Abstract
Purpose of Review
Provision of mental health services through digital technologies (e-mental health) can potentially expand access to treatments for personality disorders (PDs). We evaluated studies on e-mental health for PDs published over the last 3 years (2019–2022).
Recent Findings
Studies published in English that used e-mental health to treat people with PDs or PD-related symptoms were identified. We identified 19 studies, including four randomized controlled trials and one meta-analysis. Most interventions were based on Dialectical Behavior Therapy and delivered through smartphone applications for adults with Borderline Personality Disorder [BPD] or related symptoms. User experiences of the interventions were generally positive. Evidence for efficacy was limited.
Summary
The current literature on e-mental health for PDs is limited in scope. Research in understudied populations and randomized controlled trials designed to establish efficacy are warranted. It is not yet clear whether e-mental health may be helpful for the treatment of PDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Personality disorders (PDs) are characterized by extreme, rigid, and enduring personality traits that significantly deviate from cultural norms and cause significant distress and/or functional impairment [1]. The American Psychiatric Association’s Diagnostic and Statistical Manual (DSM-5) [1] defines 10 specific PDs that vary in their cardinal features. For example, Borderline Personality Disorder (BPD) is characterized by intense fear of abandonment along with instability in interpersonal relationships, self-identity, affect, and behavior (e.g., impulsivity) [1]. Schizoid PD, in contrast, is characterized by detachment within social relationships along with a restricted range of emotional expression and a decreased desire for emotional closeness [1]. Approximately 8% of people worldwide suffer from PDs [2]. Those with PDs have elevated rates of comorbid psychiatric disorders and may experience functional impairment, including in social relationships and career development [3]. With the high utilization of health services and occupational impairment, the economic burden associated with PDs is large, exceeding the economic costs of even more prevalent psychiatric disorders (e.g., depressive disorders) [4, 5]. Efficacious and cost-effective treatments are needed given the prevalence and disease burden of PDs.
Evidence-based treatments exist for some PDs. For example, dialectical behavior therapy (DBT) has been recognized as the gold standard for the treatment of BPD [6, 7]. However, access to traditional therapist-delivered psychotherapies such as DBT may be limited for many people due to costs, mental health stigma, and logistical barriers such as travel required to attend therapy appointments [8, 9]. For many, therapists trained in DBT are simply not accessible. E-mental health, which provides mental health services through digital information and communication technologies (e.g., smartphone applications, the Internet), has been widely used to promote mental health in the past decade [10, 11]. E-mental health has the potential to increase cost-effectiveness [12], expand access to mental health resources [13], reduce the stigma associated with seeking traditional psychotherapy [14], and provide personalized psychological services [15].
The use of e-mental health in the treatment of PDs has also gained popularity in the past decade and for potentially good reason. As early as 2011, a pilot study suggested that smartphone-delivered DBT effectively reduced emotional distress and substance use craving in BPD patients [16]. The authors of this study highlighted the potential of employing e-mental health to increase the application of DBT skills within daily life. From this perspective, e-mental health may not only expand access to intervention approaches for PDs but also increase the integration of interventions within daily life. This integration may be particularly welcome given the pervasive nature of PDs which are, by definition, characterized by rigid and enduring features that manifest regularly within daily life [1].
Despite this potential, recently published reviews have reported that the effectiveness of e-mental health for PDs (specifically BPD) did not outperform in-person treatments and wait-list comparisons [17••] and most studies on e-mental health for PDs were in the initial stages (e.g., feasibility/usability testing) [18••, 19]. Given the rapid rate of publication in the area of e-mental health, particularly during the COVID-19 pandemic [20], there is a need for an updated review of this growing literature. Moreover, previous reviews did not include protocol papers that can help understand planned studies and highlight the directions that the field is heading.
The current systematic review aims to provide an up-to-date depiction of the literature on e-mental health for PDs, focusing on the last 3 years (2019–2022). For the purposes of the current review, e-mental health was defined to include mental health interventions delivered through smartphones, websites, and other information and communication technologies. Synchronous therapy delivered via telephone or video conferencing (i.e., telehealth/telepsychiatry) was excluded. To most fully characterize recent research on e-mental health for PDs, we did not set any restrictions based on study design (i.e., reviews, perspectives/commentaries, qualitative studies, and protocol papers were included).
