Abstract
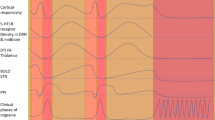
The exact pathophysiological mechanisms leading to the activation and sensitization of the trigeminovascular pathway, which in turns results in the migraine attack, are not completely elucidated. It is likely that direct activation by cortical spreading depression, together with dysfunctional central control of pain, plays a major role in the onset and spreading of the migraine attack. This review focuses on recent structural and functional neuroimaging studies that investigated the role of subcortical and cortical structures in modulating nociceptive input in migraine, which outlined the presence of an imbalance between inhibitory and excitatory modulation of pain processing in the disease.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Merikangas KR. Contributions of epidemiology to our understanding of migraine. Headache. 2013;53:230–46.
Hadjikhani N, Sanchez Del Rio M, Wu O, et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc Natl Acad Sci U S A. 2001;98:4687–92.
Lauritzen M, Dreier JP, Fabricius M, Hartings JA, Graf R, Strong AJ. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab : Off J Int Soc Cereb Blood Flow Metab. 2011;31:17–35.
Schwedt TJ, Goadsby PJ. 14th International Headache Congress: basic science highlights. Headache. 2010;50:520–6.
Bolay H, Reuter U, Dunn AK, Huang Z, Boas DA, Moskowitz MA. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nat Med. 2002;8:136–42.
Vincent MB, Hadjikhani N. Migraine aura and related phenomena: beyond scotomata and scintillations. Cephalalgia : Int J Headache. 2007;27:1368–77.
Vecchia D, Pietrobon D. Migraine: a disorder of brain excitatory-inhibitory balance? Trends Neurosci. 2012;35:507–20.
Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. 2011;12:570–84.
Weiller C, May A, Limmroth V, et al. Brain stem activation in spontaneous human migraine attacks. Nat Med. 1995;1:658–60.
Bahra A, Matharu MS, Buchel C, Frackowiak RS, Goadsby PJ. Brainstem activation specific to migraine headache. Lancet. 2001;357:1016–7.
Afridi SK, Giffin NJ, Kaube H, et al. A positron emission tomographic study in spontaneous migraine. Arch Neurol. 2005;62:1270–5.
Afridi SK, Matharu MS, Lee L, et al. A PET study exploring the laterality of brainstem activation in migraine using glyceryl trinitrate. Brain. 2005;128:932–9.
Naliboff BD, Berman S, Chang L, et al. Sex-related differences in IBS patients: central processing of visceral stimuli. Gastroenterology. 2003;124:1738–47.
Dunckley P, Wise RG, Fairhurst M, et al. A comparison of visceral and somatic pain processing in the human brainstem using functional magnetic resonance imaging. J Neurosci : Off J Soc Neurosci. 2005;25:7333–41.
Barman SM, Gebber GL, Kitchens H. Rostral dorsolateral pontine neurons with sympathetic nerve-related activity. Am J Physiol. 1999;276:H401–12.
Borsook D, Burstein R. The enigma of the dorsolateral pons as a migraine generator. Cephalalgia. 2012;32:803–12.
Moulton EA, Burstein R, Tully S, Hargreaves R, Becerra L, Borsook D. Interictal dysfunction of a brainstem descending modulatory center in migraine patients. PLoS One. 2008;3:e3799.
Wager TD, Scott DJ, Zubieta JK. Placebo effects on human mu-opioid activity during pain. Proc Natl Acad Sci U S A. 2007;104:11056–61.
Lai TH, Fuh JL, Lirng JF, Lin CP, Wang SJ. Brainstem 1H-MR spectroscopy in episodic and chronic migraine. J Headache Pain. 2012;13:645–51.
DaSilva AF, Granziera C, Snyder J, Hadjikhani N. Thickening in the somatosensory cortex of patients with migraine. Neurology. 2007;69:1990–5.
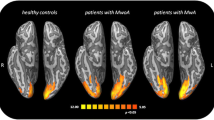
Granziera C, DaSilva AF, Snyder J, Tuch DS, Hadjikhani N. Anatomical alterations of the visual motion processing network in migraine with and without aura. PLoS Med. 2006;3:e402.
