Abstract
Purpose of Review
The goal of this article is to highlight how and why urinalyses and urine cultures are misused, review quality improvement interventions to optimize urine culture utilization, and highlight how to implement successful, sustainable interventions to improve urine culture practices in the acute care setting.
Recent Findings
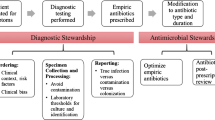
Quality improvement initiatives aimed at reducing inappropriate treatment of asymptomatic bacteriuria often focus on optimizing urine test utilization (i.e., urine culture stewardship). Urine culture stewardship interventions in acute care hospitals span the spectrum of quality improvement initiatives, ranging from strong systems-based interventions like suppression of urine culture results to weaker interventions that focus on clinician education alone. While most urine culture stewardship interventions have met with some success, overall results are mixed, and implementation strategies to improve sustainability are not well understood.
Summary
Successful diagnostic stewardship interventions are based on an assessment of underlying key drivers and focus on multifaceted and complementary approaches. Individual intervention components have varying impacts on effectiveness, provider autonomy, and sustainability. The best urine culture stewardship strategies ultimately include both technical and socio-adaptive components with long-term, iterative feedback required for sustainability.

Similar content being viewed by others
References
Wilson ML, Gaido L. Laboratory diagnosis of urinary tract infections in adult patients. Clin Infect Dis. 2004;38(8):1150–8.
Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D, et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis. 2019;68(10):1611–5.
Trautner BW, Petersen NJ, Hysong SJ, Horwitz D, Kelly PA, Naik AD. Overtreatment of asymptomatic bacteriuria: identifying provider barriers to evidence-based care. Am J Infect Control. 2014;42(6):653–8.
Trautner BW. Asymptomatic bacteriuria: when the treatment is worse than the disease. Nat Rev Urol. 2011;9(2):85–93.
Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D, et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis. 2019.
Advani SD, Fakih MG. The evolution of catheter-associated urinary tract infection (CAUTI): is it time for more inclusive metrics? Infect Control Hosp Epidemiol. 2019:1–5.
Garibaldi RA, Mooney BR, Epstein BJ, Britt MR. An evaluation of daily bacteriologic monitoring to identify preventable episodes of catheter-associated urinary tract infection. Infect Control. 1982;3(6):466–70.
Eddeland A, Hedelin H. Bacterial colonization of the lower urinary tract in women with long-term indwelling urethral catheter. Scand J Infect Dis. 1983;15(4):361–5.
Trautner BW. Urinary tract infection as a continuum-implications for diagnostic and antibiotic stewardship. Clin Infect Dis. 2020.
Tambyah PA, Maki DG. The relationship between pyuria and infection in patients with indwelling urinary catheters: a prospective study of 761 patients. Arch Intern Med. 2000;160(5):673–7.
Nicolle LE. Asymptomatic bacteriuria: review and discussion of the IDSA guidelines. Int J Antimicrob Agents. 2006;28(Suppl 1):S42–8.
Biggel M, Heytens S, Latour K, Bruyndonckx R, Goossens H, Moons P. Asymptomatic bacteriuria in older adults: the most fragile women are prone to long-term colonization. BMC Geriatr. 2019;19(1):170.
Petty LA, Vaughn VM, Flanders SA, Patel T, Malani AN, Ratz D, et al. Assessment of testing and treatment of asymptomatic bacteriuria initiated in the emergency department. Open Forum Infect Dis. 2020;7(12):ofaa537.
Petty LA, Vaughn VM, Flanders SA, Malani AN, Conlon A, Kaye KS, et al. Risk factors and outcomes associated with treatment of asymptomatic bacteriuria in hospitalized patients. JAMA Intern Med. 2019.
Advani SD, Gao CA, Datta R, Sann L, Smith C, Leapman MS, et al. Knowledge and practices of physicians and nurses related to urine cultures in catheterized patients: an assessment of adherence to IDSA guidelines. Open Forum Infect Dis. 2019;6(8).
CDC. National Healthcare Safety Network (NHSN) Patient safety component manual. January 2017. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–63.