Method
Protocol and Registration
The current review was preregistered through the Open Science Framework (https://osf.io/wfu7r/) and complied with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [21].
Eligibility Criteria
Inclusion criteria were quantitative, qualitative, and mixed-methods studies that used e-mental health to treat people with PDs (e.g., BPD) or that focused on technology-delivered interventions commonly used for the treatment of PDs (e.g., DBT for BPD) regardless of whether they included a sample restricted to people with PDs. Theoretical reviews and perspective/opinion articles on e-mental health for people with PDs were also included. We did not restrict based on publication status (i.e., dissertations were eligible). Studies on synchronous interventions delivered via telephone or video conferencing (i.e., telehealth/telepsychiatry) were not included as the evidence for these is well established. Studies published in languages other than English were excluded.
Information Sources
We searched PubMed for studies on e-mental health for people with PDs. The database was searched from January 1, 2019, to March 7, 2022.
Search
We paired search terms related to e-mental health with terms related to PDs. Search terms were (“smartphone” OR “smart phone” OR “mobile phone” OR “cellular phone” OR “cell phone” OR “mobile app” OR “mobile device” OR “mobile-based” OR “mobile health” OR “mhealth” OR “m-health” OR “iphone” OR “android” OR “tablet” OR “Internet”) AND (“personality disorder” OR “dialectical behavior therapy” OR “dbt” OR “dialectical behavioral therapy”).
Study Selection
Titles and abstract screening and full-text screening were conducted by the first author (QX) in consultation with the corresponding author (SG). A consensus was reached between the two authors on final decisions for inclusion/exclusion.
Data Collection Process
Study-level data were coded using the standardized spreadsheets developed for the review. The first author (QX) who has experience conducting systematic reviews completed all study-level data coding in consultation with the corresponding author (SG).
Data Items
The following variables were coded for each study: study design (e.g., review, randomized controlled trial/controlled trial); sample characteristics including sample size, clinical condition (e.g., BPD patients), age, country of origin, percentage of female; intervention characteristics including intervention type (e.g., DBT), basis (e.g., DBT-based), and format (e.g., email-based; app-based); outcome type (e.g., usability, BDP symptoms); and main results.
Summary Measures
Since the current study is a systematic review rather than a meta-analysis, no summary measures were used.
Synthesis of Results
The main results of each study were summarized qualitatively.
Results
Study Selection
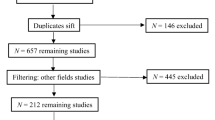
One hundred and thirty-two articles were retrieved from PubMed using the search terms. Nineteen eligible studies were included in the current review. Among the excluded studies, 107 were excluded during title and abstract screening (57 were not related to e-mental health, and 50 were not related to PDs). Six studies were excluded during full-text screening (three were not related to e-mental health and three were not related to PDs). See Fig. 1 for the PRISMA flow diagram.
Study Characteristics
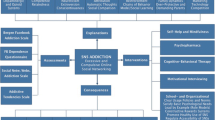
Among the 19 included studies, four (21.05%) were randomized controlled trials (RCTs) [22•–25], one (5.26%) was a nonrandomized controlled trial (NCT) [26], three (15.69%) were RCT protocols [27•–29], six (31.58%) were single-group intervention studies [30–35], two (10.53%) were intervention development studies [36, 37•], and three (15.79%) were reviews [17••, 18••, 38]. The majority of intervention studies (k = 12 out of 16, 75.00%) used DBT techniques. Specifically, nine out of the 16 intervention studies (56.25%) were based on DBT (i.e., the interventions were DBT) [23–27•, 30, 32, 34, 35], and three (18.75%) were DBT-informed (i.e., included DBT elements) [29, 31, 37•]. Only four intervention studies (25.00%) did not use DBT techniques [22•, 28, 33, 36]. For the three reviews, one (33.33%) included only DBT-based studies [38], and two (66.67%) did not restrict the interventions to DBT [17••, 18•]. In terms of the delivery format, most studies used smartphone apps to deliver the interventions. Twelve (63.16%) studies were smartphone app-based [17••, 23, 24, 27•, 28, 30–32, 34, 36–38•], five (26.32%) were Internet-based [22•, 25, 29, 33, 35], one (5.26%) was email-based [26], and one review (5.26%) examined various forms of technology (e.g., virtual reality, mobile apps, computer-assisted) [18••]. The vast majority of the studies (k = 18 out of 19, 94.74%) were conducted in North America and Europe, only one study [24] was conducted in Argentina.
