Abstract
Purpose of Review
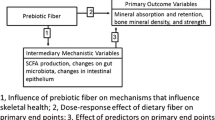
Osteoporosis is commonly diagnosed through the clinical assessment of bone quantity using bone mineral density; however, the primary clinical concern is bone fragility. Bone fragility is determined by both bone quantity and bone quality. Over the past decade, the gut microbiome has emerged as a factor that can regulate diseases throughout the body. This review discusses how microbial organisms and their genetic products that inhabit the gastrointestinal tract influence bone quantity, bone quality, and bone strength.
Recent Findings
Recent studies have shown that the gut microbiome regulates bone loss during estrogen depletion and glucocorticoid treatment. A series of studies has also shown that the gut microbiome influences whole bone strength by modifying bone tissue quality. The possible links between the gut microbiome and bone tissue quality are discussed focusing on the effects of microbiome-derived vitamin K.
Summary
We provide a brief introduction to the gut microbiome and how modifications to the gut microbiome may lead to changes in bone. The gut microbiome is a promising target for new therapeutic approaches that address bone quality in ways not possible with current interventions.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Hernandez CJ, van der Meulen MC. Understanding bone strength is not enough. J Bone Miner Res. 2017;32:1157–62 This review, intended for non-engineers, explains the effects of tissue material properties on whole bone strength.
• Knight R, Callewaert C, Marotz C, Hyde ER, Debelius JW, McDonald D, et al. The microbiome and human biology. Annu Rev Genom Hum Genet. 2017;18:65–86 This review motivates the need for further investigation into the microbiome in human health and disease.
Rajilić-Stojanović M, de Vos WM. The first 1000 cultured species of the human gastrointestinal microbiota. FEMS Microbiol Rev. 2014;38:996–1047.
Mimee M, Citorik RJ, Lu TK. Microbiome therapeutics — advances and challenges. Adv Drug Deliv Rev. 2016;105:44–54.
Faith JJ, Guruge JL, Charbonneau M, Subramanian S, Seedorf H, Goodman AL, et al. The Long-term stability of the human gut microbiota. Science. 2013;341:1237439.
Lozupone CA, Stombaugh J, Gonzalez A, Ackermann G, Wendel D, Vazquez-Baeza Y, et al. Meta-analyses of studies of the human microbiota. Genome Res. 2013;23:1704–14.
Thaiss CA, Elinav E. The remedy within: will the microbiome fulfill its therapeutic promise? J Mol Med. 2017;95:1021–7.
Einhorn TA. Bone strength: the bottom line. Calcif Tiss Int. 1992;51:331–9.
Järvinen TL, Sievänen H, Jokihaara J, Einhorn TA. Revival of bone strength: the bottom line. J Bone Miner Res. 2005;20:717–20.
Hernandez CJ, Guss JD, Luna M, Goldring SR. Links between the microbiome and bone. J Bone Miner Res. 2016;31:1638–46.
Pacifici R. Bone remodeling and the microbiome. Cold Spring Harb Perspect Med. 2018;8. https://doi.org/10.1101/cshperspect.a031203.
Yan J, Charles JF. Gut microbiome and bone: to build, destroy, or both? Curr Osteoporos Rep. 2017;15:376–84.
McCabe L, Britton RA, Parameswaran N. Prebiotic and probiotic regulation of bone health: role of the intestine and its microbiome. Curr Osteoporos Rep. 2015;13:363–71.
David LA, Materna AC, Friedman J, Campos-Baptista MI, Blackburn MC, Perrotta A, et al. Host lifestyle affects human microbiota on daily timescales. Genome Biol. 2014;15:R89.
Goodrich JK, Waters JL, Poole AC, Sutter JL, Koren O, Blekhman R, et al. Human genetics shape the gut microbiome. Cell. 2014;159:789–99.
Basu TK, Donaldson D. Intestinal absorption in health and disease: micronutrients. Best Pract Res Cl Ga. 2003;17:957–79.
Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. Human nutrition, the gut microbiome and the immune system. Nature. 2011;474:327–36.
Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–7.