De Stefano N, Matthews PM, Narayanan S, Francis GS, Antel JP, Arnold DL. Axonal dysfunction and disability in a relapse of multiple sclerosis: longitudinal study of a patient. Neurology. 1997;49:1138–41.
Veloso F, Kumar K, Toth C. Headache secondary to deep brain implantation. Headache. 1998;38:507–15.
Rocca MA, Ceccarelli A, Falini A, et al. Brain gray matter changes in migraine patients with T2-visible lesions: a 3-T MRI study. Stroke; J Cereb Circ. 2006;37:1765–70.
DaSilva AF, Granziera C, Tuch DS, Snyder J, Vincent M, Hadjikhani N. Interictal alterations of the trigeminal somatosensory pathway and periaqueductal gray matter in migraine. Neuroreport. 2007;18:301–5.
Mainero C, Boshyan J, Hadjikhani N. Altered functional magnetic resonance imaging resting-state connectivity in periaqueductal gray networks in migraine. Ann Neurol. 2011;70:838–45.
Burstein R, Cutrer MF, Yarnitsky D. The development of cutaneous allodynia during a migraine attack clinical evidence for the sequential recruitment of spinal and supraspinal nociceptive neurons in migraine. Brain : J Neurol. 2000;123(Pt 8):1703–9.
Louter MA, Bosker JE, van Oosterhout WP, et al. Cutaneous allodynia as a predictor of migraine chronification. Brain : J Neurol. 2013. This longitudinal study demonstrates that cutaneous allodynia, a common feature accompanying migraine attacks and a clinical marker of central sensitization, is an independent predictor of migraine chronification. This finding has been interpreted to reflect functional and/or structural impairment at the level of brainstem pain modulatory networks, possibly consequent to repetitive activations of trigeminovascular neurons, in turn leading to repetitive activations of brainstem modulatory pathways.
Cliffer KD, Burstein R, Giesler Jr GJ. Distributions of spinothalamic, spinohypothalamic, and spinotelencephalic fibers revealed by anterograde transport of PHA-L in rats. J Neurosci. 1991;11:852–68.
Summ O, Charbit AR, Andreou AP, Goadsby PJ. Modulation of nocioceptive transmission with calcitonin gene-related peptide receptor antagonists in the thalamus. Brain. 2010;133:2540–8.
Burstein R, Jakubowski M, Garcia-Nicas E, et al. Thalamic sensitization transforms localized pain into widespread allodynia. Ann Neurol. 2010;68:81–91.
Schwedt TJ, Schlaggar BL, Mar S, et al. Atypical resting-state functional connectivity of affective pain regions in chronic migraine. Headache. 2013;53:737–51.
Granziera C, Daducci A, Romascano D, et al. Structural abnormalities in the thalamus of migraineurs with aura: A multiparametric study at 3 T. Hum Brain Mapp. 2013. This is a multiparametric MRI study that demonstrates broad microstructural alterations in the thalamus of MWA patients that may underlie abnormal cortical excitability control, leading to cortical spreading depression and visual aura.
Kruit MC, Launer LJ, Overbosch J, van Buchem MA, Ferrari MD. Iron accumulation in deep brain nuclei in migraine: a population-based magnetic resonance imaging study. Cephalalgia. 2009;29:351–9.
Alstadhaug KB. Migraine and the hypothalamus. Cephalalgia. 2009;29:809–17.
Carstens E. Hypothalamic inhibition of rat dorsal horn neuronal responses to noxious skin heating. Pain. 1986;25:95–107.
Bartsch T, Levy MJ, Knight YE, Goadsby PJ. Inhibition of nociceptive dural input in the trigeminal nucleus caudalis by somatostatin receptor blockade in the posterior hypothalamus. Pain. 2005;117:30–9.
Robert C, Bourgeais L, Arreto CD, et al. Paraventricular hypothalamic regulation of trigeminovascular mechanisms involved in headaches. J Neurosci. 2013;33:8827–40.
Kagan R, Kainz V, Burstein R, Noseda R. Hypothalamic and basal ganglia projections to the posterior thalamus: Possible role in modulation of migraine headache and photophobia. Neuroscience. 2013;248C:359–68.
Denuelle M, Fabre N, Payoux P, Chollet F, Geraud G. Hypothalamic activation in spontaneous migraine attacks. Headache. 2007;47:1418–26.