The average age of the samples included in the current review was 30.11 years old. Samples were on average majority female (83.06%). Among the 19 samples included, nine (56.25%) had BPD diagnosis [18••, 22•, 23, 26, 28, 31–34], six (37.50%) had common symptoms of BPD (e.g., self-injury, suicidality) [17••, 24, 25, 27•, 29, 35], one (6.25%) included various PDs (not limited to BPD) [30], two (12.50%) included people assisting in technology development [36, 37•], and one (6.25%) focused on smartphone apps rather than participants [38•].
The design and sample characteristics of included studies are reported in Table 1. The outcomes and results of included studies are shown in Table 2. Below, we discuss the included studies based on their study design.
Randomized Controlled Trials (RCTs) and Nonrandomized Controlled Trials (NCTs)
There were five eligible RCTs and NCTs in the current review. Four [23, 24–26] were based on DBT and one [22•] was based on schema therapy. Two studies delivered interventions through smartphone apps [23, 24], two through the Internet [22•, 25], and one through email [26]. These trials measured a wide variety of outcomes including aspects of feasibility and acceptability (e.g., treatment compliance, dropout rate, acceptability), general outcomes (e.g., disease burden, health care utilization), and BPD symptom-related outcomes (e.g., suicidality, emotion regulation). Four studies reported results comparing an e-mental health condition with a control condition [22•–24, 26]. Results of comparisons between e-mental health interventions and control conditions provided mixed results. We discuss the results of these four studies one by one below. One study [25] involved secondary data analysis of an RCT testing Internet-delivered DBT (iDBT) [39]. However, the included study [25] did not examine differences between the iDBT and control group, but instead focused on predictions of dropout from iDBT based on clinical characteristics and user experience. Results indicated that technological and unknown barriers (i.e., participants were unreachable when user experience was being assessed) as well as perceived usefulness were associated with dropout.
As noted, four studies directly compared e-mental health interventions with control conditions for people with PDs or PD-related symptoms. All four studies focused on adult samples. Laursen et al. [23] compared DBT delivered via a mobile diary app with paper-based diary cards. Relative to the paper-based diary card condition, the app group showed improved effects on suicidal behavior but inferior effects on measures of depression, quality-adjusted life years, and borderline severity, with no differences between the groups on health care utilization. Rodante et al. [24] evaluated the preliminary effectiveness of augmenting DBT with an app compared to DBT alone. Combining DBT with an app produced superior effects on suicide and self-harm relative to DBT alone. Moreover, the DBT app was rated as having good acceptability by participants. Alavi et al. [26] compared the effectiveness of email-delivered DBT with in-person DBT in a nonrandomized design. Emotion regulation difficulties improved from pre- to post-test in both conditions, but the two groups did not differ in changes in emotion regulation difficulties. Klein et al. [22•] studied the relative effectiveness and safety of adding an Internet-based schema therapy to treatment-as-usual (TAU) and TAU only. Results showed that the addition of an Internet-based schema therapy did not improve BPD severity or serious adverse events (e.g., self-injury, drug intoxication) compared to TAU only. In summary, among the four studies comparing e-mental health with a control condition, one showed a superior effect of the e-mental health intervention to the control condition [24], two did not find differences in effectiveness [22•, 26], and one showed a mixture of results favoring the e-mental health or the control condition depending on the outcome measure [23].
