative colitis,” (in eng), Gastroenterology, vol. 158, no. 8, pp. 2139-2149.e14, Jun 2020, doi: 10.1053/j.gastro.2020.02.030.
W. J. Sandborn, ed, 2021.
Danese SCJF, Lukas M, Gisbert JP, D’Haens G, Hayee B, Pannacione R, Kim HK, Reinisch W, Tyrrell H, Oh YS, Tole S, Chai A, Chamberlain-James K, Tang MT, Schreiber S the GARDENIA Study Group, “Abstracts LB01 Etrolizumab versus infliximab for treating patients 35RASpberry809 with moderately to severely active ulcerative colitis: results from the Phase III GARDENIA study,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
Dotan IPJ, Duvall A; Bouhnik Y, Radford-Smith G, Higgins PDR, Mishkin DS, Arrisi P, Scalori A, Oh YS, Tole S, Chai A, Chamberlain-James K, Lacey S, MccBride J, Rubin DT, HIBISCUS I and II Study Group, “Abstracts LB09 Etrolizumab compared with adalimumab or placebo as induction therapy for ulcerative colitis: results from the randomized, phase III HIBISCUS I and II trials I,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
Peyrin-Biroulet LHAL, Bossuyt P, Long, M., Allez M, Juillerat P, Armuzzi A, Loftus EV Jr, Ostad-Saffari E, Scalori A, Oh YS, Tole S, Chai A, Pulley J, Lacey S, Sandborn WJ, on behalf of the HICKORY Study Group, “Abstracts LB08 Etrolizumab as induction and maintenance therapy in patients with ulcerative colitis previously exposed to anti-tumor necrosis factor agent: the randomized, Phase III HICKORY trial,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
•• Sandborn WJ et al., “Etrolizumab for the treatment of ulcerative colitis and Crohn’s disease: an overview of the phase 3 clinical program,” (in eng), Adv Ther, vol. 37, no. 7, pp. 3417-3431, Jul 2020, doi: 10.1007/s12325-020-01366-2. A overview of the largest and most comprehensive phase 3 clinical trial of a novel pharmacologic agent in inflammatory bowel disease to date.
Vermeire SLPL, Ritter T, Hanauer S, Bressler B, Khanna R, Isaacs K, Shah S, Kadva AK, Tyrrell H, Oh YS, Tole S, Chai A, Pulley J, Zhang W, Feagan BG, on behalf of the LAUREL Study Group, “Abstracts: LB18 etrolizumab versus placebo in tumor necrosis factor antagonist naive patients with ulcerative colitis: results from the randomized Phase III LAUREL trial,” in United European Gastroenterology Journal, 2020, vol. 8, no. 10: SAGE Publications, 2020/12/04 ed., pp. 1258-1275, doi: 10.1177/2050640620968709. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724535/
Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s Disease Activity Index. National Cooperative Crohn’s Disease Study (in eng). Gastroenterology. Mar 1976;70(3):439–44.
de Jong MJ, Huibregtse R, Masclee AAM, Jonkers D, Pierik MJ, “Patient-reported outcome measures for use in clinical trials and clinical practice in inflammatory bowel diseases: a systematic review,” (in eng), Clin Gastroenterol Hepatol, vol. 16, no. 5, pp. 648-663.e3, May 2018, doi: 10.1016/j.cgh.2017.10.019.
Danese S et al., “Endoscopic, radiologic, and histologic healing with vedolizumab in patients with active Crohn’s disease,” (in eng), Gastroenterology, vol. 157, no. 4, pp. 1007-1018.e7, Oct 2019, doi: 10.1053/j.gastro.2019.06.038.
Ferrante M et al., “OP27 long-term safety and efficacy of risankizumab treatment in patients with Crohn’s disease: final results from the phase 2 open-label extension study,” Journal of Crohn's and Colitis, vol. 14, no. Supplement_1, pp. S024-S025, 2020, doi: 10.1093/ecco-jcc/jjz203.026.
Lowenberg M et al., “Vedolizumab induces endoscopic and histologic remission in patients with Crohn’s disease,” Gastroenterology, vol. 157, no. 4, pp. 997-1006 e6, Oct 2019, doi: 10.1053/j.gastro.2019.05.067.
