Abstract
Purpose of Review
Painful diabetic neuropathy (PDN) is a prevalent and debilitating condition, characterized by severe burning, tingling, and lancinating pain usually located in the distal lower extremities. In addition to manifesting with severe pain, PDN may also be associated with poor quality of life and sleep, mood disorders, burns, falls, and social withdrawal. The authors appraised the current body of literature for evidence on neuromodulation interventions for PDN.
Recent Findings
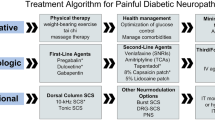
In patients with refractory PDN unresponsive to conventional medical management (glucose optimization and oral analgesic medications), there is level I evidence supporting the use of 10-kHz and tonic dorsal column spinal cord stimulation (SCS). Included studies reported significant associations between 10-kHz and tonic dorsal column SCS and superior analgesic outcomes, physical functioning, and patient satisfaction. Current level of evidence remains limited for other modalities of neuromodulation for PDN including burst SCS (level II-3), dorsal root ganglion SCS (level III), and peripheral nerve stimulation (level II-3). Some studies reported improvements in neurological physical examination, sensory testing, and/or reflex testing in patients undergoing 10-kHz SCS for treatment of PDN.
Summary
In summary, the purpose of this review is to equip provider with important updates on the use of neuromodulation interventions for the treatment of PDN that is refractory to conventional medical therapy, with current level I evidence supporting use of 10-kHz and tonic SCS for PDN.


Similar content being viewed by others
References
Kerner W, Brückel J, Association GD. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes. 2014;122(7):384–6. https://doi.org/10.1055/s-0034-1366278.
Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep. 2019;19(10):86. https://doi.org/10.1007/s11892-019-1212-8.
Pop-Busui R, Boulton AJ, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(1):136–54. https://doi.org/10.2337/dc16-2042.
Gorson KC, Schott C, Herman R, Ropper AH, Rand WM. Gabapentin in the treatment of painful diabetic neuropathy: a placebo controlled, double blind, crossover trial. J Neurol Neurosurg Psychiatry. 1999;66(2):251–2. https://doi.org/10.1136/jnnp.66.2.251.
Majdinasab N, Kaveyani H, Azizi M. A comparative double-blind randomized study on the effectiveness of duloxetine and gabapentin on painful diabetic peripheral polyneuropathy. Drug Des Devel Ther. 2019;13:1985–92. https://doi.org/10.2147/DDDT.S185995.
Blair HA. Capsaicin 8% dermal patch: a review in peripheral neuropathic pain. Drugs. 2018;78(14):1489–500. https://doi.org/10.1007/s40265-018-0982-7.
van Nooten F, Trundell D, Staniewska D, Chen J, Davies EW, Revicki DA. Evaluating the measurement properties of the self-assessment of treatment version II, follow-up version, in patients with painful diabetic peripheral neuropathy. Pain Res Treat. 2017;2017:6080648. https://doi.org/10.1155/2017/6080648.
Hagedorn JM, Pittelkow TP, Hunt CL, D’Souza RS, Lamer TJ. Current perspectives on spinal cord stimulation for the treatment of cancer pain. J Pain Res. 2020;13:3295–305. https://doi.org/10.2147/JPR.S263857.
Deer TR, Grider JS, Lamer TJ, et al. A systematic literature review of spine neurostimulation therapies for the treatment of pain. Pain Med. 2020;21(7):1421–32. https://doi.org/10.1093/pm/pnz353.
Klomp HM, Steyerberg EW, Habbema JD, van Urk H, Group ES. What is the evidence on efficacy of spinal cord stimulation in (subgroups of) patients with critical limb ischemia? Ann Vasc Surg. 2009;23(3):355–63. https://doi.org/10.1016/j.avsg.2008.08.016.
