Abstract
Purpose of review
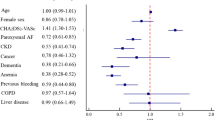
Atrial fibrillation (AF) is a growing health problem worldwide. While the disease plagues both men and women, this arrhythmia does not affect both sexes equally. Women are more likely to have major adverse outcomes such as stroke and its sequela; however, recent data on stroke prevention show improving outcomes. The purpose of this review of the recent literature is to summarize important updates on risk scores and management of patients with AF.
Recent findings
It has been well known that women have a higher risk of strokes than men when untreated or when treated with warfarin. Current risk scores emphasizing new risk factors such as the higher risk of strokes in women have been incorporated into clinical guidelines. However, with the use of direct oral anticoagulants, this sex disparity on stroke is no longer seen and women have less major bleeding than men. The use of cardiac glycosides is associated with increased incidence of breast cancer, and this medication is used more in women. Procedural complications for the management of AF are higher in women.
Summary
The study of the pathophysiology of AF and its management is a rapidly evolving area of cardiovascular medicine. Sex-specific data is necessary to achieve advances in the field and improve the outcomes in both men and women.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013;112(8):1142–7. https://doi.org/10.1016/j.amjcard.2013.05.063.
Benjamin EJ, Virani SS, Callaway CW, Chang AR, Cheng S, Chiuve SE, et al. Heart disease and stroke Statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. https://doi.org/10.1161/cir.0000000000000558.
Schnabel RB, Pecen L, Ojeda FM, Lucerna M, Rzayeva N, Blankenberg S, et al. Gender differences in clinical presentation and 1-year outcomes in atrial fibrillation. Heart. 2017;103(13):1024–30. https://doi.org/10.1136/heartjnl-2016-310406.
Ko D, Rahman F, Martins MA, Hylek EM, Ellinor PT, Schnabel RB, et al. Atrial fibrillation in women: treatment. Nat Rev Cardiol. 2017;14(2):113–24. https://doi.org/10.1038/nrcardio.2016.171.
Magnussen C, Niiranen TJ, Ojeda F, Gianfagna F, Blankenberg S, Njølstad I et al. Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts: results from the BiomarCaRE Consortium (Biomarker for Cardiovascular Risk Assessment in Europe). Circulation. 2017:CIRCULATIONAHA. 117.028981.
Ko D, Rahman F, Schnabel RB, Yin X, Benjamin EJ, Christophersen IE. Atrial fibrillation in women: epidemiology, pathophysiology, presentation, and prognosis. Nat Rev Cardiol. 2016;13(6):321–32. https://doi.org/10.1038/nrcardio.2016.45.
Emdin CA, Wong CX, Hsiao AJ, Altman DG, Peters SA, Woodward M, et al. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ. 2016;532:h7013. https://doi.org/10.1136/bmj.h7013.
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation. 2014;129(8):837–47. https://doi.org/10.1161/CIRCULATIONAHA.113.005119.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of atrial fibrillation. JAMA. 2001;285(22):2864–70.
Chen J-Y, Zhang A-D, Lu H-Y, Guo J, Wang F-F, Li Z-C. CHADS2 versus CHA2DS2-VASc score in assessing the stroke and thromboembolism risk stratification in patients with atrial fibrillation: a systematic review and meta-analysis. J Geriatr Cardiol. 2013;10(3):258–66.
Fauchier L, Clementy N, Pelade C, Collignon C, Nicolle E, Lip GYH. Patients with ischemic stroke and incident atrial fibrillation. Stroke. 2015;46(9):2432–7. https://doi.org/10.1161/strokeaha.115.010270.
Bisson A, Bodin A, Clementy N, Babuty D, Lip GYH, Fauchier L. Prediction of incident atrial fibrillation according to gender in patients with ischemic stroke from a Nationwide cohort. Am J Cardiol. 2018;121(4):437–44. https://doi.org/10.1016/j.amjcard.2017.11.016.
Liu R, Yang X, Li S, Jiang Y, Wang Y, Wang Y. Modified CHADS2 and CHA2DS2-VASc scores to predict atrial fibrillation in acute ischemic stroke patients. Journal of Clinical Neuroscience: J Clin Neurosci. 2018;51:35–8. https://doi.org/10.1016/j.jocn.2018.02.016.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation--developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385–413. https://doi.org/10.1093/europace/eus305.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–76. https://doi.org/10.1016/j.jacc.2014.03.022.