Al-Qas Hanna F, Sambirska O, Iyer S, Szpunar S, Fakih MG. Clinician practice and the National Healthcare Safety Network definition for the diagnosis of catheter-associated urinary tract infection. Am J Infect Control. 2013;41(12):1173–7.
Petty LA, Vaughn VM, Flanders SA, Malani AN, Conlon A, Kaye KS, et al. Risk factors and outcomes associated with treatment of asymptomatic bacteriuria in hospitalized patients. JAMA Intern Med. 2019;179(11):1519–27.
Vaughn VM, Chopra V. Revisiting the panculture. BMJ Qual Saf. 2017;26(3):236–9.
Strand CL, Wajsbort RR, Sturmann K. Effect of iodophor vs iodine tincture skin preparation on blood culture contamination rate. JAMA. 1993;269(8):1004–6.
Fakih MG, Advani SD, Vaughn VM. Diagnosis of urinary tract infections: need for a reflective rather than reflexive approach. Infect Control Hosp Epidemiol. 2019:1–2.
Fakih MG, Khatib R. Improving the culture of culturing: critical asset to antimicrobial stewardship. Infect Control Hosp Epidemiol. 2017;38(3):377–9.
Awadalla R, Gnjidic D, Patanwala A, Sakiris M, Penm J. The effectiveness of stewardship interventions to reduce the prescribing of extended-release opioids for acute pain: a systematic review. Pain Med. 2020;21(10):2401–11.
Frontera JA, Wang E, Phillips M, Radford M, Sterling S, Delorenzo K, et al. Protocolized urine sampling is associated with reduced catheter-associated urinary tract infections: a pre- and post-intervention study. Clin Infect Dis. 2020.
Lamb MJ, Baillie L, Pajak D, Flynn J, Bansal V, Simor A, et al. Elimination of screening urine cultures prior to elective joint arthroplasty. Clin Infect Dis. 2017;64(6):806–9.
Claeys KC, Blanco N, Morgan DJ, Leekha S, Sullivan KV. Advances and challenges in the diagnosis and treatment of urinary tract infections: the need for diagnostic stewardship. Curr Infect Dis Rep. 2019;21(4):11.
Sullivan KV, Morgan DJ, Leekha S. Use of diagnostic stewardship practices to improve urine culturing among SHEA Research Network hospitals. Infect Control Hosp Epidemiol. 2019;40(2):228–31.
Ling D, Seidelman J, Dodds-Ashley E, Lewis S, Moehring RW, Anderson DJ, et al. Navigating reflex urine culture practices in community hospitals: need for a validated approach. Am J Infect Control. 2020.
Redwood R, Knobloch MJ, Pellegrini DC, Ziegler MJ, Pulia M, Safdar N. Reducing unnecessary culturing: a systems approach to evaluating urine culture ordering and collection practices among nurses in two acute care settings. Antimicrob Resist Infect Control. 2018;7:4.
Humphries RM, Dien BJ. Point-counterpoint: reflex cultures reduce laboratory workload and improve antimicrobial stewardship in patients suspected of having urinary tract infections. J Clin Microbiol. 2016;54(2):254–8.
Epstein L, Edwards JR, Halpin AL, Preas MA, Blythe D, Harris AD, et al. Evaluation of a novel intervention to reduce unnecessary urine cultures in intensive care units at a tertiary care hospital in Maryland, 2011–2014. Infect Control Hosp Epidemiol. 2016;37(5):606–9.
Lynch CS, Appleby-Sigler A, Bork JT, Dave R, Agnes K, Sanikop M, et al. Effect of urine reflex culturing on rates of cultures and infections in acute and long-term care. Antimicrob Resist Infect Control. 2020;9(1):96.
Howard-Anderson JR, Ashraf S, Overton EC, Reif L, Murphy DJ, Jacob JT. Sustained decrease in urine culture utilization after implementing a reflex urine culture intervention: a multicenter quasi-experimental study. Infect Control Hosp Epidemiol. 2020;41(3):369–71.
