Abstract
Purpose of Review
While ureteroscopy (URS) is a common procedure for ureteric stones, this window between diagnosis and treatment leaves the possibility for a ‘negative’, ‘stoneless’ or ‘diagnostic’ URS. We perform a systematic review to look at the rate of ‘negative ureteroscopy’ and risk factors associated with it.
Recent Findings
From a total of 3599 articles and 68 abstracts, 4 studies (1336 patients) were selected. The negative URS rate varied from 4 to 14%. Common predictors seem to be female gender, small stones, radiolucent stones and distal ureteric stones.
Summary
Although infrequent, negative ureteroscopy should be avoided in patients with ureteric stones by performing a low-dose CT scan on the day of surgery. This should especially be performed for females and those with smaller, radiolucent or distal ureteric stones.
Similar content being viewed by others
Introduction
The global incidence of stone disease ranges from 1 to 15% with a lifetime prevalence of up to 14% in the UK [1••]. This has been contributed by a rise in the incidence of obesity, metabolic syndrome and warm weather [2, 3•, 4,5,6,7]. The surgical management especially ureteroscopy (URS) has seen a huge rise over the last two decades (252%) with its share of total endourological treatment of stone disease increasing by 17% [8••]. Although URS is regarded as a procedure with low risk of major complications, Clavien III–V complications do occur and range from ureteric perforation or avulsion, urosepsis, haematoma, pulmonary or cardiac complications and rarely death [9•].
Up to 68% of ureteric stones are likely to pass spontaneously without any surgical intervention depending on their size or location in the ureter [10]. This information is easier to corroborate when patient reports having passed their stone; however, this does not always happen. Stone passage or not is also clouded by on-going symptoms, time delay for their surgery, radiopacity of the stone and previous imaging modality used. Where ambiguity exists, patients who have not passed their stone spontaneously could therefore be offered an up-to-date imaging. This should be done as close to their planned URS procedure to ensure that they do not undergo an unnecessary URS procedure as in some cases the stone might already have passed.
While non-contrast CT scan (NCCT) is the gold standard for the initial diagnosis of ureteric or kidney stones, there is no recommendation for the type of imaging modality to confirm stone passage [11–12]. Ultrasound has a sensitivity of 19–93% and a specificity of 84–100% but can be user dependent [12], while plain KUB X-ray has a sensitivity of 44–77% and a specificity of 80–87% but varies on whether the stone is radiopaque or not.
Although treatment of ureteric stones should be carried out if the stone has not spontaneously passed, there is currently no stipulated time interval for this to be done [11]. It is however preferable to avoid delays if stone treatment is deemed necessary. This window between diagnosis and treatment leaves the possibility for a ‘negative’, ‘stoneless’ or ‘diagnostic’ URS, where a stone is absent from the urinary tract due to spontaneous unnoticed passage of stone while the patients wait for this procedure to happen. Considering the risks involved with ureteroscopy for stone disease [13, 14], we look at the rate of ‘negative ureteroscopy’ with risk factors associated with it and discuss strategies to reduce it in clinical practice.
Materials and Methods
Evidence Acquisition
Inclusion criteria
-
1.
Patients undergoing ureteroscopy for stone disease and reporting on ‘negative’ ureteroscopy
-
2.
English language articles
-
3.
Patients of all age groups
Exclusion criteria
-
1.
Ureteroscopy done for non-stone cases
-
2.
Animal or laboratory studies
-
3.
Case reports or review articles
Search Strategy and Study Selection
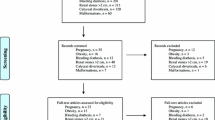
The systematic review was performed according to the Cochrane review guidelines and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) checklist [15, 16] from January 1990 to October 2018 for English language articles. The search strategy was conducted to find relevant studies from the Medline, EMBASE, Scopus, Cochrane Library, CINAHL, Clinicaltrials.gov, Google Scholar and individual urologic journals. The search terms included ‘Ureteroscopy’, ‘URS’, ‘Retrograde intrarenal surgery’, ‘RIRS’, ‘ureteric’, ‘ureter’, ‘stoneless’, ‘stone’, ‘calculi’, ‘Negative’ and ‘Diagnostic’. Boolean operators (AND, OR) were used to refine the search. Two experienced reviewers (PR and BS) identified all studies. All studies that appeared to fit the inclusion criteria were included for full review. Each reviewer independently selected studies for inclusion in the review and discrepancies were resolved by mutual consensus.
Data Extraction and Analysis
The following variables were extracted from each study: journal published, year of publication, total number of URS performed, rate and predictors of diagnostic URS and strategies to prevent it. Data was collated using Microsoft Excel (version 12.2.4).