Mason PK, Lake DE, DiMarco JP, Ferguson JD, Mangrum JM, Bilchick K, et al. Impact of the CHA2DS2-VASc score on anticoagulation recommendations for atrial fibrillation. Am J Med. 2012;125(6):603. e1-. e6.
Friberg L, Benson L, Rosenqvist M, Lip GY. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ. 2012;344:e3522.
Yao X, Gersh BJ, Sangaralingham LR, Kent DM, Shah ND, Abraham NS, et al. Comparison of the CHA2DS2-VASc, CHADS2, HAS-BLED, ORBIT, and ATRIA risk scores in predicting non–vitamin K antagonist oral anticoagulants-associated bleeding in patients with atrial fibrillation. Am J Cardiol. 2017;120(9):1549–56.
Nezu T, Hosomi N, Kondo K, Aoki S, Matsumoto M, Kobayashi S. Greater severity of neurological defects in women admitted with atrial fibrillation-related stroke. Circ J. 2016;80(1):250–5. https://doi.org/10.1253/circj.CJ-15-0873.
Martin RC, Burgin WS, Schabath MB, Kirby B, Chae SH, Fradley MG, et al. Gender-specific differences for risk of disability and death in atrial fibrillation-related stroke. Am J Cardiol. 2017;119(2):256–61.
Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am. 2008;92(1):17–40, ix. https://doi.org/10.1016/j.mcna.2007.09.002.
Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation. The Framingham study. Stroke. 1996;27(10):1760–4.
Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med. 2003;349(11):1019–26. https://doi.org/10.1056/NEJMoa022913.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham study. Stroke. 1991;22(8):983–8.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50(5):e1–e88. https://doi.org/10.1093/ejcts/ezw313.
Lip GY, Rushton-Smith SK, Goldhaber SZ, Fitzmaurice DA, Mantovani LG, Goto S, et al. Does sex affect anticoagulant use for stroke prevention in nonvalvular atrial fibrillation? The prospective global anticoagulant registry in the FIELD-atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2015;8(2 Suppl 1):S12–20. https://doi.org/10.1161/circoutcomes.114.001556.
•• Thompson LE, Maddox TM, Lei L, Grunwald GK, Bradley SM, Peterson PN et al. Sex Differences in the Use of Oral Anticoagulants for Atrial Fibrillation: A Report From the National Cardiovascular Data Registry (NCDR(R)) PINNACLE Registry. J Am Heart Assoc. 2017;6(7). https://doi.org/10.1161/jaha.117.005801. This study highlights the underutilization of oral anticoagulants for thromboembolic prophylaxis in women and showed that women with AF are significantly less likely to receive OACs at all levels of CHA2DS2VASc levels.
• Noseworthy P, Yao X, Sangaralingham L, Shah N. 5716Age and gender differences in stroke and bleeding risks in atrial fibrillation patients treated with non-vitamin K antagonist oral anticoagulants. Eur Heart J 2017;38(suppl_1). This study compared the direct oral anticoagulants and showed that dabigatran was associated with a lower risk of thromboembolism compared with apixaban and rivaroxaban in women 75 years of age and above.
•• Loikas D, Forslund T, Wettermark B, Schenck-Gustafsson K, Hjemdahl P, von Euler M. Sex and gender differences in Thromboprophylactic treatment of patients with atrial fibrillation after the introduction of non–vitamin K oral anticoagulants. Am J Cardiol 2017;120(8):1302–1308. This study investigated the sex differences in use of thromboprophylaxis in patients with AF before and after the introduction of direct oral anticoagulants and showed that the the sex differences in 2011 were no longer observed in 2015, with the exception of women ≥ 80 years and patients with complicated co-morbidities.
Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347(23):1825–33. https://doi.org/10.1056/NEJMoa021328.
Sullivan RM, Zhang J, Zamba G, Lip GY, Olshansky B. Relation of gender-specific risk of ischemic stroke in patients with atrial fibrillation to differences in warfarin anticoagulation control (from AFFIRM). Am J Cardiol. 2012;110(12):1799–802. https://doi.org/10.1016/j.amjcard.2012.08.014.
Pancholy SB, Sharma PS, Pancholy DS, Patel TM, Callans DJ, Marchlinski FE. Meta-analysis of gender differences in residual stroke risk and major bleeding in patients with nonvalvular atrial fibrillation treated with oral anticoagulants. Am J Cardiol. 2014;113(3):485–90. https://doi.org/10.1016/j.amjcard.2013.10.035.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Connolly SJ, Eikelboom J, Joyner C, Diener HC, Hart R, Golitsyn S, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364(9):806–17. https://doi.org/10.1056/NEJMoa1007432.