Poundarik AA, Diab T, Sroga GE, Ural A, Boskey AL, Gundberg CM, et al. Dilatational band formation in bone. Proc Natl Acad Sci. 2012;109:19178–83.
Atkins GJ, Welldon KJ, Wijenayaka AR, Bonewald LF, Findlay DM. Vitamin K promotes mineralization, osteoblast-to-osteocyte transition, and an anticatabolic phenotype by γ-carboxylation-dependent and -independent mechanisms. Am J Physiol Cell Physiol. 2009;297:C1358–67.
Zaiss MM, Jones RM, Schett G, Pacifici R. The gut-bone axis: how bacterial metabolites bridge the distance. J Clin Invest. 2019;129:3018–28.
•• Tyagi AM, Yu M, Darby TM, et al. The microbial metabolite butyrate stimulates bone formation via T regulatory cell-mediated regulation of WNT10B expression. Immunity. 2018;49:1116-1131.e7 This study provides a link between the microbial metabolite butyrate and bone.
•• Guss JD, Taylor E, Rouse Z, Roubert S, Higgins CH, Thomas CJ, et al. The microbial metagenome and bone tissue composition in mice with microbiome-induced reductions in bone strength. Bone. 2019;127:146–54 This is the first paper to associate the functional capacity of the gut microbiome to bone phenotypes in mice.
Tsukasaki M, Takayanagi H. Osteoimmunology: evolving concepts in bone–immune interactions in health and disease. Nat Rev Immunol. 2019;19:626–42.
Li J-Y, Yu M, Pal S, Tyagi AM, Dar H, Adams J, et al. Parathyroid hormone–dependent bone formation requires butyrate production by intestinal microbiota. J Clin Invest. 2020;130:1767–81.
Yu M, Malik Tyagi A, Li J-Y, Adams J, Denning TL, Weitzmann MN, et al. PTH induces bone loss via microbial-dependent expansion of intestinal TNF+ T cells and Th17 cells. Nat Commun. 2020;11:468.
Vich Vila A, Collij V, Sanna S, Sinha T, Imhann F, Bourgonje AR, et al. Impact of commonly used drugs on the composition and metabolic function of the gut microbiota. Nat Commun. 2020;11:362.
Maier L, Pruteanu M, Kuhn M, Zeller G, Telzerow A, Anderson EE, et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature. 2018;555:623–8.
Yan J, Takakura A, Zandi-Nejad K, Charles JF. Mechanisms of gut microbiota-mediated bone remodeling. Gut Microbes. 2018;9:84–92.
Sjogren K, Engdahl C, Henning P, Lerner UH, Tremaroli V, Lagerquist MK, et al. The gut microbiota regulates bone mass in mice. J Bone Miner Res. 2012;27:1357–67.
Yan J, Herzog JW, Tsang K, Brennan CA, Bower MA, Garrett WS, et al. Gut microbiota induce IGF-1 and promote bone formation and growth. Proc Natl Acad Sci U S A. 2016;113:E7554–63.
Schepper JD, Collins F, Rios-Arce ND, Kang HJ, Schaefer L, Gardinier JD, et al. Involvement of the gut microbiota and barrier function in glucocorticoid-induced osteoporosis. J Bone Miner Res. 2020;35:801–20.
Rios-Arce ND, Schepper JD, Dagenais A, Schaefer L, Daly-Seiler CS, Gardinier JD, et al. Post-antibiotic gut dysbiosis-induced trabecular bone loss is dependent on lymphocytes. Bone. 2020;134:115269.
Schepper JD, Collins FL, Rios-Arce ND, Raehtz S, Schaefer L, Gardinier JD, et al. Probiotic Lactobacillus reuteri prevents postantibiotic bone loss by reducing intestinal dysbiosis and preventing barrier disruption. J Bone Miner Res. 2019;34:681–98.
Li J-Y, Chassaing B, Tyagi AM, Vaccaro C, Luo T, Adams J, et al. Sex steroid deficiency–associated bone loss is microbiota dependent and prevented by probiotics. J Clin Investig. 2016;126:2049–63.
