Abstract
Purpose of Review
Epilepsy associated with periventricular nodular heterotopia (PNH), a developmental malformation, is frequently drug-resistant and requires focal therapeutic intervention. Invasive EEG study is usually necessary to delineate the epileptogenic zone, but constructing an accurate hypothesis to define an appropriate electrode implantation scheme and the treatment is challenging. This article reviews recent studies that help understanding the epileptogenicity and potential therapeutic options in PNH.
Recent Findings
New noninvasive diagnostic and intracerebral EEG analytic tools demonstrated that cortical hyperexcitability and aberrant connectivity (between nodules and cortices and among nodules) are likely mechanisms causing epilepsy in most patients. The deeply seated PNH, if epileptogenic, are ideal target for stereotactic ablative techniques, which offer concomitant ablation of multiple regions with relatively satisfactory seizure outcome.
Summary
Advance in diagnostic and analytic tools have enhanced our understanding of the complex epileptogenicity in PNH. Development in stereotactic ablative techniques now offers promising therapeutic options for these patients.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Guerrini R, Barba C. Malformations of cortical development and aberrant cortical networks: epileptogenesis and functional organization. J Clin Neurophysiol. 2010;27(6):372–9. https://doi.org/10.1097/WNP.0b013e3181fe0585.
Barkovich AJ, Kuzniecky RI. Gray matter heterotopia. Neurology. 2000;55(11):1603–8.
Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns WB. A developmental and genetic classification for malformations of cortical development: update 2012. Brain. 2012;135(5):1348–69. https://doi.org/10.1093/brain/aws019.
Sheen VL, Dixon PH, Fox JW, Hong SE, Kinton L, Sisodiya SM, et al. Mutations in the X-linked filamin 1 gene cause periventricular nodular heterotopia in males as well as in females. Hum Mol Genet. 2001;10(17):1775–83. https://doi.org/10.1093/hmg/10.17.1775.
Mandelstam SA, Leventer RJ, Sandow A, McGillivray G, van Kogelenberg M, Guerrini R, et al. Bilateral posterior periventricular nodular heterotopia: a recognizable cortical malformation with a spectrum of associated brain abnormalities. AJNR Am J Neuroradiol. 2013;34(2):432–8. https://doi.org/10.3174/ajnr.A3427.
Parrini E. Periventricular heterotopia: phenotypic heterogeneity and correlation with filamin A mutations. Brain. 2006;129(7):1892–906. https://doi.org/10.1093/brain/awl125.
Meroni A, Galli C, Bramerio M, Tassi L, Colombo N, Cossu M, et al. Nodular heterotopia: a neuropathological study of 24 patients undergoing surgery for drug-resistant epilepsy. Epilepsia. 2009;50(1):116–24. https://doi.org/10.1111/j.1528-1167.2008.01717.x.
Dubeau F, Tampieri D, Lee N, Andermann E, Carpenter S, Leblanc R, et al. Periventricular and subcortical nodular heterotopia. A study of 33 patients. Brain. 1995;118(Pt 5):1273–87.
Tassi L, Colombo N, Cossu M, Mai R, Francione S, Lo Russo G, et al. Electroclinical, MRI and neuropathological study of 10 patients with nodular heterotopia, with surgical outcomes. Brain. 2005;128(Pt 2):321–37. https://doi.org/10.1093/brain/awh357.
Valton L, Guye M, McGonigal A, Marquis P, Wendling F, Regis J, et al. Functional interactions in brain networks underlying epileptic seizures in bilateral diffuse periventricular heterotopia. Clin Neurophysiol. 2008;119(1):212–23. https://doi.org/10.1016/j.clinph.2007.09.118.
Aghakhani Y, Kinay D, Gotman J, Soualmi L, Andermann F, Olivier A, et al. The role of periventricular nodular heterotopia in epileptogenesis. Brain. 2005;128(Pt 3):641–51. https://doi.org/10.1093/brain/awh388.
Cossu M, Fuschillo D, Cardinale F, Castana L, Francione S, Nobili L, et al. Stereo-EEG-guided radio-frequency thermocoagulations of epileptogenic grey-matter nodular heterotopy. J Neurol Neurosurg Psychiatry. 2014;85(6):611–7. https://doi.org/10.1136/jnnp-2013-305514.