Proietti M, Cheli P, Basili S, Mazurek M, Lip GY. Balancing thromboembolic and bleeding risk with non-vitamin K antagonist oral anticoagulants (NOACs): a systematic review and meta-analysis on gender differences. Pharmacol Res. 2017;117:274–82.
Moseley A, Doukky R, Williams KA, Jaffer AK, Volgman AS. Indirect comparison of novel oral anticoagulants in women with Nonvalvular atrial fibrillation. J Women's Health. 2017;26(3):214–21. https://doi.org/10.1089/jwh.2016.5892.
Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61(2):755–9. https://doi.org/10.1016/0003-4975(95)00887-X.
Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999;82(5):547–54.
Di Biase L, Santangeli P, Anselmino M, Mohanty P, Salvetti I, Gili S, et al. Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation?: results from a multicenter study. J Am Coll Cardiol. 2012;60(6):531–8.
Casu G, Gulizia MM, Molon G, Mazzone P, Audo A, Casolo G, et al. ANMCO/AIAC/SICI-GISE/SIC/SICCH consensus document: percutaneous occlusion of the left atrial appendage in non-valvular atrial fibrillation patients: indications, patient selection, staff skills, organisation, and training. Eur Heart J Suppl. 2017;19(suppl_D):D333–D53.
O'brien EC, Holmes DN, Ansell JE, Allen LA, Hylek E, Kowey PR, et al. Physician practices regarding contraindications to oral anticoagulation in atrial fibrillation: findings from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF) registry. Am Heart J. 2014;167(4):601–609.e1.
Madden JL. Resection of the left auricular appendix: a prophylaxis for recurrent arterial emboli. J Am Med Assoc. 1948;140(9):769–72.
Healey JS, Crystal E, Lamy A, Teoh K, Semelhago L, Hohnloser SH, et al. Left atrial appendage occlusion study (LAAOS): results of a randomized controlled pilot study of left atrial appendage occlusion during coronary bypass surgery in patients at risk for stroke. Am Heart J. 2005;150(2):288–93. https://doi.org/10.1016/j.ahj.2004.09.054.
Whitlock RP, Vincent J, Blackall MH, Hirsh J, Fremes S, Novick R, et al. Left atrial appendage occlusion study II (LAAOS II). Can J Cardiol. 2013;29(11):1443–7.
Whitlock R, Healey J, Vincent J, Brady K, Teoh K, Royse A, et al. Rationale and design of the left atrial appendage occlusion study (LAAOS) III. Ann Cardiothorac Surg. 2014;3(1):45–54.
Inoue T, Suematsu Y. Left atrial appendage resection can be performed minimally invasively with good clinical and echocardiographic outcomes without any severe risk. Eur J Cardiothorac Surg. 2018;54:78–83.
Fountain RB, Holmes DR, Chandrasekaran K, Packer D, Asirvatham S, Van Tassel R, et al. The PROTECT AF (WATCHMAN left atrial appendage system for embolic PROTECTion in patients with atrial fibrillation) trial. Am Heart J. 2006;151(5):956–61.
Holmes DR Jr, Doshi SK, Kar S, Price MJ, Sanchez JM, Sievert H, et al. Left atrial appendage closure as an alternative to warfarin for stroke prevention in atrial fibrillation: a patient-level meta-analysis. J Am Coll Cardiol. 2015;65(24):2614–23.
Reddy VY, Doshi SK, Kar S, Gibson DN, Price MJ, Huber K, et al. 5-year outcomes after left atrial appendage closure: from the PREVAIL and PROTECT AF trials. J Am Coll Cardiol. 2017;70(24):2964–75.
Kaneko H, Neuss M, Weissenborn J, Butter C. Predictors of thrombus formation after percutaneous left atrial appendage closure using the WATCHMAN device. Heart Vessel. 2017;32(9):1137–43.
Saw J, Tzikas A, Shakir S, Gafoor S, Omran H, Nielsen-Kudsk JE, et al. Incidence and clinical impact of device-associated thrombus and peri-device leak following left atrial appendage closure with the Amplatzer cardiac plug. J Am Coll Cardiol Intv. 2017;10(4):391–9.
Cochet H. Left atrial appendage patency and device-related thrombus after percutaneous left atrial appendage occlusion: a computed tomography study. Eur Heart J Cardiovasc Imaging. 2018;0:1–11. https://doi.org/10.1093/ehjci/jey010.
