Abstract
Purpose of Review
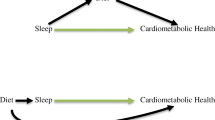
Inflammation has emerged as an important biological process in the development of many age-related diseases that occur at different frequencies in men and women. The aim of this review was to examine the current evidence linking stress and sleep with inflammation with a focus on sex differences.
Recent Findings
Psychosocial stress that occurs either acutely or chronically is associated with elevated levels of systemic inflammation. While not as robust, insufficient sleep, particularly sleep disturbances, appears to be associated with higher levels of inflammatory activity as well. In several contexts, associations of stress and insufficient sleep with inflammation appear stronger in women than in men. However, this should be interpreted with caution as few studies test for sex differences.
Summary
Stress and poor sleep often predict elevations in systemic inflammation. While there is some evidence that these associations are stronger in women, findings are largely mixed and more systematic investigations of sex differences in future studies are warranted.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Scrivo R, Vasile M, Bartosiewicz I, Valesini G. Inflammation as “common soil” of the multifactorial diseases. Autoimmun Rev. 2011;10(7):369–74. https://doi.org/10.1016/j.autrev.2010.12.006.
Hunter TM, Boytsov NN, Zhang X, Schroeder K, Michaud K, Araujo AB. Prevalence of rheumatoid arthritis in the United States adult population in healthcare claims databases, 2004-2014. Rheumatol Int. 2017;37(9):1551–7. https://doi.org/10.1007/s00296-017-3726-1.
Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. 2016;16(1):22–34. https://doi.org/10.1038/nri.2015.5.
Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull. 2017;143(8):783–822. https://doi.org/10.1037/bul0000102.
Mikkola TS, Gissler M, Merikukka M, Tuomikoski P, Ylikorkala O. Sex differences in age-related cardiovascular mortality. PLoS One. 2013;8(5):e63347. https://doi.org/10.1371/journal.pone.0063347.
• Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38. https://doi.org/10.1038/nri.2016.90 This paper reviews sex differences in immune responses including inflammation.
Rainville JR, Tsyglakova M, Hodes GE. Deciphering sex differences in the immune system and depression. Front Neuroendocrinol. 2017;50:67–90. https://doi.org/10.1016/j.yfrne.2017.12.004.
Bekhbat M, Neigh GN. Sex differences in the neuro-immune consequences of stress: focus on depression and anxiety. Brain Behav Immun. 2018;67:1–12. https://doi.org/10.1016/j.bbi.2017.02.006.
Duma D, Collins JB, Chou JW, Cidlowski JA. Sexually dimorphic actions of glucocorticoids provide a link to inflammatory diseases with gender differences in prevalence. Sci Signal. 2010;3(143):ra74. https://doi.org/10.1126/scisignal.2001077.
Deak T, Quinn M, Cidlowski JA, Victoria NC, Murphy AZ, Sheridan JF. Neuroimmune mechanisms of stress: sex differences, developmental plasticity, and implications for pharmacotherapy of stress-related disease. Stress. 2015;18(4):367–80. https://doi.org/10.3109/10253890.2015.1053451.
• Epel ES, Crosswell AD, Mayer SE, Prather AA, Slavich GM, Puterman E, et al. More than a feeling: a unified view of stress measurement for population science. Front Neuroendocrinol. 2018;49:146–69. https://doi.org/10.1016/j.yfrne.2018.03.001 This review provides a contemporary theoretical perspective on stress and stress measurement.
Cohen S, Murphy MLM, Prather AA. Ten surprising facts about stressful life events and disease risk. Annu Rev Psychol. 2018;70:577–97. https://doi.org/10.1146/annurev-psych-010418-102857.
Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137(6):959–97. https://doi.org/10.1037/a0024768.
• Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-alpha. Mol Psychiatry. 2016;21(5):642–9. https://doi.org/10.1038/mp.2015.67 This paper provides a meta-analytic review of the data linking early life trauma and inflammation.
Baldwin JR, Arseneault L, Caspi A, Fisher HL, Moffitt TE, Odgers CL, et al. Childhood victimization and inflammation in young adulthood: a genetically sensitive cohort study. Brain Behav Immun. 2018;67:211–7. https://doi.org/10.1016/j.bbi.2017.08.025.
