Abstract
Purpose of Review
The objective of this study was to describe the increasing incidence and risk of cardiovascular disease among persons living with HIV (PLWH) in Sub-Saharan Africa. We also used data to compare hypertension (a common NCD among PLWH) outcomes between PLWH and HIV–uninfected individuals among older adults in Northwestern Tanzania.
Recent Findings
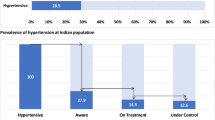
Hypertension is increasingly common in Sub-Saharan Africa and a leading cause of cardiovascular disease for PLWH. Among those with hypertension, PLWH have a 50% higher risk of incident myocardial infarction compared to the general population. In response to the rising incidence of these non-communicable diseases (NCDs) among PLWH, recently, the Joint United Nations Program on HIV/AIDS supported the integration of NCD care into routine clinical care for HIV. However, data are lacking on levels of awareness of hypertension status, diagnosis, and antihypertensive medication adherence.
Summary
Given the higher likelihood of elevated blood pressure among PLWH, there is an urgent need to implement interventions to improve blood pressure control in this population. Researchers should evaluate treatment barriers at multiple levels including health system, healthcare providers, and patients’ level and tailor evidence-based interventions to increase achievement of blood pressure control for PLWH.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as:
•• Of major importance
Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep. 2013;15(3):134–6.
Relief, U.S.P.s.E.P.f.A. PEPFAR 2020 annual report to congress. 2020 [cited 2021 January 5]; Available from: https://www.state.gov/wp-content/uploads/2020/09/PEPFAR2020ARC.pdf.
Haregu TN, et al. National responses to HIV/AIDS and non-communicable diseases in developing countries: analysis of strategic parallels and differences. J Public Health Res. 2014;3(1):99–99.
Njuguna B, et al., Models of integration of HIV and noncommunicable disease care in sub-Saharan Africa: lessons learned and evidence gaps. AIDS (London, England). 2018;32 Suppl 1(Suppl 1):S33-S42.
Gazzaruso C, et al. Hypertension among HIV patients: prevalence and relationships to insulin resistance and metabolic syndrome. J Hypertens. 2003;21(7):1377–82.
Peck RN, et al. Hypertension, kidney disease, HIV and antiretroviral therapy among Tanzanian adults: a cross-sectional study. BMC Med. 2014;12:125.
Nduka CU, et al. Evidence of increased blood pressure and hypertension risk among people living with HIV on antiretroviral therapy: a systematic review with meta-analysis. J Hum Hypertens. 2016;30(6):355–62.
Pearce D, et al. Comparison of in-hospital mortality from acute myocardial infarction in HIV sero-positive versus sero-negative individuals. Am J Cardiol. 2012;110(8):1078–84.
Ladapo JA, et al. Disparities in the quality of cardiovascular care between HIV-infected versus HIV-uninfected adults in the United States: a cross-sectional study. J Am Heart Assoc. 2017;6(11).
Lattanzi S, Brigo F, Silvestrini M. Integrated care of hypertension and HIV infection. J Clin Hypertens (Greenwich). 2018;20(10):1493–5.
Riestenberg RA, et al. Differences in statin utilization and lipid lowering by race, ethnicity, and HIV status in a real-world cohort of persons with human immunodeficiency virus and uninfected persons. Am Heart J. 2019;209:79–87.
Armah KA, et al. Prehypertension, hypertension, and the risk of acute myocardial infarction in HIV-infected and -uninfected veterans. Clin Infect Dis. 2014;58(1):121–9.
Burkholder GA, et al. Racial disparities in the prevalence and control of hypertension among a cohort of HIV-infected patients in the southeastern United States. PLoS ONE. 2018;13(3):e0194940–e0194940.
De Socio GV, et al. Prevalence, awareness, treatment, and control rate of hypertension in HIV-infected patients: the HIV-HY study. Am J Hypertens. 2014;27(2):222–8.
•• So-Armah K, et al. HIV and cardiovascular disease. Lancet HIV. 2020;7(4):e279–93.
UNAIDS. Chronic care of HIV and noncommunicable diseases 2011 [cited 2021 January 5]; Available from: https://www.unaids.org/sites/default/files/media_asset/20110526_JC2145_Chronic_care_of_HIV_0.pdf
Duffy M, et al. Non-communicable diseases and HIV care and treatment: models of integrated service delivery. Trop Med Int Health. 2017;22(8):926–37.
Leung C, et al. Preparedness of HIV care and treatment clinics for the management of concomitant non-communicable diseases: a cross-sectional survey. BMC Public Health. 2016;16(1):1002.