Shi CJ, Cassell MD. Cortical, thalamic, and amygdaloid connections of the anterior and posterior insular cortices. J Comp Neurol. 1998;399:440–68.
Stankewitz A, May A. Increased limbic and brainstem activity during migraine attacks following olfactory stimulation. Neurology. 2011;77:476–82.
Hadjikhani N, Ward N, Boshyan J, et al. The missing link: Enhanced functional connectivity between amygdala and visceroceptive cortex in migraine. Cephalalgia : Int J Headache. 2013;33:1264–8. Using rs-fMRI, Hadjikhani et al. demonstrated that functional connectivity is increased in the neurolimbic pain network of Mwa and MwoA but not in other chronic pain conditions. Cortical spreading depression may be driving hyperconnectivity of the amygdala in both types of migraine.
Akcali D, Sayin A, Sara Y, Bolay H. Does single cortical spreading depression elicit pain behaviour in freely moving rats? Cephalalgia : Int J Headache. 2010;30:1195–206.
Maizels M, Aurora S, Heinricher M. Beyond neurovascular: migraine as a dysfunctional neurolimbic pain network. Headache. 2012;52:1553–65.
Sato F, Akhter F, Haque T, et al. Projections from the insular cortex to pain-receptive trigeminal caudal subnucleus (medullary dorsal horn) and other lower brainstem areas in rats. Neuroscience. 2013;233:9–27.
May A. New insights into headache: an update on functional and structural imaging findings. Nat Rev Neurol. 2009;5:199–209.
Coppola G, Curra A, Di Lorenzo C, et al. Abnormal cortical responses to somatosensory stimulation in medication-overuse headache. BMC Neurol. 2010;10:126.
Chen WT, Lin YY, Fuh JL, Hamalainen MS, Ko YC, Wang SJ. Sustained visual cortex hyperexcitability in migraine with persistent visual aura. Brain : J Nneurol. 2011;134:2387–95.
Ozkul Y, Uckardes A. Median nerve somatosensory evoked potentials in migraine. Eur J Neurol : Off J Eur Fed Neurol Soc. 2002;9:227–32.
Schoenen J. Neurophysiological features of the migrainous brain. Neurol Sci : Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2006;27 Suppl 2:S77–81.
Boulloche N, Denuelle M, Payoux P, Fabre N, Trotter Y, Geraud G. Photophobia in migraine: an interictal PET study of cortical hyperexcitability and its modulation by pain. J Neurol Neurosurg Psychiatry. 2010;81:978–84.
Noseda R, Constandil L, Bourgeais L, Chalus M, Villanueva L. Changes of meningeal excitability mediated by corticotrigeminal networks: a link for the endogenous modulation of migraine pain. J Neurosci : Off J Soc Neurosci. 2010;30:14420–9.
Maleki N, Becerra L, Brawn J, Bigal M, Burstein R, Borsook D. Concurrent functional and structural cortical alterations in migraine. Cephalalgia : Int J Headache. 2012;32:607–20.
Lev R, Granovsky Y, Yarnitsky D. Enhanced pain expectation in migraine: EEG-based evidence for impaired prefrontal function. Headache. 2013;53:1054–70. This study shows that in both episodic MwA and MwoA, cortical dysexcitability, expressed as ineffective recruitment of prefrontal inhibitory pathways, may play a role in decreased habituation and enhanced anticipation and attention to pain and other external sensory stimuli.
Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron. 2007;55:377–91.
Breslau N, Andreski P. Migraine, personality, and psychiatric comorbidity. Headache. 1995;35:382–6.
Borsook D, Maleki N, Becerra L, McEwen B. Understanding migraine through the lens of maladaptive stress responses: a model disease of allostatic load. Neuron. 2012;73:219–34.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Dr. Caterina Mainero and Dr. Celine Louapre each declare no potential conflict of interest relevant to this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Mainero, C., Louapre, C. Migraine and Inhibitory System – I Can't Hold It!. Curr Pain Headache Rep 18, 426 (2014). https://doi.org/10.1007/s11916-014-0426-3
Published:
DOI: https://doi.org/10.1007/s11916-014-0426-3