Abstract
Purposeof Review
Migraine is a chronic and disabling disease affecting a significant proportion of the world’s population. There is evidence that gastroparesis, a gastrointestinal (GI) dysmotility disorder in which transit of gastric contents is delayed, can occur in the setting of migraine. This article aims to review recent literature on overlap in the pathophysiology and clinical manifestations of migraine and gastroparesis and highlight management considerations when these disorders coexist.
Recent Findings
There has been increasing recognition of the importance of the connection between the GI tract and the brain, and mounting evidence for the overlap in the pathophysiology of migraine and gastroparesis specifically. There exists a complex interplay between the central, autonomic, and enteric nervous systems. Studies show that gastroparesis may be present during and between acute migraine attacks necessitating modification of management to optimize outcomes.
Summary
Gastric dysmotility in the setting of migraine can impact absorption of oral migraine medications and alternate formulations should be considered for some patients. Noninvasive vagus nerve stimulation has been FDA cleared for migraine treatment and is also being studied in gastroparesis. Dysfunction of the autonomic nervous system is a significant feature in the pathophysiology of gut motility and migraine, making treatments that modulate the vagus nerve attractive for future research.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •Of importance
• Aurora SK, Shrewsbury SB, Ray S, Hindiyeh N, Nguyen L. A link between gastrointestinal disorders and migraine: insights into the gut-brain connection. Headache. 2021;61:576–89. Excellent review on GI disorders in addition to gastroparesis that are associated with migraine.
Nguyen LA, Snape WJ. Clinical presentation and pathophysiology of gastroparesis. Gastroenterol Clin North Am. 2015;44:21–30.
Parkman HP. Migraine and gastroparesis from a gastroenterologist’s perspective. Headache. 2013;53(Suppl 1):4–10.
• Ye Y, Yin Y, Huh SY, Almansa C, Bennett D, Camilleri M. Epidemiology, etiology, and treatment of gastroparesis: real-world evidence from a large US national claims database. Gastroenterology. 2022;162:109-121.e5. Most recent study on the epidemiology of gastroparesis.
Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: updated age, sex, and socioeconomic-specific estimates from government health surveys. Headache. 2021;61:60–8.
Dodick DW. Migraine. Lancet. 2018;391:1315–30.
Yalcin H, Okuyucu EE, Ucar E, Duman T, Yilmazer S. Changes in liquid emptying in migraine patients: diagnosed with liquid phase gastric emptying scintigraphy. Intern Med J. 2012;42:455–9.
Volans GN. Migraine and drug absorption. Clin Pharmacokinet. 1978;3:313–8.
Aurora S, Kori S, Barrodale P, Nelsen A, McDonald S. Gastric stasis occurs in spontaneous, visually induced, and interictal migraine. Headache. 2007;47:1443–6.
Aurora SK, Kori SH, Barrodale P, McDonald SA, Haseley D. Gastric stasis in migraine: more than just a paroxysmal abnormality during a migraine attack. Headache. 2006;46:57–63.
Boyle R, Behan PO, Sutton JA. A correlation between severity of migraine and delayed gastric emptying measured by an epigastric impedance method. Br J Clin Pharmacol. 1990;30:405–9.
Yu YH, Jo Y, Jung JY, Kim BK, Seok JW. Gastric emptying in migraine: a comparison with functional dyspepsia. J Neurogastroenterol Motil. 2012;18:412–8.
Stanghellini V, Chan FKL, Hasler WL, Malagelada JR, Suzuki H, Tack J, Talley NJ. Gastroduodenal disorders. Gastroenterology. 2016;150:1380–92.
Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103:753–63.
Tougas G, Eaker EY, Abell TL, et al. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–62.
Jehangir A, Parkman HP. Role of gastric emptying in symptoms of gastroparesis. Gastrointestinal Disorders. 2019;1:391–402.
Guo JP, Maurer AH, Fisher RS, Parkman HP. Extending gastric emptying scintigraphy from two to four hours detects more patients with gastroparesis. Dig Dis Sci. 2001;46:24–9.
Sullivan A, Temperley L, Ruban A. Pathophysiology, aetiology and treatment of gastroparesis. Dig Dis Sci. 2020;65:1615–31.
Grover M, Farrugia G, Lurken MS, et al. Cellular changes in diabetic and idiopathic gastroparesis. Gastroenterology. 2011;140:1575-1585.e8.
Koch KL, Calles-Escandón J. Diabetic gastroparesis. Gastroenterol Clin North Am. 2015;44:39–57.
Pasricha PJ, Grover M, Yates KP, et al. Progress in gastroparesis – a narrative review of the work of the Gastroparesis Clinical Research Consortium. Clin Gastroenterol Hepatol. 2022;S1542-3565(22):00533–X.
