Abstract
Purpose of Review
Chronic abdominal and pelvic visceral pain is an oftentimes difficult to treat pain condition that requires a multidisciplinary approach. This article specifically reviews the interventional treatment options for pain resulting from visceral abdominal and pelvic pain.
Recent Findings
Sympathetic nerve blocks are the main interventional option for the treatment of chronic abdominal and pelvic visceral pain. Initially, nerve blocks are performed, and subsequently, neurolytic injections (alcohol or phenol) are longer term options. This review describes different techniques for sympathetic blockade. Neuromodulation is a potential option via dorsal column stimulation or dorsal root ganglion stimulation. Finally, intrathecal drug delivery is sometimes appropriate for refractory cases.
Summary
This paper will review interventional options for the treatment of chronic abdominal and pelvic visceral pain.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Gschossmann JM, Holtmann G, Mayer EA. Epidemiology and clinical phenomenology of visceral pain. Schmerz. 2002;16(6):447–51.
Sherwin LB, Leary E, Henderson WA. The association of catastrophizing with quality-of-life outcomes in patients with irritable bowel syndrome. Qual Life Res. 2017;26(8):2161–70.
Fornasari D. Pain mechanisms in patients with chronic pain. Clin Drug Investig. 2012;32(Suppl 1):45–52.
Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288(5472):15–9.
Zeilhofer HU, Wildner H, Yevenes GE. Fast synaptic inhibition in spinal sensory processing and pain control. Physiol Rev. 2012;92(1):193–235.
Ossipov MH, et al. Spinal and supraspinal mechanisms of neuropathic pain. Ann N Y Acad Sci. 2000;909:12–24.
Jaggi AS, Singh N. Role of different brain areas in peripheral nerve injury-induced neuropathic pain. Brain Res. 2011;1381:187–201.
Farmer AD, Aziz Q. Visceral pain hypersensitivity in functional gastrointestinal disorders. Br Med Bull. 2009;91:123–36.
Brogan S, Junkins S. Interventional therapies for the management of cancer pain. J Support Oncol. 2010;8(2):52–9.
Gunduz OH, Kenis-Coskun O. Ganglion blocks as a treatment of pain: current perspectives. J Pain Res. 2017;10:2815–26.
Miguel R. Interventional treatment of cancer pain: the fourth step in the World Health Organization analgesic ladder? Cancer Control. 2000;7(2):149–56.
Mohamed SA, Ahmed DG, Mohamad MF. Chemical neurolysis of the inferior hypogastric plexus for the treatment of cancer-related pelvic and perineal pain. Pain Res Manag. 2013;18(5):249–52.
Christo PJ, Mazloomdoost D. Interventional pain treatments for cancer pain. Ann N Y Acad Sci. 2008;1138:299–328.
Koyyalagunta D, et al. The Effectiveness of Alcohol Versus Phenol Based Splanchnic Nerve Neurolysis for the Treatment of Intra-Abdominal Cancer Pain. Pain Physician. 2016;19(4):281–92.
Wood KM. The use of phenol as a neurolytic agent: a review. Pain. 1978;5(3):205–29.
Schroeder ME. Neurolytic nerve block for cancer pain. J Pain Symptom Manage. 1986;1(2):91–4.
Toshniwal GR, Dureja GP, Prashanth SM. Transsacrococcygeal approach to ganglion impar block for management of chronic perineal pain: a prospective observational study. Pain Physician. 2007;10(5):661–6.
Meyerson BA. Neurosurgical approaches to pain treatment. Acta Anaesthesiol Scand. 2001;45(9):1108–13.
Titton RL, et al. Celiac plexus block: a palliative tool underused by radiologists. AJR Am J Roentgenol. 2002;179(3):633–6.
Wang PJ, et al. CT-guided percutaneous neurolytic celiac plexus block technique. Abdom Imaging. 2006;31(6):710–8.
Eisenberg E, Carr DB, Chalmers TC. Neurolytic celiac plexus block for treatment of cancer pain: a meta-analysis. Anesth Analg. 1995;80(2):290–5.
Kambadakone A, et al. CT-guided celiac plexus neurolysis: a review of anatomy, indications, technique, and tips for successful treatment. Radiographics. 2011;31(6):1599–621.
Pereira GA, et al. Celiac plexus block: an anatomical study and simulation using computed tomography. Radiol Bras. 2014;47(5):283–7.
An JW, et al. Alternative method of retrocrural approach during celiac plexus block using a bent tip needle. Korean J Pain. 2015;28(2):109–15.
Sey MS, et al. Effectiveness and safety of serial endoscopic ultrasound-guided celiac plexus block for chronic pancreatitis. Endosc Int Open. 2015;3(1):E56–9.
Smith HS, et al. Intrathecal drug delivery. Pain Physician. 2008;11(2 Suppl):S89–104.