Mirandola L, Mai RF, Francione S, Pelliccia V, Gozzo F, Sartori I, et al. Stereo-EEG: diagnostic and therapeutic tool for periventricular nodular heterotopia epilepsies. Epilepsia. 2017;58(11):1962–71. https://doi.org/10.1111/epi.13895This study reports the details of intracerebral EEG analysis and the outcome of different focal therapeutic interventions including radiofrequency-thermocoagulation in a large group of patients with PNH.
Christodoulou JA, Barnard ME, Del Tufo SN, Katzir T, Whitfield-Gabrieli S, Gabrieli JDE, et al. Integration of gray matter nodules into functional cortical circuits in periventricular heterotopia. Epilepsy Behav. 2013;29(2):400–6. https://doi.org/10.1016/j.yebeh.2013.08.028.
Liu W, An D, Tong X, Niu R, Gong Q, Zhou D. Region-specific connectivity in patients with periventricular nodular heterotopia and epilepsy: a study combining diffusion tensor imaging and functional MRI. Epilepsy Res. 2017;136:137–42. https://doi.org/10.1016/j.eplepsyres.2017.08.007.
Shafi MM, Vernet M, Klooster D, Chu CJ, Boric K, Barnard ME, et al. Physiological consequences of abnormal connectivity in a developmental epilepsy. Ann Neurol. 2015;77(3):487–503. https://doi.org/10.1002/ana.24343.
Khoo HM, von Ellenrieder N, Zazubovits N, Hall JA, Dubeau F, Gotman J. Internodular functional connectivity in heterotopia-related epilepsy. Ann Clin Transl Neurol. 2019;6(6):1010–23. https://doi.org/10.1002/acn3.769This study reports the role of functional connectivity between heterotopic nodules in epileptogenicity in a large group of patients with PNH.
Pizzo F, Roehri N, Catenoix H, Medina S, McGonigal A, Giusiano B, et al. Epileptogenic networks in nodular heterotopia: a stereoelectroencephalography study. Epilepsia. 2017;58(12):2112–23. https://doi.org/10.1111/epi.13919This study reports the role of aberrant connections between heterotopic nodules and the cortices in epileptogenicity and the outcome of focal therapeutic interventions in a large group of patients with PNH.
Wagner J, Elger CE, Urbach H, Bien CG. Electric stimulation of periventricular heterotopia: participation in higher cerebral functions. Epilepsy Behav. 2009;14(2):425–8. https://doi.org/10.1016/j.yebeh.2008.11.006.
Battaglia G, Franceschetti S, Chiapparini L, Freri E, Bassanini S, Giavazzi A, et al. Electroencephalographic recordings of focal seizures in patients affected by periventricular nodular heterotopia: role of the heterotopic nodules in the genesis of epileptic discharges. J Child Neurol. 2005;20(4):369–77. https://doi.org/10.1177/08830738050200041701.
Li LM, Dubeau F, Andermann F, Fish DR, Watson C, Cascino GD, et al. Periventricular nodular heterotopia and intractable temporal lobe epilepsy: poor outcome after temporal lobe resection. Ann Neurol. 1997;41(5):662–8. https://doi.org/10.1002/ana.410410516.
Kothare SV, VanLandingham K, Armon C, Luther JS, Friedman A, Radtke RA. Seizure onset from periventricular nodular heterotopias: depth-electrode study. Neurology. 1998;51(6):1723–7.
Battaglia G, Chiapparini L, Franceschetti S, Freri E, Tassi L, Bassanini S, et al. Periventricular nodular heterotopia: classification, epileptic history, and genesis of epileptic discharges. Epilepsia. 2006;47(1):86–97. https://doi.org/10.1111/j.1528-1167.2006.00374.x.
Agari T, Mihara T, Baba K, Kobayashi K, Usui N, Terada K, et al. Successful treatment of epilepsy by resection of periventricular nodular heterotopia. Acta Med Okayama. 2012;66(6):487–92. https://doi.org/10.18926/AMO/49045.
Carney PW, Masterton RA, Gill D, Jackson GD. Nodular heterotopia and absence seizures: fMRI evidence that they may be connected. Epilepsy Res. 2013;106(3):451–5. https://doi.org/10.1016/j.eplepsyres.2013.07.005.
De Wit MCY, Schippers HM, De Coo IFM, Arts WFM, Lequin MH, Brooks A, et al. Absence epilepsy and periventricular nodular heterotopia. Seizure. 2010;19(7):450–2. https://doi.org/10.1016/j.seizure.2010.06.013.