RCT Protocols
There were three eligible RCT protocols. Han et al. [27•] aimed to compare a DBT-based smartphone app with a matched attention control. They also planned to understand user experiences of the app through qualitative interviews. According to the protocol, this would be the first trial to examine the effectiveness of a smartphone app-based DBT intervention on suicidal and related mental health outcomes for young adults. Kaess et al. [29] reported the development and evaluation plan for an online intervention informed by cognitive behavioral therapy and DBT for youth with repetitive non-suicidal self-injury. According to the authors, it would be the first RCT to apply an Internet-based intervention for youth with self-injury. Helweg-Jørgensen et al. [28] aimed to evaluate the effectiveness of a smartphone app-based self-monitoring intervention compared with a pen-and-paper self-monitoring (control condition) during DBT treatment for BPD. The authors reported that this would be the first trial to evaluate an app-based self-monitoring system for BPD treatment.
Single Group Intervention Studies
There were six eligible single-group intervention studies. Four were DBT-based [30, 32, 34, 35], one was DBT-informed [31], and one was non-DBT (schema therapy) [33]. In terms of the delivery format, four were app-based [30–32, 34] and two were Internet-based [33, 35]. Five out of the six studies evaluated aspects of feasibility and acceptability of the interventions [30–34]. In general, participants had positive experiences with the interventions (e.g., high satisfaction, high ratings on usability). Among the six studies, Whiteside et al. [35] was the only one that evaluated effectiveness. They found reductions in suicidal thoughts and negative emotions after visiting the website focused on suicidality.
Intervention Development Studies
There were two eligible intervention development studies. O’Grady et al. [37•] developed and tested a smartphone app that provided interactive safety planning and promoted DBT skill generalization for people with suicide risk. The app was designed as an adjunct to face-to-face therapy by a multidisciplinary team of experts (e.g., computer science, clinical psychology). Clinician input was used in the iterative design process to finalize the app. In terms of usability, students with technology experience provided overall positive evaluations of the app, especially on its user privacy protection and user interface design. Derks et al. [36] developed a wearable biofeedback app to facilitate emotional awareness in people with BPD. Multiple user groups, including patients, therapists, and user-center design experts, were involved in the app development process. The three user groups perceived the app to be useful and easy to use.
Reviews
Three reviews were included. One systematic review [38•] focused on 21 DBT apps downloadable in Google Play and iOS app stores and found that the average user “star” rating was good (4.39 out of 5). However, ratings of user experience made by two independent reviewers on the Mobile App Rating Scale found usability and acceptability to be on average minimally acceptable (3.41 out of 5.00). Frías et al. [18••] reviewed technology-delivered psychosocial interventions for people with BPD. They found that the majority of the interventions were designed as an adjunct to traditional therapy and about half of the interventions were DBT-based. The review also suggested that the focus of almost all studies was on the tests of feasibility, acceptance, and usability, that is the initial phases of the clinical research cycle.
The clearest empirical evaluation of e-mental health for PDs came from a meta-analysis of seven RCTs conducted by Ilagan et al. [17••]. The authors found that smartphone apps targeting BPD symptoms were not superior to control conditions (Hedges’ g = − 0.05, 95% confidence interval [− 0.24, 0.14], where a lower value favors the control condition). Of note, only one of the control conditions was a waitlist, with the remainder involving various active interventions including TAU conditions (e.g., specialized outpatient suicide prevention clinic; [40]). Thus, the null results may indicate that e-mental health interventions are not effective at augmenting active controls rather than that e-mental health interventions do not improve outcomes in the absence of treatment.
Discussion
The current study aimed to summarize recent developments in the use of e-mental health for the management of PDs and PD-related symptoms. As with mental health care in general [41], there is a clear interest in applying digital technologies to expand access to treatment options in the area of PDs and to augment existing treatments and increase access to care.
Our search produced 19 articles published since 2019 that focused on this topic. The modal study was focused on DBT or DBT techniques, employed a smartphone-based intervention, was conducted in North America or Europe, included adult females, and included participants with BPD or common symptoms of BPD. The recent literature in this area provides some encouragement: studies evaluating intervention feasibility and acceptability tended to report promising results, clinician and expert evaluation of e-mental health technologies provided positive evaluations, and currently available DBT apps have good user ratings and minimally acceptable expert-rated usability and acceptability.