Claeys KC, Zhan M, Pineles L, Lydecker A, Clore G, Goto M, et al. Conditional reflex to urine culture: evaluation of a diagnostic stewardship intervention within the Veterans’ Affairs and Centers for Disease Control and Prevention Practice-Based Research Network. Infect Control Hosp Epidemiol. 2021;42(2):176–81.
Munigala S, Rojek R, Wood H, Yarbrough ML, Jackups RR, Burnham CD, et al. Effect of changing urine testing orderables and clinician order sets on inpatient urine culture testing: analysis from a large academic medical center. Infect Control Hosp Epidemiol. 2019;40(3):281–6.
Smith MA, Puckrin R, Lam PW, Lamb MJ, Simor AE, Leis JA. Association of increased colony-count threshold for urinary pathogens in hospitalized patients with antimicrobial treatment. JAMA Intern Med. 2019;179(7):990–2.
Lee ALH, Leung ECM, Lee MKP, Lai RWM. Diagnostic stewardship programme for urine culture: impact on antimicrobial prescription in a multi-centre cohort. J Hosp Infect. 2021;108:81–9.
Vaughn VM, Linder JA. Thoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient care. BMJ Qual Saf. 2018;27(8):583–6.
Thaler RH SR. Nudge: Penguin Books; 2009.
Shirley D, Scholtz H, Osterby K, Musuuza J, Fox B, Safdar N. Optimizing inpatient urine culture ordering practices using the electronic medical record: a pilot study. Infect Control Hosp Epidemiol. 2017;38(4):486–8.
Watson KJ, Trautner B, Russo H, Phe K, Lasco T, Pipkins T, et al. Using clinical decision support to improve urine culture diagnostic stewardship, antimicrobial stewardship, and financial cost: a multicenter experience. Infect Control Hosp Epidemiol. 2020;41(5):564–70.
Lin G, Knowlson S, Nguyen H, Cooper K, Pryor RJ, Doll M, et al. Urine test stewardship for catheterized patients in the critical care setting: provider perceptions and impact of electronic order set interventions. Am J Infect Control. 2019;47(10):1277–9.
Liao S, Rhodes J, Jandarov R, DeVore Z, Sopirala MM. Out of sight-out of mind: impact of cascade reporting on antimicrobial usage. Open Forum Infect Dis. 2020;7(2):ofaa002.
Leis JA, Rebick GW, Daneman N, Gold WL, Poutanen SM, Lo P, et al. Reducing antimicrobial therapy for asymptomatic bacteriuria among noncatheterized inpatients: a proof-of-concept study. Clin Infect Dis. 2014;58(7):980–3.
Daley P, Garcia D, Inayatullah R, Penney C, Boyd S. Modified reporting of positive urine cultures to reduce inappropriate treatment of asymptomatic bacteriuria among nonpregnant, noncatheterized inpatients: a randomized controlled trial. Infect Control Hosp Epidemiol. 2018;39(7):814–9.
Duhigg C. The power of habit: why we do what we do in life and business.: New York Random House; 2012.
Dougherty DF, Rickwa J, Guy D, Keesee K, Martin BJ, Smith J, et al. Reducing inappropriate urine cultures through a culture standardization program. Am J Infect Control. 2020;48(6):656–62.
Sarg M, Waldrop GE, Beier MA, Heil EL, Thom KA, Preas MA, et al. Impact of changes in urine culture ordering practice on antimicrobial utilization in intensive care units at an academic medical center. Infect Control Hosp Epidemiol. 2016;37(4):448–54.
Davies PE, Daley MJ, Hecht J, Hobbs A, Burger C, Watkins L, et al. Effectiveness of a bundled approach to reduce urinary catheters and infection rates in trauma patients. Am J Infect Control. 2018;46(7):758–63.
Gawande A. The checklist manifesto. London, England: Profile Books; 2011.
Mullin KM, Kovacs CS, Fatica C, Einloth C, Neuner EA, Guzman JA, et al. A multifaceted approach to reduction of catheter-associated urinary tract infections in the intensive care unit with an emphasis on “stewardship of culturing.” Infect Control Hosp Epidemiol. 2017;38(2):186–8.