• Marsland AL, Walsh C, Lockwood K, John-Henderson NA. The effects of acute psychological stress on circulating and stimulated inflammatory markers: a systematic review and meta-analysis. Brain Behav Immun. 2017;64:208–19. https://doi.org/10.1016/j.bbi.2017.01.011 This paper provides a meta-analytic review of the human literature on acute stress and markers of inflammation.
Prather AA, Carroll JE, Fury JM, McDade KK, Ross D, Marsland AL. Gender differences in stimulated cytokine production following acute psychological stress. Brain Behav Immun. 2009;23(5):622–8. https://doi.org/10.1016/j.bbi.2008.11.004.
• Lockwood KG, Marsland AL, Cohen S, Gianaros PJ. Sex differences in the association between stressor-evoked interleukin-6 reactivity and C-reactive protein. Brain Behav Immun. 2016;58:173–80. https://doi.org/10.1016/j.bbi.2016.07.001 This study demonstrates sex differences in levels of IL-6 in response to acute laboratory stress.
Hackett RA, Hamer M, Endrighi R, Brydon L, Steptoe A. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology. 2012;37(11):1801–9. https://doi.org/10.1016/j.psyneuen.2012.03.016.
Steptoe A, Owen N, Kunz-Ebrecht S, Mohamed-Ali V. Inflammatory cytokines, socioeconomic status, and acute stress responsivity. Brain Behav Immun. 2002;16(6):774–84.
Chiang JJ, Turiano NA, Mroczek DK, Miller GE. Affective reactivity to daily stress and 20-year mortality risk in adults with chronic illness: findings from the National Study of Daily Experiences. Health Psychol. 2018;37(2):170–8. https://doi.org/10.1037/hea0000567.
Sin NL, Graham-Engeland JE, Ong AD, Almeida DM. Affective reactivity to daily stressors is associated with elevated inflammation. Health Psychol. 2015;34(12):1154–65. https://doi.org/10.1037/hea0000240.
• Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2015. https://doi.org/10.1016/j.biopsych.2015.05.014 This paper provides a meta-analytic review of the literature linking sleep and inflammation.
Nowakowski S, Matthews KA, von Kanel R, Hall MH, Thurston RC. Sleep characteristics and inflammatory biomarkers among midlife women. Sleep. 2018;41(5). https://doi.org/10.1093/sleep/zsy049.
Drake CL, Pillai V, Roth T. Stress and sleep reactivity: a prospective investigation of the stress-diathesis model of insomnia. Sleep. 2014;37(8):1295–304. https://doi.org/10.5665/sleep.3916.
Drake CL, Roehrs T, Roth T. Insomnia causes, consequences, and therapeutics: an overview. Depress Anxiety. 2003;18(4):163–76. https://doi.org/10.1002/da.10151.
• Gordon AM, Mendes WB, Prather AA. The social side of sleep: elucidating the links between sleep and social processes. Curr Dir Psychol Sci. 2017;26(5):470–5. https://doi.org/10.1177/0963721417712269 This review discusses the bidirectional links between sleep and social processes including social stress.
Irwin MR, Witarama T, Caudill M, Olmstead R, Breen EC. Sleep loss activates cellular inflammation and signal transducer and activator of transcription (STAT) family proteins in humans. Brain Behav Immun. 2015;47:86–92. https://doi.org/10.1016/j.bbi.2014.09.017.
Irwin M, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med. 2006;166(16):1756–62. https://doi.org/10.1001/archinte.166.16.1756.
Carroll JE, Carrillo C, Olmstead R, Witarama T, Breen EC, Yokomizo M, et al. Sleep deprivation and divergent toll-like receptor-4 activation of cellular inflammation in aging. Sleep. 2015;38(2):205–11. https://doi.org/10.5665/sleep.4398.
Irwin MR, Wang M, Ribeiro D, Cho HJ, Olmstead R, Breen EC, et al. Sleep loss activates cellular inflammatory signaling. Biol Psychiatry. 2008;64(6):538–40. https://doi.org/10.1016/j.biopsych.2008.05.004.
Bixler EO, Papaliaga MN, Vgontzas AN, Lin HM, Pejovic S, Karataraki M, et al. Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. J Sleep Res. 2009;18(2):221–8. https://doi.org/10.1111/j.1365-2869.2008.00713.x.