Price MJ, Reddy VY, Valderrabano M, Halperin JL, Gibson DN, Gordon N, et al. Bleeding outcomes after left atrial appendage closure compared with long-term warfarin. A pooled, patient-level analysis of the WATCHMAN randomized trial experience. JACC Cardiovasc Interv. 2015;8(15):1925–32. https://doi.org/10.1016/j.jcin.2015.08.035.
Kreidieh B, Rojas F, Schurmann P, Dave AS, Kashani A, Rodríguez-Mañero M, et al. Left atrial appendage remodeling after Lariat left atrial appendage ligation. Circ Arrhythm Electrophysiol. 2015;8(6):1351–8.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. ESC Scientific Document Group. ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–2962. https://doi.org/10.1093/eurheartj/ehw210.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. J Interv Card Electrophysiol. 2017;50(1):1–55. https://doi.org/10.1007/s10840-017-0277-z.
Chatterjee S, Sardar P, Lichstein E, Mukherjee D, Aikat S. Pharmacologic rate versus rhythm-control strategies in atrial fibrillation: an updated comprehensive review and meta-analysis. Pacing Clin Electrophysiol. 2013;36(1):122–33. https://doi.org/10.1111/j.1540-8159.2012.03513.x.
Ionescu-Ittu R, Abrahamowicz M, Jackevicius CA, Essebag V, Eisenberg MJ, Wynant W, et al. Comparative effectiveness of rhythm control vs rate control drug treatment effect on mortality in patients with atrial fibrillation. Arch Intern Med. 2012;172(13):997–1004. https://doi.org/10.1001/archinternmed.2012.2266.
Sethi NJ, Feinberg J, Nielsen EE, Safi S, Gluud C, Jakobsen JC. The effects of rhythm control strategies versus rate control strategies for atrial fibrillation and atrial flutter: a systematic review with meta-analysis and Trial sequential analysis. PLoS One. 2017;12(10):e0186856. https://doi.org/10.1371/journal.pone.0186856.
Ciszewski J, Maciag A, Kowalik I, Syska P, Lewandowski M, Farkowski MM, et al. Comparison of the rhythm control treatment strategy versus the rate control strategy in patients with permanent or long-standing persistent atrial fibrillation and heart failure treated with cardiac resynchronization therapy - a pilot study of cardiac resynchronization in atrial fibrillation trial (pilot-CRAfT): study protocol for a randomized controlled trial. Trials. 2014;15:386. https://doi.org/10.1186/1745-6215-15-386.
Kirchhof P, Breithardt G, Camm AJ, Crijns HJ, Kuck KH, Vardas P, et al. Improving outcomes in patients with atrial fibrillation: rationale and design of the Early treatment of atrial fibrillation for stroke prevention trial. Am Heart J. 2013;166(3):442–8. https://doi.org/10.1016/j.ahj.2013.05.015.
Wassertheil-Smoller S, McGinn AP, Martin L, Rodriguez BL, Stefanick ML, Perez M. The associations of atrial fibrillation with the risks of incident invasive breast and colorectal Cancer. Am J Epidemiol. 2017;185(5):372–84. https://doi.org/10.1093/aje/kww185.
Osman MH, Farrag E, Selim M, Osman MS, Hasanine A, Selim A. Cardiac glycosides use and the risk and mortality of cancer; systematic review and meta-analysis of observational studies. PLoS One. 2017;12(6):e0178611. https://doi.org/10.1371/journal.pone.0178611.
Shoemaker MB, Muhammad R, Farrell M, Parvez B, White BW, Streur M, et al. Relation of morbid obesity and female gender to risk of procedural complications in patients undergoing atrial fibrillation ablation. Am J Cardiol. 2013;111(3):368–73. https://doi.org/10.1016/j.amjcard.2012.10.013.
Arbelo E, Brugada J, Blomstrom-Lundqvist C, Laroche C, Kautzner J, Pokushalov E, et al. Contemporary management of patients undergoing atrial fibrillation ablation: in-hospital and 1-year follow-up findings from the ESC-EHRA atrial fibrillation ablation long-term registry. Eur Heart J. 2017;38(17):1303–16. https://doi.org/10.1093/eurheartj/ehw564.
Shakkottai P, Sy RW, McGuire MA. Cryoablation for atrial fibrillation in 2017: what have we learned? Heart Lung Circ. 2017;26(9):950–9. https://doi.org/10.1016/j.hlc.2017.05.115.