At once, when restricting discussion to the most rigorous design for evaluating effectiveness (that is, RCTs), the actual empirical evidence demonstrating the efficacy of e-mental health for PDs appears limited. Of the three RCTs reviewed, one found that augmenting DBT with an app improved outcomes over DBT alone [24], one found that augmenting TAU with Internet-based schema therapy did not improve outcomes [22•], and one found that therapist-delivered DBT paired with a mobile diary app improved some but not all outcomes relative to therapist-delivered DBT paired with paper diary cards [23]. This lack of robust evidence for efficacy was mirrored in the one meta-analysis of RCTs included in this review. In a meta-analysis of seven RCTs, Ilagan et al. found that smartphone apps targeting BPD symptoms did not outperform control conditions, most of which involved forms of in-person TAU [17••]. This lack of robust evidence is not unique to PDs and recent broad reviews of digital mental health suggest similar challenges when results are compared to a more rigorous and randomized control group [11].
Ultimately, it is not possible at present to draw definitive conclusions regarding the potential of e-mental health for PDs. The recent scientific literature on this topic provides a mixture of encouraging and at least somewhat discouraging results (i.e., null effects from meta-analysis; [17••]). However, several specific future directions for work in this area follow from the current literature reviewed.
Future Directions
One key future direction is continuing to examine e-mental health in populations that have been to date understudied. It was encouraging to see RCT protocol papers focused on e-mental health for youth and adolescents. This may be a population particularly amenable to e-health interventions and with clear mental health needs [42, 43], particularly during the COVID-19 pandemic [44]. It may be valuable to investigate the effects of e-mental health for people with PDs living in middle- and low-income countries where access to DBT is even more limited and may often be non-existent. Given the potentially limited access to mental health care in these countries [45], e-mental health may be a cost-effective means for reducing the burden of disease associated with PDs [46]. As noted, e-mental health interventions may well provide benefits above and beyond no treatment, even if they fail to outperform other interventions or demonstrate benefits above and beyond TAU conditions. However, it remains unclear if this benefit is unique to these digital interventions or more driven by placebo, social interactions involved in partaking in a study, or simply interacting with technology. Still, in contexts where TAU is not available, e-mental health may be highly attractive. There also may be PDs and PD-related symptoms other than BPD that are amenable to e-mental health (e.g., antisocial PD, avoidant PD) that have as yet not been studied.
Another future direction may be the evaluation of more sophisticated, intensive, and/or integrated e-mental health approaches. This may involve the incorporation of greater provider guidance (which has been shown to improve outcomes for app-supported smartphone interventions; [47]). It could also involve the use of advancements in e-mental health technologies, such as passive sensing. This might include features that alert participants prior to high-risk behaviors and offer responsive and personalized support. Such innovations have been effectively implemented to reduce risky behaviors in other populations (e.g., alert participants recovering from alcohol use disorders when they are geographically proximal to a place they used to drink; [48]). E-mental health interventions including various just-in-time adaptive and ecological momentary interventions such as nudges delivered via text messages may help manage the impulsivity that can be associated with some PDs [1] as they have for supporting behavior change generally [49–51].
An important question to consider for future RCTs and meta-analyses is which control condition should be used. While ultimately comparisons with other active interventions including comparisons with robust TAU conditions will be essential for establishing the efficacy of e-mental health for PD beyond non-specific factors and for guiding treatment decision making, less rigorous comparisons including comparisons with waitlists and no treatment controls may be informative at the current stage. That said, it may not always be ethically feasible to randomize participants to no treatment (e.g., if participants are reporting elevated risk for suicidality or self-harm), in which case some degree of TAU may be essential.
Limitations
The current study has several limitations. First, our review focused exclusively on the past several years and may have neglected to include relevant studies published before 2019. As noted in the introduction, research on apps for PD has been active for over a decade [16]. We also only searched PubMed and may have missed studies not indexed there. The number of studies evaluated was relatively modest and insufficient to allow a quantitative synthesis of results (i.e., meta-analysis). The specific samples of studies retrieved were relatively homogeneous (i.e., primarily focused on smartphone-based interventions including DBT-related content for adult females in North America or Europe) and included relatively modest sample sizes in the RCTs which may have limited statistical power to detect differences between the e-mental health conditions and the control groups.