Bilezikian JP. Primary hyperparathyroidism. J Clin Endocrinol Metab. 2018;103:3993–4004.
Iida-Klein A. Short-term continuous infusion of human parathyroid hormone 1-34 fragment is catabolic with decreased trabecular connectivity density accompanied by hypercalcemia in C57BL/J6 mice. J Endocrinol. 2005;186:549–57.
Ericsson AC, Franklin CL. Manipulating the gut microbiota: methods and challenges: figure 1. ILAR J. 2015;56:205–17.
•• Jansson P-A, Curiac D, Lazou Ahrén I, Hansson F, Martinsson Niskanen T, Sjögren K, et al. Probiotic treatment using a mix of three Lactobacillus strains for lumbar spine bone loss in postmenopausal women: a randomised, double-blind, placebo-controlled, multicentre trial. The Lancet Rheumatology. 2019;1:e154–62 This is the first randomized control trial in which daily that showed that probiotic dosing reduced postmenopausal bone loss. This reveals the potential to lead to a new generation of microbiome-based interventions for osteoporosis.
Cully M. Microbiome therapeutics go small molecule. Nat Rev Drug Discov. 2019;18:569–72.
Hernandez CJ, Keaveny TM. A biomechanical perspective on bone quality. Bone. 2006;39:1173–81.
Ionova-Martin SS, Do SH, Barth HD, Szadkowska M, Porter AE, Ager JW, et al. Reduced size-independent mechanical properties of cortical bone in high-fat diet-induced obesity. Bone. 2010;46:217–25.
Aslam MN, Jepsen KJ, Khoury B, Graf KH, Varani J. Bone structure and function in male C57BL/6 mice: effects of a high-fat Western-style diet with or without trace minerals. Bone Reports. 2016;5:141–9.
Creecy A, Uppuganti S, Merkel AR, O’Neal D, Makowski AJ, Granke M, et al. Changes in the fracture resistance of bone with the progression of type 2 diabetes in the ZDSD rat. Calcif Tissue Int. 2016;99:289–301.
Furst JR, Bandeira LC, Fan W-W, Agarwal S, Nishiyama KK, McMahon DJ, et al. advanced glycation endproducts and bone material strength in type 2 diabetes. J Clin Endocrinol Metab. 2016;101:2502–10.
Kim SM, Long J, Montez-Rath M, Leonard M, Chertow GM. Hip fracture in patients with non-dialysis-requiring chronic kidney disease. J Bone Miner Res. 2016;31:1803–9.
Matias PJ, Laranjinha I, Azevedo A, Raimundo A, Navarro D, Jorge C, et al. Bone fracture risk factors in prevalent hemodialysis patients. J Bone Miner Metab. 2020;38:205–12.
Ramezani A, Raj DS. The gut microbiome, kidney disease, and targeted interventions. JASN. 2014;25:657–70.
Ahmad A, Yang W, Chen G, Shafiq M, Javed S, Ali Zaidi SS, et al. Analysis of gut microbiota of obese individuals with type 2 diabetes and healthy individuals. PLoS One. 2019;14:e0226372.
Bishop N. Bone material properties in osteogenesis imperfecta. J Bone Miner Res. 2016;31:699–708.
Lafage MH, Balena R, Battle MA, Shea M, Seedor JG, Klein H, et al. Comparison of alendronate and sodium fluoride effects on cancellous and cortical bone in minipigs. A one-year study. J Clin Invest. 1995;95:2127–33.
Chachra D, Turner CH, Dunipace AJ, Grynpas MD. The effect of fluoride treatment on bone mineral in rabbits. Calcif Tissue Int. 1999;64:345–51.
Riggs L, Hodgson S, O’Fallen M, Chao E, Wahner H, Muhs J, et al. Effect of flouride treatment on the fracture rate in postmenopausal women with osteoporosis. N Engl J Med. 1990;322:802–9.
Gallant MA, Brown DM, Hammond M, Wallace JM, Du J, Deymier-Black AC, et al. Bone cell-independent benefits of raloxifene on the skeleton: a novel mechanism for improving bone material properties. Bone. 2014;61:191–200.