Hilgier M, Rykowski JJ. One needle transcrural celiac plexus block. Single shot or continuous technique, or both. Reg Anesth. 1994;19(4):277–83.
John RS, Dixon B, Shienbaum R. Celiac plexus block, in StatPearls. Treasure Island (FL). 2021.
Kamdar MM, et al. A novel modified retrocrural approach for celiac plexus block: the single-needle retroaortic technique. Reg Anesth Pain Med. 2015;40(5):610–5.
Lieberman RP, Waldman SD. Celiac plexus neurolysis with the modified transaortic approach. Radiology. 1990;175(1):274–6.
Cornman-Homonoff J, et al. Celiac plexus block and neurolysis in the management of chronic upper abdominal pain. Semin Intervent Radiol. 2017;34(4):376–86.
de Oliveira R, dos Reis MP, Prado WA. The effects of early or late neurolytic sympathetic plexus block on the management of abdominal or pelvic cancer pain. Pain. 2004;110(1–2):400–8.
Ahmed A, Arora D. Fluoroscopy-guided neurolytic splanchnic nerve block for intractable pain from upper abdominal malignancies in patients with distorted celiac axis anatomy: an effective alternative to celiac plexus neurolysis — a retrospective study. Indian J Palliat Care. 2017;23(3):274–81.
Suleyman Ozyalcin N, et al. Efficacy of coeliac plexus and splanchnic nerve blockades in body and tail located pancreatic cancer pain. Eur J Pain. 2004;8(6):539–45.
Mercadante S, La Rosa S, Villari P. CT-guided neurolytic splanchnic nerve block by an anterior approach. J Pain Symptom Manage. 2002;23(4):268–70.
Plancarte-Sanchez R, et al. Transdiscal percutaneous approach of splanchnic nerves. Cir Cir. 2003;71(3):192–203.
de Leon-Casasola OA, Kent E, Lema MJ. Neurolytic superior hypogastric plexus block for chronic pelvic pain associated with cancer. Pain. 1993;54(2):145–51.
Stogicza A. Superior and inferior hypogastric plexus blocks.
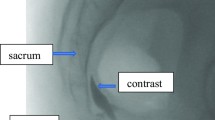
Plancarte R, et al. Superior hypogastric plexus block for pelvic cancer pain. Anesthesiology. 1990;73(2):236–9.
Turker G, et al. A new technique for superior hypogastric plexus block: the posteromedian transdiscal approach. Tohoku J Exp Med. 2005;206(3):277–81.
• Liliang PC, et al. Fluoroscopically-guided superior hypogastric plexus neurolysis using a single needle: a modified technique for a posterolateral transdiscal approach. Pain Phys. 2018;21(4):E341–5. Single needle approach for superior hypogastric plexus block.
Nagpal AS, Moody EL. Interventional management for pelvic pain. Phys Med Rehabil Clin N Am. 2017;28(3):621–46.
Erdine S, et al. Transdiscal approach for hypogastric plexus block. Reg Anesth Pain Med. 2003;28(4):304–8.
Kanazi GE, et al. New technique for superior hypogastric plexus block. Reg Anesth Pain Med. 1999;24(5):473–6.
Urits I, et al. Inferior hypogastric block for the treatment of chronic pelvic pain. Anesth Pain Med. 2021;11(1): e112225.
Choi HS, et al. A new technique for inferior hypogastric plexus block: a coccygeal transverse approach -a case report. Korean J Pain. 2012;25(1):38–42.
Khan YN, Raza SS, Khan EA. Application of spinal cord stimulation for the treatment of abdominal visceral pain syndromes: case reports. Neuromodulation. 2005;8(1):14–27.
Gupta D, et al. Ultrasonography reinvents the originally described technique for ganglion impar neurolysis in perianal cancer pain. Anesth Analg. 2008;107(4):1390–2.
Scott-Warren JT, Hill V, Rajasekaran A. Ganglion impar blockade: a review. Curr Pain Headache Rep. 2013;17(1):306.
Wemm K Jr, Saberski L. Modified approach to block the ganglion impar (ganglion of Walther). Reg Anesth. 1995;20(6):544–5.
Munir MA, Zhang J, Ahmad M. A modified needle-inside-needle technique for the ganglion impar block. Can J Anaesth. 2004;51(9):915–7.
Lin CS, et al. Ultrasound-guided ganglion impar block: a technical report. Pain Med. 2010;11(3):390–4.
Foye PM, et al. Successful injection for coccyx pain. Am J Phys Med Rehabil. 2006;85(9):783–4.
Hunter CW, Diwan S. Ganglion impar block, in Anesthesia Key. 2017.
Huang JJ. Another modified approach to the ganglion of Walther block (ganglion of impar). J Clin Anesth. 2003;15(4):282–3.