Conclusions
The current study provided mixed evidence for the potential of e-mental health for the treatment of PDs and PD-related symptoms. On the one hand, it appears that these approaches are feasible and acceptable to participants and are being designed in some instances using best practices (e.g., user-centered design, multidisciplinary teams, incorporating feedback from patients and providers; [36, 37•]). At once, the actual empirical evidence demonstrating through RCTs that e-mental health interventions improve outcomes for people with PDs or PD-related symptoms is currently lacking. We are hopeful that future large-scale RCTs conducted with attention to the scientific meaning of various control condition types, studies conducted with youth and adolescents, and studies conducted in low- and middle-income countries may help clarify whether e-mental health may be able to fulfill its potential to reduce the disease burden associated with PDs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Winsper C, Bilgin A, Thompson A, Marwaha S, Chanen AM, Singh SP, et al. The prevalence of personality disorders in the community: a global systematic review and meta-analysis. Br J Psychiatry. 2020;216(2):69–78.
Moran P, Romaniuk H, Coffey C, Chanen A, Degenhardt L, Borschmann R, et al. The influence of personality disorder on the future mental health and social adjustment of young adults: a population-based, longitudinal cohort study. Lancet Psychiatry. 2016;3(7):636–45.
Bode K, Vogel R, Walker J, Kröger C. Health care costs of borderline personality disorder and matched controls with major depressive disorder: a comparative study based on anonymized claims data. Eur J Health Econ. 2017;18(9):1125–35.
Wagner T, Assmann N, Köhne S, Schaich A, Alvarez-Fischer D, Borgwardt S, et al. The societal cost of treatment-seeking patients with borderline personality disorder in Germany. Eur Arch Psychiatry Clin Neurosci. 2022;272(4):741–52.
Linehan MM. Skills training manual for treating borderline personality disorder. Guilford Press; 1993.
Stoffers JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2012;(8):CD005652.
Mohr DC, Hart SL, Howard I, Julian L, Vella L, Catledge C, et al. Barriers to psychotherapy among depressed and nondepressed primary care patients. Ann Behav Med. 2006;32(3):254–8.
Mohr DC, Ho J, Duffecy J, Baron KG, Lehman KA, Jin L, et al. Perceived barriers to psychological treatments and their relationship to depression. J Clin Psychol. 2010;66(4):394–409.
Cunningham JA, Gulliver A, Farrer L, Bennett K, Carron-Arthur B. Internet interventions for mental health and addictions: current findings and future directions. Curr Psychiatry Rep. 2014;16(12):521.
Goldberg SB, Lam SU, Simonsson O, Torous J, Sun S. Mobile phone-based interventions for mental health: a systematic meta-review of 14 meta-analyses of randomized controlled trials. PLOS Digit Health. 2022;1(1): e0000002.
Donker T, Blankers M, Hedman E, Ljótsson B, Petrie K, Christensen H. Economic evaluations of Internet interventions for mental health: a systematic review. Psychol Med. 2015;45(16):3357–76.
Raney L, Bergman D, Torous J, Hasselberg M. Digitally driven integrated primary care and behavioral health: how technology can expand access to effective treatment. Curr Psychiatry Rep. 2017;19(11):86.
Kim HM, Xu Y, Wang Y. Overcoming the mental health stigma through m-health apps: results from the healthy minds study. Telemed J E Health. 2022.
Perna G, Grassi M, Caldirola D, Nemeroff CB. The revolution of personalized psychiatry: will technology make it happen sooner? Psychol Med. 2018;48(5):705–13.
Rizvi SL, Dimeff LA, Skutch J, Carroll D, Linehan MM. A pilot study of the DBT coach: an interactive mobile phone application for individuals with borderline personality disorder and substance use disorder. Behav Ther. 2011;42(4):589–600.
•• Ilagan GS, Iliakis EA, Wilks CR, Vahia IV, Choi-Kain LW. Smartphone applications targeting borderline personality disorder symptoms: a systematic review and meta-analysis. Borderline Personal Disord Emot Dysregul. 2020;7:12. This meta-analytic review evaluated the effectiveness of e-mental health for BPD symptoms relative to control conditions (the majority were active/TAU controls) and found that smartphone apps targeting BPD symptoms were not superior to control conditions.