Lindberg E, Janson C, Gislason T, Bjornsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: can gender differences be explained by differences in psychological status? Sleep. 1997;20(6):381–7.
Goel N, Kim H, Lao RP. Gender differences in polysomnographic sleep in young healthy sleepers. Chronobiol Int. 2005;22(5):905–15. https://doi.org/10.1080/07420520500263235.
Krishnan V, Collop NA. Gender differences in sleep disorders. Curr Opin Pulm Med. 2006;12(6):383–9. https://doi.org/10.1097/01.mcp.0000245705.69440.6a.
Mong JA, Cusmano DM. Sex differences in sleep: impact of biological sex and sex steroids. Philosophical transactions of the Royal Society of London Series B, Biological sciences. 2016;371(1688):20150110. https://doi.org/10.1098/rstb.2015.0110.
Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29(1):85–93.
Bakour C, Schwartz S, O'Rourke K, Wang W, Sappenfield W, Couluris M et al. Sleep duration trajectories and systemic inflammation in young adults: results from the National Longitudinal Study of Adolescent to Adult Health (Add Health). Sleep. 2017;40(11). doi:https://doi.org/10.1093/sleep/zsx156.
Kim TH, Carroll JE, An SK, Seeman TE, Namkoong K, Lee E. Associations between actigraphy-assessed sleep, inflammatory markers, and insulin resistance in the Midlife Development in the United States (MIDUS) study. Sleep Med. 2016;27–28:72–9. https://doi.org/10.1016/j.sleep.2016.07.023.
• Prather AA, Epel ES, Cohen BE, Neylan TC, Whooley MA. Gender differences in the prospective associations of self-reported sleep quality with biomarkers of systemic inflammation and coagulation: findings from the Heart and Soul Study. J Psychiatr Res. 2013;47(9):1228–35. https://doi.org/10.1016/j.jpsychires.2013.05.004 This study shows that poor sleep quality prospectively predicts levels of inflammation in women but not in men.
Suarez EC. Self-reported symptoms of sleep disturbance and inflammation, coagulation, insulin resistance and psychosocial distress: evidence for gender disparity. Brain Behav Immun. 2008;22(6):960–8. https://doi.org/10.1016/j.bbi.2008.01.011.
Miller MA, Kandala NB, Kivimaki M, Kumari M, Brunner EJ, Lowe GD, et al. Gender differences in the cross-sectional relationships between sleep duration and markers of inflammation: Whitehall II study. Sleep. 2009;32(7):857–64.
Kravitz HM, Zhao X, Bromberger JT, Gold EB, Hall MH, Matthews KA, et al. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep. 2008;31(7):979–90.
Mong JA, Baker FC, Mahoney MM, Paul KN, Schwartz MD, Semba K, et al. Sleep, rhythms, and the endocrine brain: influence of sex and gonadal hormones. J Neurosci. 2011;31(45):16107–16. https://doi.org/10.1523/JNEUROSCI.4175-11.2011.
• Bale TL, Epperson CN. Sex differences and stress across the lifespan. Nat Neurosci. 2015;18(10):1413–20. https://doi.org/10.1038/nn.4112 This review discusses the neurobiological differences between men and women in response to stress.
Mazure CM, Jones DP. Twenty years and still counting: including women as participants and studying sex and gender in biomedical research. BMC Womens Health. 2015;15:94. https://doi.org/10.1186/s12905-015-0251-9.
Institue of Medicine. Sex Differences and Implications for Translational Neuroscience Research: Workshop Summary. Washington, DC: National Academies Press; 2011.
Funding
This work was supported by the NIH funding R24AG048024 (ADC, AAP), K01AG057859 (ADC), and R01HL142051 (AAP) and a predoctoral training fellowship T32MH020006 for MRD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sex and Gender Issues in Behavioral Health
Rights and permissions
About this article
Cite this article
Dolsen, E.A., Crosswell, A.D. & Prather, A.A. Links Between Stress, Sleep, and Inflammation: Are there Sex Differences?. Curr Psychiatry Rep 21, 8 (2019). https://doi.org/10.1007/s11920-019-0993-4
Published:
DOI: https://doi.org/10.1007/s11920-019-0993-4