Sampathkumar P, Barth JW, Johnson M, Marosek N, Johnson M, Worden W, et al. Mayo Clinic reduces catheter-associated urinary tract infections through a Bundled 6-C Approach. Jt Comm J Qual Patient Saf. 2016;42(6):254–61.
Sampathkumar P. Reducing catheter-associated urinary tract infections in the ICU. Curr Opin Crit Care. 2017;23(5):372–7.
Huang GC, Kriegel G, Wheaton C, Sternberg S, Sands K, Richards J, et al. Implementation of diagnostic pauses in the ambulatory setting. BMJ Qual Saf. 2018;27(6):492–7.
Loeb M, Brazil K, Lohfeld L, McGeer A, Simor A, Stevenson K, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ. 2005;331(7518):669.
Luu A, Dominguez F, Yeshoua B, Vo C, Nallapa S, Chung D, et al. Reducing catheter associated urinary tract infections via cost-saving diagnostic stewardship. Clin Infect Dis. 2020.
CDC. Core elements of antibiotic stewardship. 2021. Available from: https://www.cdc.gov/antibiotic-use/core-elements/index.html.
Bonnal C, Baune B, Mion M, Armand-Lefevre L, L’Heriteau F, Wolmark Y, et al. Bacteriuria in a geriatric hospital: impact of an antibiotic improvement program. J Am Med Dir Assoc. 2008;9(8):605–9.
Linares LA, Thornton DJ, Strymish J, Baker E, Gupta K. Electronic memorandum decreases unnecessary antimicrobial use for asymptomatic bacteriuria and culture-negative pyuria. Infect Control Hosp Epidemiol. 2011;32(7):644–8.
Jackson EC, Thai XC, Bruno-Murtha LA, Barner AE. Impact of tiered interventions to decrease routine urine cultures in asymptomatic patients undergoing arthroplasty. Infect Control Hosp Epidemiol. 2019;40(1):109–10.
Fabre V, Pleiss A, Klein E, Demko Z, Salinas A, Jones G, et al. A pilot study to evaluate the impact of a nurse-driven urine culture diagnostic stewardship intervention on urine cultures in the acute care setting. Jt Comm J Qual Patient Saf. 2020;46(11):650–5.
Sumner S, Forsyth S, Collette-Merrill K, Taylor C, Vento T, Veillette J, et al. Antibiotic stewardship: the role of clinical nurses and nurse educators. Nurse Educ Today. 2018;60:157–60.
Edwards R, Drumright L, Kiernan M, Holmes A. Covering more territory to fight resistance: considering nurses’ role in antimicrobial stewardship. J Infect Prev. 2011;12(1):6–10.
Olans RN, Olans RD, DeMaria A Jr. The critical role of the staff nurse in antimicrobial stewardship–unrecognized, but already there. Clin Infect Dis. 2016;62(1):84–9.
Olans RD, Olans RN, Witt DJ. Good nursing is good antibiotic stewardship. Am J Nurs. 2017;117(8):58–63.
Wight D, Wimbush E, Jepson R, Doi L. Six steps in quality intervention development (6SQuID). J Epidemiol Community Health. 2016;70(5):520–5.
Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Crit Care Med. 2018;46(6):997–1000.
Ashiru-Oredope D, Sharland M, Charani E, McNulty C, Cooke J, Group AAS. Improving the quality of antibiotic prescribing in the NHS by developing a new antimicrobial stewardship programme: start smart–then focus. J Antimicrob Chemother. 2012;67(Suppl 1):i51-63.
Saint S, Kowalski CP, Banaszak-Holl J, Forman J, Damschroder L, Krein SL. The importance of leadership in preventing healthcare-associated infection: results of a multisite qualitative study. Infect Control Hosp Epidemiol. 2010;31(9):901–7.
Khaw C, Oberle AD, Lund BC, Egge J, Heintz BH, Erickson BA, et al. Assessment of guideline discordance with antimicrobial prophylaxis best practices for common urologic procedures. JAMA Netw Open. 2018;1(8):e186248.