Sandborn DJWJ, Chan J, Lang G, Adedokun OJ, Afzali A, Andrews JM, D’Haens G, Danese S, Hisamatsu T, Panaccione RPJ, Reinisch WRDT, Sands BE; Feagan B.G.13, on behalf of the GALAXI 1 Investigators, “OP089 The efficacy and safety of guselkumab induction therapy in patients with moderately to severely active Crohn’s disease: week 12 interim analyses from the phase 2 GALAXI 1 study,” in United European Gastroenterology 2020, vol. 8, no. S8: United European Gastroenterology Journal, pp. 8-142, doi: 10.1177/2050640620927344. [Online]. Available: https://onlinelibrary.wiley.com/doi/abs/10.1177/2050640620927344
Sands BESWJ, Peyrin-Biroulet L, Higgins P, Hirai F, Jairath V, D'Haens G, Abreu MT, Belin R, Gomez E, Valderas G, Miller D, Naegeli A, Arora V, Pollack P, Tuttle J, Hibi T, “OP108 efficacy and safety of mirikizumab after 52-weeks maintenance treatment in patients with moderate-to-severe Crohn’s disease,” in United European Gastroenterology, 2020, vol. 8, no. S8: United European Gastroenterology Journal, pp. 8-142, doi: 10.1177/2050640620927344. [Online]. Available: https://onlinelibrary.wiley.com/doi/abs/10.1177/2050640620927344
Khanna R, et al. A retrospective analysis: the development of patient reported outcome measures for the assessment of Crohn’s disease activity, (in eng). Alimentary pharmacology & therapeutics. Jan 2015;41(1):77–86. https://doi.org/10.1111/apt.13001.
Dulai PS, et al. Development of the symptoms and impacts questionnaire for Crohn's disease and ulcerative colitis. Alimentary Pharmacology & Therapeutics. 2020;51(11):1047–66. https://doi.org/10.1111/apt.15726.
• Higgins PDR et al., “Development and validation of the Crohn’s disease Patient-Reported Outcomes Signs and Symptoms (CD-PRO/SS) diary,” Journal of Patient-Reported Outcomes, vol. 2, no. 1, p. 24, 2018/05/09 2018, doi: 10.1186/s41687-018-0044-7. A novel patient-reported outcome measure to assess treatment efficacy in Crohn’s disease that was developed in accordance to the updated international regulatory agencies’ guidance for registration of new medicinal products for Crohn’s disease.
• P. D. R. Higgins et al., “Development and validation of the ulcerative colitis Patient-Reported Outcomes Signs and Symptoms (UC-pro/SS) diary,” Journal of Patient-Reported Outcomes, vol. 2, no. 1, p. 26, 2018/05/30 2018, doi: 10.1186/s41687-018-0049-2. A novel patient-reported outcome measure to assess treatment efficacy in ulcerative colitis that was developed in accordance to the updated international regulatory agencies’ guidance for registration of new medicinal products for ulcerative colitis.
European Medicines Agency. (2019). EMA/262838/2018, Letter of Support for the development of Patient-Reported Outcomes tools for use as an endpoint in Inflammatory Bowel Disease (IBD) clinical trials. [Online] Available: https://www.ema.europa.eu/en/documents/other/letter-support-development-patient-reported-outcomes-tools-use-endpoint-inflammatory-bowel-disease_en.pdf
D. K.P.D.R. Higgins and H. A.R. Jacob; Sharafali Z., Oh Y.S., Matsui A., “OP103 responder definitions for the Crohn’s Disease Patient-Reported Outcomes Signs and Symptoms (CD-PRO/ SS) tool using patients with Crohn’s disease treated with etrolizumab,” United European Gastroenterol J, UEG Week 2019 Oral Presentations vol. 7, no. 8_suppl, pp. 10-188, 2019/10/01 2019, doi: https://doi.org/10.1177/2050640619854670.
P. Higgins et al., “P224 responder definitions for the ulcerative colitis Patient-Reported Outcomes Signs and Symptoms (UC-PRO/SS) tool using patients with ulcerative colitis treated with etrolizumab,” Journal of Crohn’s and Colitis, vol. 13, no. Supplement_1, pp. S208-S209, 2019, doi: 10.1093/ecco-jcc/jjy222.348.
Sands BE, et al. Ustekinumab as induction and maintenance therapy for ulcerative colitis. New England Journal of Medicine. 2019;381(13):1201–14. https://doi.org/10.1056/NEJMoa1900750.
G. R. Lichtenstein et al., “704 tofacitinib, an oral Janus kinase inhibitor, in the treatment of ulcerative colitis: an interim analysis of an open-label, long-term extension study with up to 5.5 years of treatment,” in Am J Gastroenterol, 2019, vol. 114, pp. S413-S414.