•• Frías Á, Solves L, Navarro S, Palma C, Farriols N, Aliaga F, et al. Technology-based psychosocial interventions for people with borderline personality disorder: a scoping review of the literature. Psychopathology. 2020;53(5–6):254–63. This study reviewed technology-delivered psychosocial interventions for people with BPD and found that the focus of almost all studies was feasibility, acceptability, and usability (i.e., the initial phases of the clinical research cycle).
van der Boom B, Boumparis N, Donker T, de Beurs D, Arntz A, Riper H. Internet-delivered interventions for personality disorders - a scoping review. Internet Interv. 2022;28: 100525.
Rauschenberg C, Schick A, Hirjak D, Seidler A, Paetzold I, Apfelbacher C, et al. Evidence synthesis of digital interventions to mitigate the negative impact of the COVID-19 pandemic on public mental health: rapid meta-review. J Med Internet Res. 2021;23(3): e23365.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
• Klein JP, Hauer-von Mauschwitz A, Berger T, Fassbinder E, Mayer J, Borgwardt S, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771. This study evaluated the relative effectiveness and safety of adding an Internet-based schema therapy to TAU versus TAU only. Results showed that the addition of an Internet-based schema therapy did not improve BPD severity or serious adverse events compared to TAU only.
Laursen SL, Helweg-Jørgensen S, Langergaard A, Søndergaard J, Sørensen SS, Mathiasen K, et al. Mobile diary app versus paper-based diary cards for patients with borderline personality disorder: economic evaluation. J Med Internet Res. 2021;23(11): e28874.
Rodante DE, Kaplan MI, Olivera Fedi R, Gagliesi P, Pascali A, José Quintero PS, et al. CALMA, a mobile health application, as an accessory to therapy for reduction of suicidal and non-suicidal self-injured behaviors: a pilot cluster randomized controlled trial. Arch Suicide Res. 2020;1–18.
Wilks CR, Yin Q, Zuromski KL. User experience affects dropout from internet-delivered dialectical behavior therapy. Telemed J E Health. 2020;26(6):794–7.
Alavi N, Stephenson C, Rivera M. Effectiveness of delivering dialectical behavioral therapy techniques by email in patients with borderline personality disorder: nonrandomized controlled trial. JMIR Ment Health. 2021;8(4): e27308.
• Han J, McGillivray L, Wong QJ, Werner-Seidler A, Wong I, Calear A, et al. A Mobile Health Intervention (LifeBuoy App) to help young people manage suicidal thoughts: protocol for a mixed-methods randomized controlled trial. JMIR Res Protoc. 2020;9(10):e23655. This protocol aimed to evaluate the efficacy and user experience of a DBT-based smartphone app for young adults compared with a matched attentional control.
Helweg-Jørgensen S, Beck Lichtenstein M, Fruzzetti AE, Møller Dahl C, Pedersen SS. Daily self-monitoring of symptoms and skills learning in patients with borderline personality disorder through a mobile phone app: protocol for a pragmatic randomized controlled trial. JMIR Res Protoc. 2020;9(5): e17737.
Kaess M, Koenig J, Bauer S, Moessner M, Fischer-Waldschmidt G, Mattern M, et al. Self-injury: Treatment, Assessment, Recovery (STAR): online intervention for adolescent non-suicidal self-injury - study protocol for a randomized controlled trial. Trials. 2019;20(1):425.
Austin SF, Jansen JE, Petersen CJ, Jensen R, Simonsen E. Mobile app integration into dialectical behavior therapy for persons with borderline personality disorder: qualitative and quantitative study. JMIR Ment Health. 2020;7(6): e14913.
Frías Á, Palma C, Salvador A, Aluco E, Navarro S, Farriols N, et al. B·RIGHT: usability and satisfaction with a mobile app for self-managing emotional crises in patients with borderline personality disorder. Australas Psychiatry. 2021;29(3):294–8.
Helweg-Joergensen S, Schmidt T, Lichtenstein MB, Pedersen SS. Using a Mobile diary app in the treatment of borderline personality disorder: mixed methods feasibility study. JMIR Form Res. 2019;3(3): e12852.