Page MJ, Shamseer L, Tricco AC. Registration of systematic reviews in PROSPERO: 30,000 records and counting. Syst Rev. 2018;7(1):32. https://doi.org/10.1186/s13643-018-0699-4.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1-34. https://doi.org/10.1016/j.jclinepi.2009.06.006.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Wells GA, Shea B, O'Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. The Ottawa Hospital Research Institute: Ottawa, Canada. 2013;1–4.
Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3 Suppl):21–35. https://doi.org/10.1016/s0749-3797(01)00261-6.
Abd-Elsayed A, Schiavoni N, Sachdeva H. Efficacy of spinal cord stimulators in treating peripheral neuropathy: a case series. J Clin Anesth. 2016;28:74–7. https://doi.org/10.1016/j.jclinane.2015.08.011.
Daousi C, Benbow SJ, MacFarlane IA. Electrical spinal cord stimulation in the long-term treatment of chronic painful diabetic neuropathy. Diabet Med. 2005;22(4):393–8. https://doi.org/10.1111/j.1464-5491.2004.01410.x.
de Vos CC, Bom MJ, Vanneste S, Lenders MW, de Ridder D. Burst spinal cord stimulation evaluated in patients with failed back surgery syndrome and painful diabetic neuropathy. Neuromodulation. 2014;17(2):152–9. https://doi.org/10.1111/ner.12116.
de Vos CC, Rajan V, Steenbergen W, van der Aa HE, Buschman HP. Effect and safety of spinal cord stimulation for treatment of chronic pain caused by diabetic neuropathy. J Diabetes Complications. 2009;23(1):40–5. https://doi.org/10.1016/j.jdiacomp.2007.08.002.
Duarte RV, Andronis L, Lenders MW, de Vos CC. Quality of life increases in patients with painful diabetic neuropathy following treatment with spinal cord stimulation. Qual Life Res. 2016;25(7):1771–7. https://doi.org/10.1007/s11136-015-1211-4.
Galan V, Scowcroft J, Chang P, et al. 10-kHz spinal cord stimulation treatment for painful diabetic neuropathy: results from. Pain Manag. 2020;10(5):291–300. https://doi.org/10.2217/pmt-2020-0033.
Kinfe TM, Pintea B. The usefulness of spinal cord stimulation for chronic pain due to combined vasospastic prinzmetal angina and diabetic neuropathic pain of the lower limbs. J Neurol Surg A Cent Eur Neurosurg. 2016;77(2):176–8. https://doi.org/10.1055/s-0034-1543960.
Petersen EA, Stauss TG, Scowcroft JA, et al. Effect of high-frequency (10-kHz) spinal cord stimulation in patients with painful diabetic neuropathy: a randomized clinical trial. JAMA Neurol. 2021;78(6):687–98. https://doi.org/10.1001/jamaneurol.2021.0538.
Pluijms WA, Slangen R, Bakkers M, et al. Pain relief and quality-of-life improvement after spinal cord stimulation in painful diabetic polyneuropathy: a pilot study. Br J Anaesth. 2012;109(4):623–9. https://doi.org/10.1093/bja/aes251.
Sills S. Treatment of painful polyneuropathies of diabetic and other origins with 10 kHz SCS: a case series. Postgrad Med. 2020;132(4):352–7. https://doi.org/10.1080/00325481.2020.1732065.
Slangen R, Schaper NC, Faber CG, et al. Spinal cord stimulation and pain relief in painful diabetic peripheral neuropathy: a prospective two-center randomized controlled trial. Diabetes Care. 2014;37(11):3016–24. https://doi.org/10.2337/dc14-0684.