Wozniak G, et al. Hypertension control cascade: a framework to improve hypertension awareness, treatment, and control. J clinical hypertension (Greenwich, Conn.). 2016;18(3):232–239.
Melmer A, Laimer M. Treatment goals in diabetes. Endocr Dev. 2016;31:1–27.
Schaiff RAB, Moe RM, Krichbaum DW. An overview of cholesterol management. American health & drug benefits. 2008;1(9):39–48.
Screening for High blood pressure in adults. recommendation statement. Am Fam Physician. 2016;93(4):300–2.
Piper MA, EC, Burda BU, et al. Screening for high blood pressure in adults: a systematic evidence review for the U.S. preventive services task force Evidence syntheses, No. 121 2014 [cited 2021 Feb 1]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK269497/.
WHO. The WHO STEPwise approach to noncommunicable disease risk factor surveillance (STEPS): WHO STEPS Instrument (Core and Expanded). [cited 2021 Feb 1]; Available from: http://www.who.int/ncds/surveillance/steps/STEPS_Instrument.pdf.
Simmons D, Williams DR. Random blood glucose as a screening test for diabetes in a biethnic population. Diabet Med. 1994;11(9):830–5.
O’Brien E, Parati G, Stergiou G. Ambulatory blood pressure measurement: what is the international consensus? Hypertension. 2013;62(6):988–94.
Gill GV, et al. Random blood glucose estimation in type 2 diabetes: does it reflect overall glycaemic control? Diabet Med. 1994;11(7):705–8.
Casadei K, Kiel J. Anthropometric measurement, in StatPearls. 2020, StatPearls Publishing. Copyright © 2020, StatPearls Publishing LLC.: Treasure Island (FL).
Lyamuya EF, et al. Evaluation of simple rapid HIV assays and development of national rapid HIV test algorithms in Dar es Salaam, Tanzania. BMC Infect Dis. 2009;9(1):19.
Adinan J, et al. Preparedness of health facilities in managing hypertension & diabetes mellitus in Kilimanjaro, Tanzania: a cross sectional study. BMC Health Serv Res. 2019;19(1):537–537.
Peck R, et al. Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: a cross-sectional survey. Lancet Glob Health. 2014;2(5):e285–92.
Dewhurst MJ, et al. The high prevalence of hypertension in rural-dwelling Tanzanian older adults and the disparity between detection, treatment and control: a rule of sixths? J Hum Hypertens. 2013;27(6):374–80.
Kayima J, et al. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord. 2013;13:54.
Dillon DG, et al. Association of HIV and ART with cardiometabolic traits in sub-Saharan Africa: a systematic review and meta-analysis. Int J Epidemiol. 2013;42(6):1754–71.
Tibebu A, Mengistu D, Bulto LN. Adherence to prescribed antihypertensive medications and associated factors for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa. Ethiopia Int J Health Sci (Qassim). 2017;11(4):47–52.
Burnier M, Polychronopoulou E, Wuerzner G. Hypertension and drug adherence in the elderly. Front Cardiovasc Med. 2020;7:49.
Harris TG, Rabkin M, El-Sadr WM. Achieving the fourth 90: healthy aging for people living with HIV. AIDS (London, England). 2018;32(12):1563–9.
Muiruri C, et al. Opportunities to leverage telehealth approaches along the hypertension control cascade in Sub-Saharan Africa. Curr Hypertens Rep. 2019;21(10):75–75.
Acknowledgements
We would like to thank all the participants at the BMC CTC and the participants from the Nyamagana and Ilemela districts. We also would like to thank the chairperson of each ward and the medical officers’ representatives in Nyamagana and Ilemela districts, Dr. Wemaeli Mweteni, CTC staff, and research assistants who assisted with data collection.
Funding
This research was supported by the Fogarty International Centre of the National Institutes of Health under Award Number D43TW010138. CM effort was supported by a diversity supplement from the National Heart, Lung, and Blood Institute of the National Institutes of Health (NHLBI) U01HL142099-01S1 and K01 HL159052. We also acknowledge support received from the Duke University Center for AIDS Research grant 5P30AI064518. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Telemedicine and Technology
Rights and permissions
About this article
Cite this article
Muiruri, C., Wajanga, B., Kim, C. et al. Correlates of Blood Pressure Awareness, Treatment, and Control Among Adults 50 Years or Older by HIV Status in Northwestern Tanzania. Curr Hypertens Rep 24, 259–266 (2022). https://doi.org/10.1007/s11906-022-01188-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-022-01188-3