Stefan H, Nimsky C, Scheler G, Rampp S, Hopfengartner R, Hammen T, et al. Periventricular nodular heterotopia: a challenge for epilepsy surgery. Seizure. 2007;16(1):81–6. https://doi.org/10.1016/j.seizure.2006.10.004.
Merlet I. Dipole modeling of interictal and ictal EEG and MEG paroxysms. Epileptic Disord. 2002;3(3):11–36
Ramachandrannair R, Ochi A, Imai K, Benifla M, Akiyama T, Holowka S, et al. Epileptic spasms in older pediatric patients: MEG and ictal high-frequency oscillations suggest focal-onset seizures in a subset of epileptic spasms. Epilepsy Res. 2008;78(2–3):216–24. https://doi.org/10.1016/j.eplepsyres.2007.12.007.
Megevand P, Spinelli L, Genetti M, Brodbeck V, Momjian S, Schaller K, et al. Electric source imaging of interictal activity accurately localises the seizure onset zone. J Neurol Neurosurg Psychiatry. 2014;85(1):38–43. https://doi.org/10.1136/jnnp-2013-305515.
Khoo HM, von Ellenrieder N, Zazubovits N, Dubeau F, Gotman J. Epileptic networks in action: synchrony between distant hemodynamic responses. Ann Neurol. 2017;82(1):57–66. https://doi.org/10.1002/ana.24973.
Friston KJ, Holmes AP, Poline JB, Grasby PJ, Williams SC, Frackowiak RS, et al. Analysis of fMRI time-series revisited. Neuroimage. 1995;2(1):45–53. https://doi.org/10.1006/nimg.1995.1007.
Bagshaw AP, Aghakhani Y, Benar CG, Kobayashi E, Hawco C, Dubeau F, et al. EEG-fMRI of focal epileptic spikes: analysis with multiple haemodynamic functions and comparison with gadolinium-enhanced MR angiograms. Hum Brain Mapp. 2004;22(3):179–92. https://doi.org/10.1002/hbm.20024.
Khoo HM, von Ellenrieder N, Zazubovits N, He D, Dubeau F, Gotman J. The spike onset zone: the region where epileptic spikes start and from where they propagate. Neurology. 2018;91(7):e666–e74. https://doi.org/10.1212/WNL.0000000000005998.
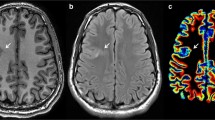
Kobayashi E, Bagshaw AP, Grova C, Gotman J, Dubeau F. Grey matter heterotopia: what EEG-fMRI can tell us about epileptogenicity of neuronal migration disorders. Brain. 2006;129(Pt 2):366–74. https://doi.org/10.1093/brain/awh710.
Kobayashi E, Hawco CS, Grova C, Dubeau F, Gotman J. Widespread and intense BOLD changes during brief focal electrographic seizures. Neurology. 2006;66(7):1049–55. https://doi.org/10.1212/01.wnl.0000204232.37720.a4.
Tyvaert L, Hawco C, Kobayashi E, LeVan P, Dubeau F, Gotman J. Different structures involved during ictal and interictal epileptic activity in malformations of cortical development: an EEG-fMRI study. Brain. 2008;131(Pt 8):2042–60. https://doi.org/10.1093/brain/awn145.
Christodoulou JA, Walker LM, Del Tufo SN, Katzir T, Gabrieli JD, Whitfield-Gabrieli S, et al. Abnormal structural and functional brain connectivity in gray matter heterotopia. Epilepsia. 2012;53(6):1024–32. https://doi.org/10.1111/j.1528-1167.2012.03466.x.
Archer JS, Abbott DF, Masterton RA, Palmer SM, Jackson GD. Functional MRI interactions between dysplastic nodules and overlying cortex in periventricular nodular heterotopia. Epilepsy Behav. 2010;19(4):631–4. https://doi.org/10.1016/j.yebeh.2010.09.018.
Abou-Khalil BW, Siegel GJ, Sackellares JC, Gilman S, Hichwa R, Marshall R. Positron emission tomography studies of cerebral glucose metabolism in chronic partial epilepsy. Ann Neurol. 1987;22(4):480–6. https://doi.org/10.1002/ana.410220407.
Seniaray N, Jain A. PET MRI coregistration in intractable epilepsy and gray matter heterotopia. Clin Nucl Med. 2017;42(3):e171–e2. https://doi.org/10.1097/rlu.0000000000001506.