Ikenaga H, Nakano Y, Oda N, Suenari K, Sairaku A, Tokuyama T, et al. Radiofrequency catheter ablation is effective for atrial fibrillation patients with hypertrophic cardiomyopathy by decreasing left atrial pressure. J Arrhythm. 2017;33(4):256–61. https://doi.org/10.1016/j.joa.2016.08.006.
Yu HT, Shim J, Park J, Kim IS, Kim TH, Uhm JS, et al. Pulmonary vein isolation alone versus additional linear ablation in patients with persistent atrial fibrillation converted to paroxysmal type with antiarrhythmic drug therapy: a multicenter, prospective, randomized study. Circ Arrhythm Electrophysiol. 2017;10(6):e004915. https://doi.org/10.1161/circep.116.004915.
Zembala M, Filipiak K, Kowalski O, Buchta P, Niklewski T, Nadziakiewicz P, et al. Staged hybrid ablation for persistent and longstanding persistent atrial fibrillation effectively restores sinus rhythm in long-term observation. Arch Med Sci. 2017;13(1):109–17. https://doi.org/10.5114/aoms.2015.53960.
Kalla M, Sanders P, Kalman JM, Lee G. Radiofrequency catheter ablation for atrial fibrillation: approaches and outcomes. Heart Lung Circ. 2017;26(9):941–9. https://doi.org/10.1016/j.hlc.2017.05.125.
Zylla MM, Brachmann J, Lewalter T, Hoffmann E, Kuck KH, Andresen D, et al. Sex-related outcome of atrial fibrillation ablation: insights from the German ablation registry. Heart Rhythm. 2016;13(9):1837–44. https://doi.org/10.1016/j.hrthm.2016.06.005.
Kautzner J, Peichl P, Sramko M, Cihak R, Aldhoon B, Wichterle D. Catheter ablation of atrial fibrillation in elderly population. J Geriatr Cardiol. 2017;14(9):563–8. https://doi.org/10.11909/j.issn.1671-5411.2017.09.008.
Duytschaever M, Demolder A, Phlips T, Sarkozy A, El Haddad M, Taghji P, et al. PulmOnary vein isolation with vs. without continued antiarrhythmic drug trEatment in subjects with recurrent atrial fibrillation (POWDER AF): results from a multicentre randomized trial. Eur Heart J. 2017;39:1429–37. https://doi.org/10.1093/eurheartj/ehx666.
Yagishita A, Yamauchi Y, Sato H, Yamashita S, Hirao T, Miyamoto T, et al. Efficacy of catheter ablation and concomitant antiarrhythmic drugs on the reduction of the arrhythmia burden in patients with long-standing persistent atrial fibrillation. J Atr Fibrillation. 2017;10(3):1649. https://doi.org/10.4022/jafib.1649.
Huffman MD, Karmali KN, Berendsen MA, Andrei AC, Kruse J, McCarthy PM et al. Concomitant atrial fibrillation surgery for people undergoing cardiac surgery. Cochrane Database Syst Rev. 2016;(8):CD011814. https://doi.org/10.1002/14651858.CD011814.pub2.
Badhwar V, Rankin JS, Damiano RJ Jr, Gillinov AM, Bakaeen FG, Edgerton JR, et al. The Society of Thoracic Surgeons 2017 clinical practice guidelines for the surgical treatment of atrial fibrillation. Ann Thorac Surg. 2017;103(1):329–41. https://doi.org/10.1016/j.athoracsur.2016.10.076.
Oza NM, Baveja S, Tedrow U. Bridging the gender gap in atrial fibrillation. Expert Rev Cardiovasc Ther. 2015;13(3):317–23. https://doi.org/10.1586/14779072.2015.1002466.
Cove CL, Albert CM, Andreotti F, Badimon L, Van Gelder IC, Hylek EM. Female sex as an independent risk factor for stroke in atrial fibrillation: possible mechanisms. Thromb Haemost. 2014;111(3):385–91. https://doi.org/10.1160/TH13-04-0347.
Ambrosi CM, Yamada KA, Nerbonne JM, Efimov IR. Gender differences in electrophysiological gene expression in failing and non-failing human hearts. PLoS One. 2013;8(1):e54635. https://doi.org/10.1371/journal.pone.0054635.
Kwok CS, Loke YK, Hale R, Potter JF, Myint PK. Atrial fibrillation and incidence of dementia: a systematic review and meta-analysis. Neurology. 2011;76(10):914–22. https://doi.org/10.1212/WNL.0b013e31820f2e38.