Köhne S, Schweiger U, Jacob GA, Braakmann D, Klein JP, Borgwardt S, et al. Therapeutic relationship in eHealth-a pilot study of similarities and differences between the online program priovi and therapists treating borderline personality disorder. Int J Environ Res Public Health. 2020;17(17):6436.
Schiffler T, Seiler-Ramadas R, Štefanac S, Haider S, Mües HM, Grabovac I. Implementation of a mobile DBT app and its impact on suicidality in transitional age youth with borderline personality disorder: a qualitative study. Int J Environ Res Public Health. 2022;19(2):701.
Whiteside U, Richards J, Huh D, Hidalgo R, Nordhauser R, Wong AJ, et al. Development and evaluation of a web-based resource for suicidal thoughts: NowMattersNow.org. J Med Internet Res. 2019;21(5):e13183.
Derks YP, Klaassen R, Westerhof GJ, Bohlmeijer ET, Noordzij ML. Development of an ambulatory biofeedback app to enhance emotional awareness in patients with borderline personality disorder: multicycle usability testing study. JMIR Mhealth Uhealth. 2019;7(10): e13479.
• O’Grady C, Melia R, Bogue J, O’Sullivan M, Young K, Duggan J. A Mobile Health Approach for Improving Outcomes in Suicide Prevention (SafePlan). J Med Internet Res. 2020;22(7):e17481. This study developed and tested a DBT-informed smartphone app for people with suicide risk by incorporating feedback from a multidisciplinary team of experts (e.g., computer science, clinical psychology). Clinician input was used in the iterative design process to finalize the app.
• Wilks CR, Gurtovenko K, Rebmann K, Williamson J, Lovell J, Wasil AR. A systematic review of dialectical behavior therapy mobile apps for content and usability. Borderline Personal Disord Emot Dysregul. 2021;8(1):29. This systematic review evaluated the user experiences of DBT apps. It was found that the average user “star” rating was good. However, ratings of user experience made by two independent reviewers found usability and acceptability to be on average minimally acceptable.
Wilks CR, Lungu A, Ang SY, Matsumiya B, Yin Q, Linehan MM. A randomized controlled trial of an Internet delivered dialectical behavior therapy skills training for suicidal and heavy episodic drinkers. J Affect Disord. 2018;232:219–28.
O’Toole MS, Arendt MB, Pedersen CM. Testing an app-assisted treatment for suicide prevention in a randomized controlled trial: effects on suicide risk and depression. Behav Ther. 2019;50(2):421–9.
Torous J, Jän Myrick K, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment Health. 2020;7(3): e18848.
Aschbrenner KA, Naslund JA, Tomlinson EF, Kinney A, Pratt SI, Brunette MF. Adolescents’ use of digital technologies and preferences for mobile health coaching in public mental health settings. Front Public Health. 2019;7:178.
Uhlhaas P, Torous J. Digital tools for youth mental health. NPJ Digit Med. 2019;2:104.
Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–20.
Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370(9593):1164–74.
McCool J, Dobson R, Whittaker R, Paton C. Mobile health (mHealth) in low- and middle-income countries. Annu Rev Public Health. 2022;43:525–39.
Linardon J, Cuijpers P, Carlbring P, Messer M, Fuller-Tyszkiewicz M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry. 2019;18(3):325–36.
Gustafson DH, McTavish FM, Chih MY, Atwood AK, Johnson RA, Boyle MG, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiat. 2014;71(5):566–72.
Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15(Pt 1):1–39.
Myin-Germeys I, Klippel A, Steinhart H, Reininghaus U. Ecological momentary interventions in psychiatry. Curr Opin Psychiatry. 2016;29(4):258–63.
Wang L, Miller LC. Just-in-the-moment adaptive interventions (JITAI): a meta-analytical review. Health Commun. 2020;35(12):1531–44.
Funding
Dr. Goldberg was supported by the National Center for Complementary & Integrative Health of the National Institutes of Health under Award Number K23AT010879 and the Hope for Depression Research Foundation Defeating Depression Award. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Personality Disorders
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xie, Q., Torous, J. & Goldberg, S.B. E-Mental Health for People with Personality Disorders: A Systematic Review. Curr Psychiatry Rep 24, 541–552 (2022). https://doi.org/10.1007/s11920-022-01360-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-022-01360-1