Conrad GR, Sinha P. FDG PET imaging of subependymal gray matter heterotopia. Clin Nucl Med. 2005;30(1):35–6. https://doi.org/10.1097/00003072-200501000-00012.
Morioka T, Nishio S, Sasaki M, Yoshida T, Kuwabara Y, Ohta M, et al. Functional imaging in periventricular nodular heterotopia with the use of FDG-PET and HMPAO-SPECT. Neurosurg Rev. 1999;22(1):41–4. https://doi.org/10.1007/s101430050007.
Calabria FF, Cascini GL, Gambardella A, Labate A, Cherubini A, Gullà D, et al. Ictal 18F-FDG PET/MRI in a patient with cortical heterotopia and focal epilepsy. Clin Nucl Med. 2017;42(10):768–9. https://doi.org/10.1097/rlu.0000000000001797.
Popescu CE, Mai R, Sara R, Lizio D, Zanni D, Rossetti C, et al. The role of FDG-PET in patients with epilepsy related to periventricular nodular heterotopias: diagnostic features and long-term outcome. J Neuroimaging. 2019;29(4):512–20. https://doi.org/10.1111/jon.12620This study reports the findings of FDG-PET in a large group of patients and the relationship between the findings and the outcome following destruction of the PNH.
Perucca P, Dubeau F, Gotman J. Intracranial electroencephalographic seizure-onset patterns: effect of underlying pathology. Brain. 2014;137:183–96. https://doi.org/10.1093/brain/awt299.
Catenoix H, Mauguiere F, Montavont A, Ryvlin P, Guenot M, Isnard J. Seizures outcome after stereoelectroencephalography-guided thermocoagulations in malformations of cortical development poorly accessible to surgical resection. Neurosurgery. 2015;77(1):9–14; discussion −5. https://doi.org/10.1227/NEU.0000000000000723.
Cuello Oderiz C, von Ellenrieder N, Dubeau F, Eisenberg A, Gotman J, Hall J, et al. Association of cortical stimulation-induced seizure with surgical outcome in patients with focal drug-resistant epilepsy. JAMA Neurol. 2019;76(9):1070–8. https://doi.org/10.1001/jamaneurol.2019.1464.
Scherer C, Schuele S, Minotti L, Chabardes S, Hoffmann D, Kahane P. Intrinsic epileptogenicity of an isolated periventricular nodular heterotopia. Neurology. 2005;65(3):495–6. https://doi.org/10.1212/01.wnl.0000172350.25380.c7.
Cossu M, Fuschillo D, Casaceli G, Pelliccia V, Castana L, Mai R, et al. Stereoelectroencephalography-guided radiofrequency thermocoagulation in the epileptogenic zone: a retrospective study on 89 cases. J Neurosurg. 2015;123(6):1358–67. https://doi.org/10.3171/2014.12.JNS141968.
Bourdillon P, Cucherat M, Isnard J, Ostrowsky-Coste K, Catenoix H, Guenot M, et al. Stereo-electroencephalography-guided radiofrequency thermocoagulation in patients with focal epilepsy: a systematic review and meta-analysis. Epilepsia. 2018;59(12):2296–304. https://doi.org/10.1111/epi.14584This is a meta-analysis reporting the outcome of stereo-EEG guided radiofrequency-thermocoagulation, which pointed out that this technique is most beneficial in patients with PNH.
Dimova P, de Palma L, Job-Chapron AS, Minotti L, Hoffmann D, Kahane P. Radiofrequency thermocoagulation of the seizure-onset zone during stereoelectroencephalography. Epilepsia. 2017;58(3):381–92. https://doi.org/10.1111/epi.13663.
Whiting AC, Bingaman JR, Catapano JS, Whiting BB, Godzik J, Walker CT, et al. Laser interstitial thermal therapy for epileptogenic periventricular nodular heterotopia. World Neurosurg. 2020;138:e892–e7. https://doi.org/10.1016/j.wneu.2020.03.133.
Esquenazi Y, Kalamangalam GP, Slater JD, Knowlton RC, Friedman E, Morris SA, et al. Stereotactic laser ablation of epileptogenic periventricular nodular heterotopia. Epilepsy Res. 2014;108(3):547–54. https://doi.org/10.1016/j.eplepsyres.2014.01.009This is one of the index case reports revealing the potential of stereotactic laser ablation in treating epileptogenic PNH with details of patients.