Vaughn VM, Gupta A, Petty LA, Gandhi TN, Flanders S, Swaminathan L, Hsaiky L, Ratz D, Horowitz J, McLaughlin E, Chopra V. Misdiagnosis of urinary tract and misdiagnosis of pneumonia linked at the hospital level: a multi-hospital cohort study. Society of Hospital Medicine Annual meeting. 2020;187.
Wiltsey Stirman S, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci. 2012;7:17.
Gupta K, O’Brien W, Gallegos-Salazar J, Strymish J, Branch-Elliman W. How testing drives treatment in asymptomatic patients: level of pyuria directly predicts probability of antimicrobial prescribing. Clin Infect Dis. 2020;71(3):614–21.
Anand A, Ballinger B, Ganti L. Impact of urinalysis on medical decision-making and length of stay. Cureus. 2018;10(4):e2531.
Khawcharoenporn T, Vasoo S, Ward E, Singh K. Abnormal urinalysis finding triggered antibiotic prescription for asymptomatic bacteriuria in the ED. Am J Emerg Med. 2011;29(7):828–30.
Neyman G, Dalsey W. A Quantification of the impact of awaiting results of a urinalysis upon emergency department length of stay. J Emerg Med. 2021;60(2):158–64.
Klein CN, Elman MR, Townes JM, Lewis JS, McGregor JC. Unintended consequences of a reflex urine culture order set on appropriate antibiotic use. Infect Control Hosp Epidemiol. 2020;41(9):1090–2.
Dietz J, Lo TS, Hammer K, Zegarra M. Impact of eliminating reflex urine cultures on performed urine cultures and antibiotic use. Am J Infect Control. 2016;44(12):1750–1.
Advani S, Polage C, Fakih M. Deconstructing the urinalysis: A novel approach to diagnostic and antimicrobial stewardship. Antimicrobial Stewardship & Healthcare Epidemiology 2021;1(1), E6. https://doi.org/10.1017/ash.2021.167.
Fakih MG, Krein SL, Edson B, Watson SR, Battles JB, Saint S. Engaging health care workers to prevent catheter-associated urinary tract infection and avert patient harm. Am J Infect Control. 2014;42(10 Suppl):S223–9.
Reynolds SS, Sova CD, Lewis SS, Smith BA, Wrenn RH, Turner NA, et al. Sustained reduction in catheter-associated urinary tract infections using multi-faceted strategies led by champions: a quality improvement initiative. Infect Control Hosp Epidemiol. 2021:1–5.
Saint S, Greene MT, Krein SL, Rogers MA, Ratz D, Fowler KE, et al. A Program to prevent catheter-associated urinary tract infection in acute care. N Engl J Med. 2016;374(22):2111–9.
Fakih MG, George C, Edson BS, Goeschel CA, Saint S. Implementing a national program to reduce catheter-associated urinary tract infection: a quality improvement collaboration of state hospital associations, academic medical centers, professional societies, and governmental agencies. Infect Control Hosp Epidemiol. 2013;34(10):1048–54.
Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon. 2014;45(1):14–25.
Acknowledgements
We would like to thank Dr. David Weber, Professor of Medicine, Infectious diseases, University of North Carolina, for review of the manuscript.
Funding
SA reports grants from the CDC, NIH NIDDK K12 (K12DK100024), SHEA and consulting fees from IPEC Experts, LLC (co-owner) and IDSA. VV reports grants from AHRQ, Gordon and Betty Moore Foundation, NHBLI, NIA, and SHEA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
NA.
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
NA.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Healthcare Associated Infections
Rights and permissions
About this article
Cite this article
Advani, S., Vaughn, V.M. Quality Improvement Interventions and Implementation Strategies for Urine Culture Stewardship in the Acute Care Setting: Advances and Challenges. Curr Infect Dis Rep 23, 16 (2021). https://doi.org/10.1007/s11908-021-00760-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s11908-021-00760-3