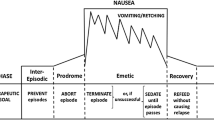
Dodick DW. A phase-by-phase review of migraine pathophysiology. Headache: J Head Face Pain. 2018;58:4–16.
Maniyar FH, Sprenger T, Schankin C, Goadsby PJ. The origin of nausea in migraine-a PET study. J Headache Pain. 2014;15:84.
Yuan CS, Barber WD. Area postrema: gastric vagal input from proximal stomach and interactions with nucleus tractus solitarius in cat. Brain Res Bull. 1993;30:119–25.
Boissonade FM, Sharkey KA, Davison JS. Fos expression in ferret dorsal vagal complex after peripheral emetic stimuli. Am J Physiol. 1994;266:R1118-1126.
Shapiro RE, Miselis RR. The central neural connections of the area postrema of the rat. J Comp Neurol. 1985;234:344–64.
Straube A, Ellrich J, Eren O, Blum B, Ruscheweyh R. Treatment of chronic migraine with transcutaneous stimulation of the auricular branch of the vagal nerve (auricular t-VNS): a randomized, monocentric clinical trial. J Headache Pain. 2015;16:63.
Akerman S, Simon B, Romero-Reyes M. Vagus nerve stimulation suppresses acute noxious activation of trigeminocervical neurons in animal models of primary headache. Neurobiol Dis. 2017;102:96–104.
Li N, Liu L, Sun M, Wang R, Jin W, Liu C, Hu Y. Predominant role of gut-vagus-brain neuronal pathway in postoperative nausea and vomiting: evidence from an observational cohort study. BMC Anesthesiol. 2021;21:234.
Beh SC. Noninvasive vagus nerve stimulation for nausea prevention during BPPV treatment. Neuromodulation. 2020;23:886–7.
Sj T, Am R, Fd S. Mechanisms of action of the 5-HT1B/1D receptor agonists. Arch Neurol. 2002;59(7):1084–8. https://doi.org/10.1001/archneur.59.7.1084.
Charbit AR, Akerman S, Goadsby PJ. Dopamine: what’s new in migraine? Curr Opin Neurol. 2010;23:275–81.
Ho TW, Edvinsson L, Goadsby PJ. CGRP and its receptors provide new insights into migraine pathophysiology. Nat Rev Neurol. 2010;6:573–82.
Holzer P, Farzi A. Neuropeptides and the microbiota-gut-brain axis. Adv Exp Med Biol. 2014;817:195–219.
Falkenberg K, Bjerg HR, Olesen J. Two-hour CGRP infusion causes gastrointestinal hyperactivity: possible relevance for CGRP antibody treatment. Headache. 2020;60:929–37.
Kaufman J, Levine I. Acute gastric dilatation of stomach during attack of migraine. Radiology. 1936;27:301–2.
(2016) 2nd Federation of Neurogastroenterology and Motility Meeting, 25–28 August 2016, Hyatt Regency San Francisco, San Francisco, California, USA. NeurogastroenterolMotil 28(1):5–108
Togha M, Martami F, Jafari E, Ariyanfar S, Hashemi SM. The prevalence and characteristics of visceral autonomic symptoms among migraineurs: a population-based study. Cephalalgia. 2022;42:500–9.
• Gottfried-Blackmore A, Adler EP, Fernandez-Becker N, Clarke J, Habtezion A, Nguyen L. Open-label pilot study: non-invasive vagal nerve stimulation improves symptoms and gastric emptying in patients with idiopathic gastroparesis. Neurogastroenterol Motil. 2020;32: e13769. Evidence for the use of non-invasive vagal nerve stimulation for the treatment of gastroparesis.
• Paulon E, Nastou D, Jaboli F, Marin J, Liebler E, Epstein O. Proof of concept: short-term non-invasive cervical vagus nerve stimulation in patients with drug-refractory gastroparesis. Frontline Gastroenterol. 2017;8:325–30. Evidence for the use of non-invasive vagal nerve stimulation for the treatment of gastroparesis.
Tassorelli C, Grazzi L, de Tommaso M, et al. Noninvasive vagus nerve stimulation as acute therapy for migraine: the randomized PRESTO study. Neurology. 2018;91:e364–73.
Lacy BE, Tack J, Gyawali CP. AGA clinical practice update on management of medically refractory gastroparesis: expert review. Clin Gastroenterol Hepatol. 2022;20:491–500.
Camilleri M, Chedid V, Ford AC, Haruma K, Horowitz M, Jones KL, Low PA, Park S-Y, Parkman HP, Stanghellini V. Gastroparesis. Nat Rev Dis Primers. 2018;4:41.
Liu N, Abell T. Gastroparesis updates on pathogenesis and management. Gut Liver. 2017;11:579–89.