Fayed I, Sacino MF, Gaillard WD, Keating RF, Oluigbo CO. MR-guided laser interstitial thermal therapy for medically refractory lesional epilepsy in pediatric patients: experience and outcomes. Pediatr Neurosurg. 2018;53(5):322–9. https://doi.org/10.1159/000491823.
Nagae LM, Honce JM, Nyberg E, Ojemann S, Abosch A, Drees CN. Imaging of laser therapy in epilepsy. J Neuroimaging. 2017;27(3):292–9. https://doi.org/10.1111/jon.12438.
Gonzalez-Martinez J, Vadera S, Mullin J, Enatsu R, Alexopoulos AV, Patwardhan R, et al. Robot-assisted stereotactic laser ablation in medically intractable epilepsy: operative technique. Neurosurgery. 2014;10(Suppl 2):167–72; discussion 72-3. https://doi.org/10.1227/NEU.0000000000000286.
Clarke DF, Tindall K, Lee M, Patel B. Bilateral occipital dysplasia, seizure identification, and ablation: a novel surgical technique. Epileptic Disord. 2014;16(2):238–43. https://doi.org/10.1684/epd.2014.0658.
Morris SA, Rollo M, Rollo P, Johnson J, Grant GA, Friedman E, et al. Prolonged blood-brain barrier disruption following laser interstitial ablation in epilepsy: a case series with a case report of postablation optic neuritis. World Neurosurg. 2017;104:467–75. https://doi.org/10.1016/j.wneu.2017.05.009.
Brown MG, Drees C, Nagae LM, Thompson JA, Ojemann S, Abosch A. Curative and palliative MRI-guided laser ablation for drug-resistant epilepsy. J Neurol Neurosurg Psychiatry. 2018;89(4):425–33. https://doi.org/10.1136/jnnp-2017-316003.
Barber SM, Tomycz L, George T, Clarke DF, Lee M. Delayed intraparenchymal and intraventricular hemorrhage requiring surgical evacuation after MRI-guided laser interstitial thermal therapy for lesional epilepsy. Stereotact Funct Neurosurg. 2017;95(2):73–8. https://doi.org/10.1159/000453280This case report revealed an important pitfall of stereotactic laser ablation in treating patients with epileptogenic PNH.
Cvetkovska E, Martins WA, Gonzalez-Martinez J, Taylor K, Li J, Grinenko O, et al. Heterotopia or overlaying cortex: what about in-between? Epilepsy Behav Case Rep. 2019;11:4–9. https://doi.org/10.1016/j.ebcr.2018.09.007.
Thompson SA, Kalamangalam GP, Tandon N. Intracranial evaluation and laser ablation for epilepsy with periventricular nodular heterotopia. Seizure. 2016;41:211–6. https://doi.org/10.1016/j.seizure.2016.06.019.
Wu C, Sperling MR, Falowski SM, Chitale AV, Werner-Wasik M, Evans JJ, et al. Radiosurgery for the treatment of dominant hemisphere periventricular heterotopia and intractable epilepsy in a series of three patients. Epilepsy Behav Case Rep. 2013;1:1–6. https://doi.org/10.1016/j.ebcr.2012.10.004.
Fountain N, Tseng P, Quigg M, Dallapiazza R, Elias J. Potential of focused ultrasound in epilepsy surgery. Journal of Therapeutic Ultrasound. 2015;3(S1):O29. https://doi.org/10.1186/2050-5736-3-s1-o29.
Schwab RS, Sweet WH, Mark VH, Kjellberg RN, Ervin FR. Treatment of intractable temporal lobe epilepsy by stereotactic amygdala lesions. Trans Am Neurol Assoc. 1965;90:12–9.
Cossu M, Mirandola L, Tassi L. RF-ablation in periventricular heterotopia-related epilepsy. Epilepsy Res. 2018;142:121–5. https://doi.org/10.1016/j.eplepsyres.2017.07.001.
Bourdillon P, Isnard J, Catenoix H, Montavont A, Rheims S, Ryvlin P, et al. Stereo electroencephalography-guided radiofrequency thermocoagulation (SEEG-guided RF-TC) in drug-resistant focal epilepsy: results from a 10-year experience. Epilepsia. 2017;58(1):85–93. https://doi.org/10.1111/epi.13616.
Bourdillon P, Rheims S, Catenoix H, Montavont A, Ostrowsky-Coste K, Isnard J, et al. Surgical techniques: stereoelectroencephalography-guided radiofrequency-thermocoagulation (SEEG-guided RF-TC). Seizure. 2020;77:64–8. https://doi.org/10.1016/j.seizure.2019.01.021.