Foye PM. New approaches to ganglion impar blocks via coccygeal joints. Reg Anesth Pain Med. 2007;32(3):269.
Reig E, et al. Thermocoagulation of the ganglion impar or ganglion of Walther: description of a modified approach. Preliminary results in chronic, nononcological pain. Pain Pract. 2005;5(2):103–10.
Smith TJ, et al. Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol. 2002;20(19):4040–9.
Deer TR, et al. Comprehensive consensus based guidelines on intrathecal drug delivery systems in the treatment of pain caused by cancer pain. Pain Physician. 2011;14(3):E283-312.
Chaney MA. Side effects of intrathecal and epidural opioids. Can J Anaesth. 1995;42(10):891–903.
Bottros MM, Christo PJ. Current perspectives on intrathecal drug delivery. J Pain Res. 2014;7:615–26.
Deer TR. Polyanalgesic Consensus Conference 2012. Neuromodulation. 2012;15(5):418–9.
Upadhyay SP, Mallick PN. Intrathecal drug delivery system (IDDS) for cancer pain management: a review and updates. Am J Hosp Palliat Care. 2012;29(5):388–98.
Cohen SP, Dragovich A. Intrathecal analgesia. Anesthesiol Clin. 2007;25(4):863–82, viii.
Smyth CE, Jarvis V, Poulin P. Brief review: Neuraxial analgesia in refractory malignant pain. Can J Anaesth. 2014;61(2):141–53.
Falco FJ, et al. Intrathecal infusion systems for long-term management of chronic non-cancer pain: an update of assessment of evidence. Pain Phys. 2013;16(2 Suppl):SE185–216.
AM, D. Traitement des syndromes douloureux de la peripherie par l’alcoolisation sub-arachnoidienne. La Presse Méd. 1931;67:1249–1252.
Candido K, Stevens RA. Intrathecal neurolytic blocks for the relief of cancer pain. Best Pract Res Clin Anaesthesiol. 2003;17(3):407–28.
Korevaar WC. Transcatheter thoracic epidural neurolysis using ethyl alcohol. Anesthesiology. 1988;69(6):989–93.
Mehta M, Salmon N. Extradural block. Confirmation of the injection site by X-ray monitoring. Anaesthesia. 1985;40(10):1009–12.
Gerbershagen HU. Neurolysis. Subarachnoid neurolytic blockade Acta Anaesthesiol Belg. 1981;32(1):45–57.
Kapural L, et al. Spinal cord stimulation for chronic visceral abdominal pain. Pain Med. 2010;11(3):347–55.
Qin C, Farber JP, Foreman RD. Spinal cord stimulation modulates activity of lumbosacral spinal neurons receiving input from urinary bladder in rats. Neurosci Lett. 2007;428(1):38–42.
Steege JF. Superior hypogastric block during microlaparoscopic pain mapping. J Am Assoc Gynecol Laparosc. 1998;5(3):265–7.
Kapural L, et al. Technical aspects of spinal cord stimulation for managing chronic visceral abdominal pain: the results from the national survey. Pain Med. 2010;11(5):685–91.
Grabow TS, Tella PK, Raja SN. Spinal cord stimulation for complex regional pain syndrome: an evidence-based medicine review of the literature. Clin J Pain. 2003;19(6):371–83.
Taylor RS, et al. The cost effectiveness of spinal cord stimulation in the treatment of pain: a systematic review of the literature. J Pain Symptom Manage. 2004;27(4):370–8.
Baranidharan G, Simpson KH, Dhandapani K. Spinal cord stimulation for visceral pain--a novel approach. Neuromodulation. 2014;17(8):753–8; discussion 758.
• Hunter CW, Yang A. Dorsal root ganglion stimulation for chronic pelvic pain: a case series and technical report on a novel lead configuration. Neuromodulation. 2019;22:87–95. Dorsal root ganglion lead configuration.
• Patel K. Dorsal root ganglion stimulation for chronic pelvic pain. Obstetrics Gynecol. 2019;133 Suppl 1, 223. (2) Hunter CW, Yang A. Dorsal root ganglion stimulation for chronic pelvic pain: a case series and technical report on a novel lead configuration. Neuromodulation. 2019;22:87–95. Dorsal root ganglion stimulation for pelvic pain.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Christopher Wie, Shirin Ghanavatian, Scott Pew, Alexander Kim, Natalie Strand, John Freeman, Mostafa Maita, Stephen Covington, and Jillian Maloney declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Chronic Pain Medicine
Rights and permissions
About this article
Cite this article
Wie, C., Ghanavatian, S., Pew, S. et al. Interventional Treatment Modalities for Chronic Abdominal and Pelvic Visceral Pain. Curr Pain Headache Rep 26, 683–691 (2022). https://doi.org/10.1007/s11916-022-01072-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-022-01072-4