Tesfaye S, Watt J, Benbow SJ, Pang KA, Miles J, MacFarlane IA. Electrical spinal-cord stimulation for painful diabetic peripheral neuropathy. Lancet. 1996;348(9043):1698–701. https://doi.org/10.1016/S0140-6736(96)02467-1.
van Beek M, Geurts JW, Slangen R, et al. Severity of neuropathy is associated with long-term spinal cord stimulation outcome in painful diabetic peripheral neuropathy: five-year follow-up of a prospective two-center clinical trial. Diabetes Care. 2018;41(1):32–8. https://doi.org/10.2337/dc17-0983.
de Vos CC, Meier K, Zaalberg PB, et al. Spinal cord stimulation in patients with painful diabetic neuropathy: a multicentre randomized clinical trial. Pain. 2014;155(11):2426–31. https://doi.org/10.1016/j.pain.2014.08.031.
Chapman KB, Van Roosendaal BW, Van Helmond N, Yousef TA. Unilateral dorsal root ganglion stimulation lead placement with resolution of bilateral lower extremity symptoms in diabetic peripheral neuropathy. Cureus. 2020;12(9):e10735. https://doi.org/10.7759/cureus.10735.
Eldabe S, Espinet A, Wahlstedt A, et al. Retrospective case series on the treatment of painful diabetic peripheral neuropathy with dorsal root ganglion stimulation. Neuromodulation. 2018;21(8):787–92. https://doi.org/10.1111/ner.12767.
Falowski S, Pope JE, Raza A. Early US experience with stimulation of the dorsal root ganglia for the treatment of peripheral neuropathy in the lower extremities: a multicenter retrospective case series. Neuromodulation. 2019;22(1):96–100. https://doi.org/10.1111/ner.12860.
Dabby R, Sadeh M, Goldberg I, Finkelshtein V. Electrical stimulation of the posterior tibial nerve reduces neuropathic pain in patients with polyneuropathy. J Pain Res. 2017;10:2717–23. https://doi.org/10.2147/JPR.S137420.
Sokal P, Harat M, Zieliński P, Kierońska S. Tibial nerve stimulation with a miniature, wireless stimulator in chronic peripheral neuropathic pain. J Pain Res. 2017;10:613–9. https://doi.org/10.2147/JPR.S128861.
Zeno A, Handler SJ, Jakus-Waldman S, Yazdany T, Nguyen JN. Percutaneous tibial nerve stimulation in diabetic and nondiabetic women with overactive bladder syndrome: a retrospective cohort study. Female Pelvic Med Reconstr Surg. 2021. https://doi.org/10.1097/SPV.0000000000001036.
D’Souza RS, Strand N. Neuromodulation with burst and tonic stimulation decreases opioid consumption: a post hoc analysis of the success using neuromodulation with BURST (SUNBURST) randomized controlled trial. Neuromodulation. 2021;24(1):135–41. https://doi.org/10.1111/ner.13273.
Staudt MD, Prabhala T, Sheldon BL, et al. Current strategies for the management of painful diabetic neuropathy. J Diabetes Sci Technol. 2020:1932296820951829. https://doi.org/10.1177/1932296820951829
Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Prescription of long-acting opioids and mortality in patients with chronic noncancer pain. JAMA. 2016;315(22):2415–23. https://doi.org/10.1001/jama.2016.7789.
D'Souza RS, Eldrige JS. Prescription drug monitoring program. StatPearls. StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC. 2020.
D’Souza RS, Hagedorn JM. Anticoagulation use during dorsal column spinal cord stimulation trial. Pain Med. 2020. https://doi.org/10.1093/pm/pnaa244.
Dombovy-Johnson ML, D'Souza RS, Thuc Ha C, Hagedorn JM. Incidence and risk factors for spinal cord stimulator lead migration with or without loss of efficacy: a retrospective review of 91 consecutive thoracic lead implants. Neuromodulation: Technology at the Neural Interface. n/a(n/a). https://doi.org/10.1111/ner.13487.
D'Souza RS, Hunt CL. A rare case of anchor fracture manifesting with new-onset neuropathic pain after spinal cord stimulator implantation. Neuromodulation. 2021. https://doi.org/10.1111/ner.13530.