Voges J, Buntjen L, Schmitt FC. Radiofrequency-thermoablation: general principle, historical overview and modern applications for epilepsy. Epilepsy Res. 2018;142:113–6. https://doi.org/10.1016/j.eplepsyres.2018.03.007.
Schmitt FC, Voges J, Buentjen L, Woermann F, Pannek HW, Skalej M, et al. Radiofrequency lesioning for epileptogenic periventricular nodular heterotopia: a rational approach. Epilepsia. 2011;52(9):e101–5. https://doi.org/10.1111/j.1528-1167.2011.03116.x.
Cardinale F, Cossu M, Castana L, Casaceli G, Schiariti MP, Miserocchi A, et al. Stereoelectroencephalography: surgical methodology, safety, and stereotactic application accuracy in 500 procedures. Neurosurgery. 2013;72(3):353–66; discussion 66. https://doi.org/10.1227/NEU.0b013e31827d1161.
Wellmer J, Parpaley Y, Rampp S, Popkirov S, Kugel H, Aydin U, et al. Lesion guided stereotactic radiofrequency thermocoagulation for palliative, in selected cases curative epilepsy surgery. Epilepsy Res. 2016;121:39–46. https://doi.org/10.1016/j.eplepsyres.2016.01.005.
Bourdillon P, Devaux B, Job-Chapron AS, Isnard J. SEEG-guided radiofrequency thermocoagulation. Neurophysiol Clin. 2018;48(1):59–64. https://doi.org/10.1016/j.neucli.2017.11.011.
Catenoix H, Mauguiere F, Guenot M, Ryvlin P, Bissery A, Sindou M, et al. SEEG-guided thermocoagulations: a palliative treatment of nonoperable partial epilepsies. Neurology. 2008;71(21):1719–26. https://doi.org/10.1212/01.wnl.0000335166.20451.88.
Scholly J, Pizzo F, Timofeev A, Valenti-Hirsch MP, Ollivier I, Proust F, et al. High-frequency oscillations and spikes running down after SEEG-guided thermocoagulations in the epileptogenic network of periventricular nodular heterotopia. Epilepsy Res. 2019;150:27–31. https://doi.org/10.1016/j.eplepsyres.2018.12.006.
Rosomoff HL, Carroll F. Reaction of neoplasm and brain to laser. Arch Neurol. 1966;14(2):143–8. https://doi.org/10.1001/archneur.1966.00470080027004.
Curry DJ, Gowda A, McNichols RJ, Wilfong AA. MR-guided stereotactic laser ablation of epileptogenic foci in children. Epilepsy Behav. 2012;24(4):408–14. https://doi.org/10.1016/j.yebeh.2012.04.135.
Hoppe C, Witt JA, Helmstaedter C, Gasser T, Vatter H, Elger CE. Laser interstitial thermotherapy (LiTT) in epilepsy surgery. Seizure. 2017;48:45–52. https://doi.org/10.1016/j.seizure.2017.04.002.
Lagman C, Chung LK, Pelargos PE, Ung N, Bui TT, Lee SJ, et al. Laser neurosurgery: a systematic analysis of magnetic resonance-guided laser interstitial thermal therapies. J Clin Neurosci. 2017;36:20–6. https://doi.org/10.1016/j.jocn.2016.10.019.
Youngerman BE, Save AV, McKhann GM. Magnetic resonance imaging-guided laser interstitial thermal therapy for epilepsy: systematic review of technique, indications, and outcomes. Neurosurgery. 2020;86(4):E366–E82. https://doi.org/10.1093/neuros/nyz556.
Krishna V, Sammartino F, Rezai A. A review of the current therapies, challenges, and future directions of transcranial focused ultrasound technology: advances in diagnosis and treatment. JAMA Neurol. 2018;75(2):246–54. https://doi.org/10.1001/jamaneurol.2017.3129.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Hui Ming Khoo, Jean Gotman, Jeffery A. Hall, and François Dubeau declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Epilepsy
Rights and permissions
About this article
Cite this article
Khoo, H.M., Gotman, J., Hall, J.A. et al. Treatment of Epilepsy Associated with Periventricular Nodular Heterotopia. Curr Neurol Neurosci Rep 20, 59 (2020). https://doi.org/10.1007/s11910-020-01082-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s11910-020-01082-y