Sandborn WJ, et al. Safety of tofacitinib for treatment of ulcerative colitis, based on 4.4 years of data from global clinical trials, (in eng). Clin Gastroenterol Hepatol. Jul 2019;17(8):1541–50. https://doi.org/10.1016/j.cgh.2018.11.035.
W. J. Sandborn et al., “Efficacy and safety of extended induction with tofacitinib for the treatment of ulcerative colitis. LID - S1542-3565(20)31496-8 [pii] LID - 10.1016/j.cgh.2020.10.038 [doi],” (in eng), Clin Gastroenterol Hepatol, no. 1542-7714 (Electronic), 2020.
B. E. Sands et al., “Peficitinib, an oral Janus kinase inhibitor, in moderate-to-severe ulcerative colitis: results from a randomised, phase 2 study,” (in eng), J Crohns Colitis, vol. 12, no. 10, pp. 1158-1169, Nov 9 2018, doi: 10.1093/ecco-jcc/jjy085.
Lobatón T, et al. Prognostic value of histological activity in patients with ulcerative colitis in deep remission: a prospective multicenter study, (in eng). United European Gastroenterol J. Jun 2018;6(5):765–72. https://doi.org/10.1177/2050640617752207.
M. Fumery, S. Singh, P. S. Dulai, C. Gower-Rousseau, L. Peyrin-Biroulet, and W. J. Sandborn, “Natural history of adult ulcerative colitis in population-based cohorts: a systematic review,” (in eng), Clin Gastroenterol Hepatol, vol. 16, no. 3, pp. 343-356.e3, Mar 2018, doi: 10.1016/j.cgh.2017.06.016.
Yvellez OV et al., “Cumulative histologic inflammation predicts colorectal neoplasia in ulcerative colitis: a validation study,” (in eng), Inflamm Bowel Dis, vol. 27, no. 2, pp. 203-206, Jan 19 2021, doi: 10.1093/ibd/izaa047.
Geboes K, Riddell R, Öst A, Jensfelt B, Persson T, Löfberg R. A reproducible grading scale for histological assessment of inflammation in ulcerative colitis. Gut. 2000;47(3):404–9. https://doi.org/10.1136/gut.47.3.404.
Marchal-Bressenot A, et al. Development and validation of the Nancy histological index for UC (in eng). Gut. Jan 2017;66(1):43–9. https://doi.org/10.1136/gutjnl-2015-310187.
Mosli MH, et al. Development and validation of a histological index for UC, (in eng). Gut. Jan 2017;66(1):50–8. https://doi.org/10.1136/gutjnl-2015-310393.
Daperno M, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD, (in eng). Gastrointest Endosc. Oct 2004;60(4):505–12. https://doi.org/10.1016/s0016-5107(04)01878-4.
Novak G et al., “Histologic scoring indices for evaluation of disease activity in Crohn’s disease,” (in eng), Cochrane Database Syst Rev, vol. 7, no. 7, p. Cd012351, Jul 21 2017, doi: 10.1002/14651858.CD012351.pub2.
Feagan BG, et al. Risankizumab in patients with moderate to severe Crohn’s disease: an open-label extension study. Lancet Gastroenterol Hepatol. Oct 2018;3(10):671–80. https://doi.org/10.1016/S2468-1253(18)30233-4.
Li K et al., “Effects of ustekinumab on histologic disease activity in patients with Crohn’s disease,” (in eng), Gastroenterology, vol. 157, no. 4, pp. 1019-1031.e7, Oct 2019, doi: 10.1053/j.gastro.2019.06.037.
D'Haens G, et al. Endoscopic and histological healing with infliximab anti-tumor necrosis factor antibodies in Crohn’s disease: a European multicenter trial, (in eng). Gastroenterology. May 1999;116(5):1029–34. https://doi.org/10.1016/s0016-5085(99)70005-3.
Ma C, et al. Systematic review with meta-analysis: endoscopic and histologic placebo rates in induction and maintenance trials of ulcerative colitis, (in eng). Aliment Pharmacol Ther. Jun 2018;47(12):1578–96. https://doi.org/10.1111/apt.14672.
Macaluso FS, Maida M, Ventimiglia M, Renna S, Cottone M, and Orlando A, “Factors affecting clinical and endoscopic outcomes of placebo arm in trials of biologics and small molecule drugs in ulcerative colitis: a meta-analysis,” (in eng), Inflamm Bowel Dis, vol. 25, no. 6, pp. 987-997, May 4 2019, doi: 10.1093/ibd/izy365.