Results
A total of 3599 articles were initially identified and after removal of duplicates, 1637 were screened of which 68 abstracts were further evaluated (Fig. 1). Eight full-text articles were obtained and finally 4 studies (1336 patients) were selected for our review [17,18,19,20]. These studies were published from 2011 to 2018, covering URS procedures carried out between 2003 and 2015.
Negative URS Rate and Predictive Factors
The negative URS rate varied from 3.9 to 13.7% (Table 1) [17,18,19,20]. Three studies investigated potential predictive factors for a negative URS (Table 2) [17, 18, 20]. None of the studies found age to be a significant factor for negative URS. Female gender was a significant predictor in two studies [17, 18]. Katafigiotis et al. found that female sex significantly predicted negative URS (OR 6.80; CI 1.56, 29.70; p = 0.011) [17]. Lamberts et al. also found that female sex significantly predicted negative URS (OR 1.41; CI 1.25, 1.58; p < 0.05) [18]. Kreshover et al., however, did not find sex to be a significant predictive factor for negative URS [20]. Katafigiotis and colleagues also found that non-radiopaque stones significantly predicted negative URS (OR 11.11; CI 2.51, 49.20; p = 0.002) [17]. They used a multivariate model which combined stone length, surface area, volume, and width on CT scan and found that smaller size significantly predicted negative URS (AUC 0.95; CI 0.92–0.97; p < 0.0001). Similarly, Kreshover et al. found that stone size (p < 0.00) and location (p = 0.04) significantly predicted negative URS with higher rate of negative URS for small stones and stones located in the distal ureter [20].
Katafigiotis and colleagues found no association for negative URS with anatomical site (divided by thirds of the ureter), body mass index (BMI), stone number or side and seasonal variation [17]. Similarly, Kreshover et al. showed that the presence of preoperative pain, hydronephrosis, time interval since the initial CT scan and the use of medical expulsive therapy (MET) were not predictors of negative URS [20]. In the third study, Lamberts and team found that insurance type significantly predicted negative URS; however, race/ethnicity and the year of surgery did not predict negative URS [18].
Imaging Strategy Used in Studies
The imaging strategy is reported in Table 2. Only two studies described their imaging strategy for the investigation of potential urinary calculi [17, 20]. Katafigiotis et al. performed a plain KUB XR on all patients a day before receiving an endourologic procedure and if any doubt existed after initial imaging, a CT KUB was performed. In the event of a negative URS, both nephroscopy and a whole collecting system revision were completed with a flexible scope. Kreshover et al. described their indication for URS, but not their strategy following a negative URS [20]. Their indication for URS included the persistence of stone and/or pain in patients diagnosed with a ureteral stone, or pain/infection in patients with a renal stone or a contralateral stone with the aforementioned indication and an ipsilateral stone.
Discussion
Outcomes of Our Review
This is the first paper to systematically review the literature and collate the evidence on ‘stoneless’ or ‘negative’ URS reporting on a rate of between 4 and 14%. While it might be almost impossible to have no cases of negative URS, clearly all efforts should be made for this to be minimised. Some of the common predictors seem to be small stones, radiolucent stones, distal ureteric stones and female gender.
Meaning of the Study
With an overall complication rate reported from clinical research office of endourological society (CROES) at 7.4%9, urologists need to realise that URS for stone disease should only be offered when necessary and the rate of negative diagnostic URS for stone disease should be minimal. CROES study included an intra-operative complication rate of 4.2%, which is a potentially damaging risk and should be avoided. With an increase in medicolegal allegations, perhaps there needs to be a balance between the radiation risk with repeat imaging, diagnostic accuracy of the imaging, cancellation of URS procedure when the ureteric stone is still present and complications from negative unnecessary URS. This poses a unique challenge where the imaging modality needs to be accurate; the radiation dose follows the ‘as low as reasonably achievable’ (ALARA) principle and the imaging is carried out close to the date of surgery, preferably on the same day. Similarly, while the objective is to minimise negative URS, patients need to go ahead with their URS procedure if the stone in question is still not passed. For this reason, while plain KUB XR can be useful for radiopaque stone, it might not be helpful in all patients specially when the stone is radiolucent. An USS is user dependent and may not be helpful for ureteric stones either. The only way to confirm the diagnosis would be a NCCT and while CT urogram (CTU) might be more diagnostic, it is probably unnecessary in all patients and would increase the radiation dose considerably.
Female gender was associated with a higher rate of negative URS. Females have an increased prevalence of pelvic phleboliths on imaging which may be mistaken for urinary stones [21,22,23]. Furthermore, females have a higher prevalence of medullary sponge kidney, which may result in parenchymal calcifications being mistaken for urinary stones [24]. There may also be an increased change of unnoticed spontaneous passage in females due to the shorter urethra and lower voiding pressure ultimately reducing the level of dysuria [25].