Santangeli P, Di Biase L, Bai R, Mohanty S, Pump A, Brantes MC, et al. Atrial fibrillation and the risk of incident dementia: a meta-analysis. Heart Rhythm. 2012;9(11):1761–1768.e2.
Mead GE, Keir S. Association between cognitive impairment and atrial fibrillation: a systematic review. J Stroke Cerebrovasc Dis. 2001;10(2):35–43. https://doi.org/10.1053/jscd.2001.24663.
Ott A, Breteler MM, de Bruyne MC, van Harskamp F, Grobbee DE, Hofman A. Atrial fibrillation and dementia in a population-based study. The Rotterdam study. Stroke. 1997;28(2):316–21.
Elias MF, Sullivan LM, Elias PK, Vasan RS, D'Agostino RB Sr, Seshadri S, et al. Atrial fibrillation is associated with lower cognitive performance in the Framingham offspring men. J Stroke Cerebrovasc Dis. 2006;15(5):214–22. https://doi.org/10.1016/j.jstrokecerebrovasdis.2006.05.009.
Forti P, Maioli F, Pisacane N, Rietti E, Montesi F, Ravaglia G. Atrial fibrillation and risk of dementia in non-demented elderly subjects with and without mild cognitive impairment. Neurol Res. 2006;28(6):625–9. https://doi.org/10.1179/016164106x130461.
Di Carlo A, Baldereschi M, Amaducci L, Maggi S, Grigoletto F, Scarlato G, et al. Cognitive impairment without dementia in older people: prevalence, vascular risk factors, impact on disability. The Italian longitudinal study on aging. J Am Geriatr Soc. 2000;48(7):775–82.
Gargano JW, Paul Coverdell RM. National Acute Stroke Registry Michigan Prototype I. Sex differences in stroke recovery and stroke-specific quality of life: results from a statewide stroke registry. Stroke. 2007;38(9):2541–8.
Nishtala A, Piers RJ, Himali JJ, Beiser AS, Davis-Plourde KL, Saczynski JS, et al. Atrial fibrillation and cognitive decline in the Framingham heart study. Heart Rhythm. 2018;15(2):166–72. https://doi.org/10.1016/j.hrthm.2017.09.036.
Stefansdottir H, Arnar DO, Aspelund T, Sigurdsson S, Jonsdottir MK, Hjaltason H, et al. Atrial fibrillation is associated with reduced brain volume and cognitive function independent of cerebral infarcts. Stroke. 2013;44(4):1020–5. https://doi.org/10.1161/STROKEAHA.12.679381.
Ball J, Carrington MJ, Stewart S, investigators S. Mild cognitive impairment in high-risk patients with chronic atrial fibrillation: a forgotten component of clinical management? Heart. 2013;99(8):542–7. https://doi.org/10.1136/heartjnl-2012-303182.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Charlotte Bai, Nidhi Madan, Shaza Alshahrani, and Annabelle Santos Volgman each declare no potential conflicts of interest.
Neelum T. Aggarwal declares the following: Merck and Company-Adjudication Committee member (Consultant); Eli Lilly: Clinical Trial of Solanezumab for Older Individuals Who May be at Risk for Memory Loss (A4 Study-Site Principal Investigator-Rush) ClinicalTrials.gov Identifier: NCT02008357; Novartis/AMGEN: A Study of CAD106 and CNP520 Versus Placebo in Participants at Risk for the Onset of Clinical Symptoms of Alzheimer’s Disease (Generation S1)-Site Principal Investigator-Rush: ClinicalTrials.gov Identifier: NCT02565511; Novartis/AMGEN: A Study of CNP520 Versus Placebo in Participants at Risk for the Onset of Clinical Symptoms of Alzheimer’s Disease (Generation S2)- Site Principal Investigator- Rush ClinicalTrials.gov Identifier: NCT03131453; and Janssen: An Efficacy and Safety Study of JNJ-54861911 in Participants Who Are Asymptomatic at Risk for Developing Alzheimer’s Dementia (EARLY)-Site Principal Investigator-Rush ClinicalTrials.gov Identifier: NCT02569398.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Women’s Health
Rights and permissions
About this article
Cite this article
Bai, C.J., Madan, N., Alshahrani, S. et al. Sex Differences in Atrial Fibrillation—Update on Risk Assessment, Treatment, and Long-Term Risk. Curr Treat Options Cardio Med 20, 79 (2018). https://doi.org/10.1007/s11936-018-0682-3
Published:
DOI: https://doi.org/10.1007/s11936-018-0682-3