Gottlieb K, et al. Endoscopy and central reading in inflammatory bowel disease clinical trials: achievements, challenges and future developments. Gut. 2021;70(2):418–26. https://doi.org/10.1136/gutjnl-2020-320690.
Reinisch W et al., “Long-term safety and efficacy of the anti-MAdCAM-1 monoclonal antibody ontamalimab (SHP647) for the treatment of ulcerative colitis: the open-label study TURANDOT II,” (in eng), J Crohns Colitis, Feb 18 2021, doi: https://doi.org/10.1093/ecco-jcc/jjab023.
Sandborn WJ et al., “Efficacy and safety of upadacitinib in a randomized trial of patients with Crohn’s disease,” (in eng), Gastroenterology, vol. 158, no. 8, pp. 2123-2138.e8, Jun 2020, doi: 10.1053/j.gastro.2020.01.047.
Jairath V, et al. Responsiveness of histological disease activity indices in ulcerative colitis: a post hoc analysis using data from the TOUCHSTONE randomised controlled trial (in eng). Gut. Jul 2019;68(7):1162–8. https://doi.org/10.1136/gutjnl-2018-316702.
Selinger C et al., “OTU-003 Etrolizumab as induction therapy in moderate to severe crohn’s disease: results from bergamot cohort 1,” Gut, vol. 67, no. Suppl 1, pp. A53-A53, 2018, doi: 10.1136/gutjnl-2018-BSGAbstracts.106.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Chung Sang Tse has no conflicts to disclose. Vipul Jairath has received consulting fees from AbbVie, Eli Lilly, GlaxoSmithKline, Arena Pharmaceuticals, Genetech, Pendopharm, Sandoz, Merck, Takeda, Janssen, Robarts Clinical Trials, Topivert, Celltrion; and speaker’s fees from Takeda, Janssen, Shire, Ferring, AbbVie, and Pfizer. Brian Feagan has received grant/research support from Millennium Pharmaceuticals, Merck, Tillotts Pharma AG, AbbVie, Novartis Pharmaceuticals, Centocor Inc, Elan/Biogen, UCB Pharma, Bristol-Myers Squibb, Genentech, ActoGenix, and Wyeth Pharmaceuticals Inc.; consulting fees from Millennium Pharmaceuticals, Merck, Centocor Inc, Elan/Biogen, Janssen-Ortho, Teva Pharmaceuticals, Bristol-Myers Squibb, Celgene, UCB Pharma, AbbVie, Astra Zeneca, Serono, Genentech, Tillotts Pharma AG, Unity Pharmaceuticals, Albireo Pharma, Given Imaging Inc., Salix Pharmaceuticals, Novonordisk, GSK, Actogenix, Prometheus Therapeutics and Diagnostics, Athersys, Axcan, Gilead, Pfizer, Shire, Wyeth, Zealand Pharma, Zyngenia, GiCare Pharma Inc., and Sigmoid Pharma; and speaker’s fees from UCB, AbbVie, and J&J/Janssen. William Sandborn has received research grant support from Atlantic Healthcare Limited, Amgen, Genentech, Gilead Sciences, AbbVie, Janssen, Takeda, Lilly, and Celgene/Receptos; consulting fees from Abbvie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Conatus, Cosmo, Escalier Biosciences, Ferring, Genentech, Gilead, Gossamer Bio, Janssen, Lilly, Miraca Life Sciences, Nivalis Therapeutics, Novartis Nutrition Science Partners, Oppilan Pharma, Otsuka, Paul Hastings, Pfizer, Precision IBD, Progenity, Prometheus Laboratories, Ritter Pharmaceuticals, Robarts Clinical Trials (owned by Health Academic Research Trust or HART), Salix, Shire, Seres Therapeutics, Sigmoid Biotechnologies, Takeda, Tigenix, Tillotts Pharma, UCB Pharma, and Vivelix; and stock options from Ritter Pharmaceuticals, Oppilan Pharma, Escalier Biosciences, Gossamer Bio, Precision IBD, and Progenity.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tse, C.S., Jairath, V., Feagan, B.G. et al. Updates in Clinical, Endoscopic, and Histologic Composite and Co-primary Endpoints for Clinical Trials in Inflammatory Bowel Disease. Curr Treat Options Gastro 19, 608–627 (2021). https://doi.org/10.1007/s11938-021-00362-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-021-00362-x