An Ideal Approach to Reduce Negative Ureteroscopy
During the initial presentation, all patients should have a NCCT along with a plain KUBXR unless the stone is clearly visible on the scout image of the NCCT [26]. This might help with the follow-up for radiopaque stones. While USS is not always reliable for follow-up, a CTU carries a large radiation dose and therefore a NCCT seems to be the sensible approach.
Those patients who spontaneously pass their stone with complete resolution of their symptoms, efforts must be made to send the stone for biochemical analysis. Where the patients have not noted passing their ureteric stone, the solution would therefore be to get a NCCT prior to URS which could be either on the day of surgery or as close to the date of surgery as possible. This would especially be useful for radiolucent stone or small stones or stones in the ureter which is not clearly seen on plain KUBXR. This might however not be necessary in all cases especially where the stone is clearly visible on the plain KUBXR during their initial presentation, where a repeat KUBXR imaging to compare the initial image can help with confirming the stone presence.
Where symptoms suggestive of ureteric stones are still there but the imaging is inconclusive, a careful informed counselling and decision-making need to happen with the patient going through the pros and cons of doing the URS. The risk of major complications albeit small must be discussed [9, 13, 14].
Strengths and Limitations of the Study
Although there is very little published data on negative URS, this is common in clinical practice and no current guidance exists on this subject. Our review provides the predictors for negative URS and some management strategies to minimise it. The limitation of our systematic review is the publication bias that may exist in the literature with authors shying away from publishing their results on negative URS. Perhaps, it is time that we collectively share this guilt to try and reduce unnecessary URS procedures, the complications of which will lead to patient suffering in most cases. Although the rates of negative URS are mentioned, the studies included do not mention the complications from the anaesthesia or the procedure itself.
Areas of Future Research
The conclusions of our study are a reflection of the included studies but as the role of URS is broadened for paediatric and pregnant patients with increasing stone complexity [27,28,29], the effect of these complications may be more pronounced in these high-risk patients. With a reducing cost and rising number of URS procedures now being done for stone disease [8••, 30, 31], the temptation to perform this as a diagnostic procedure should be curbed. The cost of repeat imaging and potential cancellation of the URS procedure must be balanced with that of the cost of URS and any complications should it arise.
While the plain XRKUB is cheap and readily available, it is not as reliable as a NCCT. Although most NCCT now follows a low-dose and an ultra-low-dose protocol, perhaps an ideal way of reducing the follow-up radiation further would be to obtain targeted imaging of the concerned area. Its role and accuracy in patients with stent in situ will also need to be clarified. Perhaps it is time for a truly multicentric prospective study to determine the practicality and real cost of reducing the rates of diagnostic ureteroscopy.
Conclusion
Although infrequent, negative ureteroscopy should be avoided in patients with ureteric stones. No current guidelines are available and perhaps performing a non-contrast low-dose CT scan on the day of surgery will help to reduce it while maintaining a low radiation dose. This should especially be performed for females and those with smaller, radiolucent or distal ureteric stones.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Rukin N, Siddiqui Z, Chedgy E, et al. Trends in upper tract stone disease in England: evidence from the Hospital Episodes Statistics (HES) database. Urol Int. 2017;98(4):391–6 This paper looks at the UK hospital data and puts the prevelance of kidney stones at 14%.
Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010;12(2–3):e86.
• Geraghty R, Proietti S, Traxer O, et al. Worldwide impact of warmer seasons on the incidence of renal colic and kidney stone disease (KSD): evidence from a systematic review of literature. J Endourol. 2017;31(8):729–35 This systematic review shows a clear association of warm weather with renal colic and kidney stone disease.
Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. Jama. 2005;293(4):455–62.
Taylor E, Curhan G. Diet and fluid prescription in stone disease. Kidney Int. 2006;70(5):835–9.
Wong YV, Cook P, Somani BK. The association of metabolic syndrome and urolithiasis. Int J Endocrinol. 2015;2015:1–9.
Wong Y, Cook P, Roderick P, Somani BK. Metabolic syndrome and kidney stone disease: a systematic review of literature. J Endourol. 2016;30(3):246–53.
•• Geraghty R, Jones P, Somani BK. Worldwide trends of urinary stone disease treatment over the last two decades: a systematic review. J Endourol. 2017;31(6):547–56 This paper shows a convincing worldwide evidence of increasing use of URS for treatment of stone disease.
• Somani BK, Giusti G, Sun Y, et al. Complications associated with ureteroscopy (URS) related to treatment of urolithiasis: The Clinical Office of Endourological Society URS Global Study. World J Urol. 2017;35(4):675–81 This paper looks at the complications of URS from CROES worldwide database. The data shows that although URS is common, there are several minor and major complications associated with it.