Navari RM, Schwartzberg LS. Evolving role of neurokinin 1-receptor antagonists for chemotherapy-induced nausea and vomiting. Onco Targets Ther. 2018;11:6459–78.
Hasler WL, Wilson LA, Parkman HP, et al. Factors related to abdominal pain in gastroparesis: contrast to patients with predominant nausea and vomiting. Neurogastroenterol Motil. 2013;25(427–438):e300-301.
Abdelfatah MM, Noll A, Kapil N, et al. Long-term outcome of gastric per-oral endoscopic pyloromyotomy in treatment of gastroparesis. Clin Gastroenterol Hepatol. 2021;19:816–24.
Aurora SK, Papapetropoulos S, Kori SH, Kedar A, Abell TL. Gastric stasis in migraineurs: etiology, characteristics, and clinical and therapeutic implications. Cephalalgia. 2013;33:408–15.
Ferrari A, Tiraferri I, Neri L, Sternieri E. Why pharmacokinetic differences among oral triptans have little clinical importance: a comment. J Headache Pain. 2011;12:5–12.
Assadpour S, Shiran MR, Asadi P, Akhtari J, Sahebkar A. Harnessing intranasal delivery systems of sumatriptan for the treatment of migraine. Biomed Res Int. 2022;2022:3692065.
Tepper SJ, Johnstone MR. Breath-powered sumatriptan dry nasal powder: an intranasal medication delivery system for acute treatment of migraine. MDER. 2018;11:147–56.
Djupesland PG, Skretting A. Nasal deposition and clearance in man: comparison of a bidirectional powder device and a traditional liquid spray pump. J Aerosol Med Pulm Drug Deliv. 2012;25:280–9.
Lipton RB, McGinley JS, Shulman KJ, Silberstein SD, Wirth RJ, Buse DC. AVP-825 (sumatriptan nasal powder) reduces nausea compared to sumatriptan tablets: results of the COMPASS Randomized Clinical Trial. Headache. 2018;58:229–42.
Cameron C, Kelly S, Hsieh S-C, et al. Triptans in the acute treatment of migraine: a systematic review and network meta-analysis. Headache. 2015;55(Suppl 4):221–35.
Smith TR, Winner P, Aurora SK, Jeleva M, Hocevar-Trnka J, Shrewsbury SB. STOP 301: a phase 3, open-label study of safety, tolerability, and exploratory efficacy of INP104, Precision Olfactory Delivery (POD®) of dihydroergotamine mesylate, over 24/52 weeks in acute treatment of migraine attacks in adult patients. Headache. 2021;61:1214–26.
Albrecht D, Iwashima M, Dillon D, Harris S, Levy J. A phase 1, randomized, open-label, safety, tolerability, and comparative bioavailability study of intranasal dihydroergotamine powder (STS101), intramuscular dihydroergotamine mesylate, and intranasal DHE mesylate spray in healthy adult subjects. Headache. 2020;60:701–12.
Chou DE, Tso AR, Goadsby PJ. Aprepitant for the management of nausea with inpatient IV dihydroergotamine. Neurology. 2016;87:1613–6.
NURTEC® ODT (rimegepant) receives additional approval for preventive treatment for adult patients with episodic migraine. In: American Headache Society. https://americanheadachesociety.org/news/nurtec-odt-rimegepant-receives-additional-approval-for-preventive-treatment-for-adult-patients-with-episodic-migraine/. Accessed 25 Jul 2022
Moreno-Ajona D, Pérez-Rodríguez A, Goadsby PJ. Gepants, calcitonin-gene-related peptide receptor antagonists: what could be their role in migraine treatment? Curr Opin Neurol. 2020;33:309–15.
Singh-Franco D, Wolowich WR, De La Rosa D. Intranasal metoclopramide for acute and recurrent diabetic gastroparesis in adults. Drugs Ther Perspect. 2021;37:581–9.
VanderPluym JH, Halker Singh RB, Urtecho M, et al. Acute treatments for episodic migraine in adults: a systematic review and meta-analysis. JAMA. 2021;325:2357–69.
Eli Lilly and Company (2022) A phase 4 single-blind study of gastrointestinal transit time in adult patients with migraine before and after initiation of a mAb CGRP antagonist. clinicaltrials.gov
Escher CM, Paracka L, Dressler D, Kollewe K. Botulinum toxin in the management of chronic migraine: clinical evidence and experience. Ther Adv Neurol Disord. 2017;10:127–35.
Inan LE, Inan N, Unal-Artık HA, Atac C, Babaoglu G. Greater occipital nerve block in migraine prophylaxis: narrative review. Cephalalgia. 2019;39:908–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have existing conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Headache.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arca, K.N., Cai, J., Wang, F. et al. Migraine and Gastroparesis. Curr Neurol Neurosci Rep 22, 813–821 (2022). https://doi.org/10.1007/s11910-022-01241-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-022-01241-3