Powell KM, Brown AP, Skaggs CG, Pulliam AN, Berman AG, Deosthale P, et al. 6′-Methoxy Raloxifene-analog enhances mouse bone properties with reduced estrogen receptor binding. Bone Rep. 2020;12:100246.
Harris TB, Launer LJ, Eiriksdottir G, Kjartansson O, Jonsson PV, Sigurdsson G, et al. Age, gene/environment susceptibility-Reykjavik study: multidisciplinary applied Phenomics. Am J Epidemiol. 2007;165:1076–87.
Kopperdahl DL, Aspelund T, Hoffmann PF, Sigurdsson S, Siggeirsdottir K, Harris TB, et al. Assessment of incident spine and hip fractures in women and men using finite element analysis of CT scans. J Bone Miner Res. 2014;29:570–80.
Keaveny TM. Biomechanical computed tomography-noninvasive bone strength analysis using clinical computed tomography scans: BCT and bone strength. An NY Acad Sci. 2010;1192:57–65.
Nawathe S, Yang H, Fields AJ, Bouxsein ML, Keaveny TM. Theoretical effects of fully ductile versus fully brittle behaviors of bone tissue on the strength of the human proximal femur and vertebral body. J Biomech. 2015;48:1264–9.
• Guss JD, Horsfield MW, Fontenele FF, Sandoval TN, Luna M, Apoorva F, et al. Alterations to the gut microbiome impair bone strength and tissue material properties. J Bone Miner Res. 2017;32:1343–53 This is the first study to demonstrate an effect of the gut microbiome on bone strength.
Alliston T. Biological regulation of bone quality. Curr Osteoporos Rep. 2014;12:366–75.
Knapen MHJ, Schurgers LJ, Vermeer C. Vitamin K2 supplementation improves hip bone geometry and bone strength indices in postmenopausal women. Osteoporos Int. 2007;18:963–72.
Rønn SH, Harsløf T, Pedersen SB, Langdahl BL. Vitamin K2 (menaquinone-7) prevents age-related deterioration of trabecular bone microarchitecture at the tibia in postmenopausal women. Eur J Endocrinol. 2016;175:541–9.
Emaus N, Gjesdal CG, Almås B, Christensen M, Grimsgaard AS, Berntsen GKR, et al. Vitamin K2 supplementation does not influence bone loss in early menopausal women: a randomised double-blind placebo-controlled trial. Osteoporos Int. 2010;21:1731–40.
Division D, Mills J-O. Low-dose daily intake of vitamin K2 (Menaquinone-7) improves osteocalcin g-carboxylation: a double-blind, randomized controlled trials. J Nutr Sci Vitaminol. 61:471–80.
Nikel O, Poundarik AA, Bailey S, Vashishth D. Structural role of osteocalcin and osteopontin in energy dissipation in bone. J Biomech. 2018;80:45–52.
Ichikawa T, Horie-Inoue K, Ikeda K, Blumberg B, Inoue S. Steroid and xenobiotic receptor SXR mediates vitamin K 2 -activated transcription of extracellular matrix-related genes and collagen accumulation in osteoblastic cells. J Biol Chem. 2006;281:16927–34.
Jukes TH, Williams WL. Nutritional effects of antibiotics. Pharmacol Rev. 1953;5:381–420.
Rusoff LL, Fussell JM, Hyde CE, Crown RM, Gall LS. Parenteral administration of aureomycin to young calves with a note on mode of action. J Dairy Sci. 1954;37:488–97.
Ross E, Yacowitz H. Effect of penicillin on growth and bone ash of chicks fed different levels of vitamin-D and phosphorus. Poultry Sci. 1954;33:262–5.
Acknowledgments
Research reported in the article was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) under the National Institutes of Health award numbers R21AR068061, R21AR073454, and R21AR071534.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Biomechanics
Rights and permissions
About this article
Cite this article
Castaneda, M., Strong, J.M., Alabi, D.A. et al. The Gut Microbiome and Bone Strength. Curr Osteoporos Rep 18, 677–683 (2020). https://doi.org/10.1007/s11914-020-00627-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-020-00627-x