Yallappa S, Amer T, Jones P, Greco F, Tailly T, Somani BK, et al. Natural history of conservatively managed ureteric stones from a cumulative analysis of 6600 patients. J Endourol. 2018;32(5):371–9.
Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on diagnosis and conservative management of urolithiasis. Eur Urol. 2016;69(3):468–74.
Ray AA, Ghiculete D, Pace KT, Honey RJD'A. Limitations to ultrasound in the detection and measurement of urinary tract calculi. Urology. 2010;76(2):295–300.
Whitehurst LA, Somani BK. Perirenal haematoma after ureteroscopy: a systematic review. J Endourol. 2017;31(5):438–45.
Whitehurst L, Jones P, Somani BK. Global mortality of kidney stone disease over the last two decades a systematic review of literature. World J Urol. 2018. https://doi.org/10.1007/s00345-018-2424-2 Review.
Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. Chichester: Wiley; 2008.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Katafigiotis I, Sabler IM, Heifetz EM, Rosenfeld A, Stavros S, Lorber A, et al. “Stoneless” or negative ureteroscopy: a reality in the endourologic routine or avoidable source of frustration? Estimating the risk factors for a negative ureteroscopy. J Endourol. 2018;32(9):825–30.
Lamberts RW, Conti SL, Leppert JT, Elliott CS. Defining the rate of negative ureteroscopy in the general population treated for upper tract urinary stone disease. J Endourol. 2017;31(3):266–71.
White WM, Johnson EB, Zite NB, Beddies J, Krambeck AE, Hyams E, et al. Predictive value of current imaging modalities for the detection of urolithiasis during pregnancy: a multicenter, longitudinal study. J Urol. 2013;189(3):931–4.
Kreshover JE, Dickstein RJ, Rowe C, Babayan RK, Wang DS. Predictors for negative ureteroscopy in the management of upper urinary tract stone disease. Urology. 2011;78(4):748–52.
Smith RC, Rosenfield AT, Choe KA, Essenmacher KR, Verga M, Glickman MG, et al. Acute flank pain: comparison of non-contrast-enhanced CT and intravenous urography. Radiology. 1995;194(3):789–94.
Sommer F, Jeffrey R Jr, Rubin G, et al. Detection of ureteral calculi in patients with suspected renal colic: value of reformatted noncontrast helical CT. AJR. Am J Roentgenol. 1995;165(3):509–13.
Mattsson T. Frequency and location of pelvic phleboliths. Clin Radiol. 1980;31(1):115–8.
Thomas E, Witte Y, Thomas J, Arvis G. Cacchi and Ricci’s disease. Radiology, epidemiology and biology. Prog Urol. 2000;10(1):29–35.
Nitti VW, Brucker B. Urodynamic and video-urodynamic evaluation of the lower urinary tract. Campbell-Walsh Urol. 2012;10:2010–9.
Rob S, Bryant T, Wilson I, Somani BK. Ultra low dose, low dose and standard dose CTKUB: is there a difference? results from a systematic review of literature. Clin Radiol. 2017;72(1):11–5.
Featherstone NC, Somani BK, Griffin S. Ureteroscopy and laser stone fragmentation (URSL) for large (>1cm) paediatric stones: outcomes from a university teaching hospital. J Paediatr Urol. 2017;13(2):202.e1–7.
Ishii H, Aboumarzouk O, Somani BK. Current status of ureteroscopy for stone disease in pregnancy. Urolithiasis. 2014;42(1):1–7.
Ishii H, Couzins M, Aboumarzouk O, Biyani CS, Somani BK. Outcomes of systematic literature review of ureteroscopy for stone disease in the obese and morbidly obese population. J Endourol. 2016;30(2):135–45.
Somani BK, Robertson A, Kata SG. Decreasing cost of flexible ureterorenoscopic procedures: cost volume relationship. Urology. 2011;78(3):528–30.
Pietropaolo A, Proietti S, Geraghty R, et al. Trends of ‘urolithiasis: interventions, simulation and laser technology’ over the last 16 years (2000–2015) as published in the literature (PubMed): a systematic review. WJU. 2017;35(11):1651–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Patrick Rice and Sarah Prattley each declare no potential conflicts of interest.
Bhaskar K Somani is a section editor for Current Urology Reports.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Endourology
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rice, P., Prattley, S. & Somani, B.K. ‘Negative Ureteroscopy’ for Stone Disease: Evidence from a Systematic Review. Curr Urol Rep 20, 13 (2019). https://doi.org/10.1007/s11934-019-0878-4
Published:
DOI: https://doi.org/10.1007/s11934-019-0878-4