D'Souza R, Olatoye O, Butler C, Barman R, Ashmore Z, Hagedorn J. Adverse events associated with 10-kHz dorsal column spinal cord stimulation: a five-year analysis of the manufacturer and user facility device experience (MAUDE) database. Clin J Pain. 2021;in press.
van Beek M, Hermes D, Honig WM, et al. Long-term spinal cord stimulation alleviates mechanical hypersensitivity and increases peripheral cutaneous blood perfusion in experimental painful diabetic polyneuropathy. Neuromodulation. 2018;21(5):472–9. https://doi.org/10.1111/ner.12757.
Mor A, Dekkers OM, Nielsen JS, Beck-Nielsen H, Sørensen HT, Thomsen RW. Impact of glycemic control on risk of infections in patients with type 2 diabetes: a population-based cohort study. Am J Epidemiol. 2017;186(2):227–36. https://doi.org/10.1093/aje/kwx049.
Martin ET, Kaye KS, Knott C, et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2016;37(1):88–99. https://doi.org/10.1017/ice.2015.249.
Cancienne JM, Werner BC, Browne JA. Is there an association between hemoglobin A1C and deep postoperative infection after TKA? Clin Orthop Relat Res. 2017;475(6):1642–9. https://doi.org/10.1007/s11999-017-5246-4.
Harris AH, Bowe TR, Gupta S, Ellerbe LS, Giori NJ. Hemoglobin A1C as a marker for surgical risk in diabetic patients undergoing total joint arthroplasty. J Arthroplasty. 2013;28(8 Suppl):25–9. https://doi.org/10.1016/j.arth.2013.03.033.
Cancienne JM, Werner BC, Chen DQ, Hassanzadeh H, Shimer AL. Perioperative hemoglobin A1c as a predictor of deep infection following single-level lumbar decompression in patients with diabetes. Spine J. 2017;17(8):1100–5. https://doi.org/10.1016/j.spinee.2017.03.017.
Iorio R, Williams KM, Marcantonio AJ, Specht LM, Tilzey JF, Healy WL. Diabetes mellitus, hemoglobin A1C, and the incidence of total joint arthroplasty infection. J Arthroplasty. 2012;27(5):726-9.e1. https://doi.org/10.1016/j.arth.2011.09.013.
Hagedorn JM, McArdle I, D’Souza RS, Yadav A, Engle AM, Deer TR. Effect of patient characteristics on clinical outcomes more than 12 months following dorsal root ganglion stimulation implantation: a retrospective review. Neuromodulation. 2021. https://doi.org/10.1111/ner.13326.
Skaribas IM, Peccora C, Skaribas E. Single S1 dorsal root ganglia stimulation for intractable complex regional pain syndrome foot pain after lumbar spine surgery: a case series. Neuromodulation. 2019;22(1):101–7. https://doi.org/10.1111/ner.12780.
Langford B, Mauck WD. Advancement in neuromodulation technology with the innovation of design-specific peripheral nerve stimulators: sural nerve stimulation for radiculopathy. Pain Med. 2020;21(6):1297–300. https://doi.org/10.1093/pm/pnaa077.
Strand NH, D’Souza R, Wie C, et al. Mechanism of action of peripheral nerve stimulation. Curr Pain Headache Rep. 2021;25(7):47. https://doi.org/10.1007/s11916-021-00962-3.
Langford B, Hooten WM, D’Souza S, Moeschler S, D’Souza RS. YouTube as a source of medical information about spinal cord stimulation. Neuromodulation. 2020. https://doi.org/10.1111/ner.13303.
Acknowledgements
We would like to thank Cynthia J. Beeler, M.L.S., AHIP for assisting with the formal search strategy utilized in this review paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuromodulation
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
D’Souza, R.S., Langford, B., Dombovy-Johnson, M. et al. Neuromodulation Interventions for the Treatment of Painful Diabetic Neuropathy: a Systematic Review. Curr Pain Headache Rep 26, 365–377 (2022). https://doi.org/10.1007/s11916-022-01035-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-022-01035-9