Abstract
Purpose of Review
The goal of the present review is to describe the current findings on the association of sleep with resistant hypertension (hypertension that remains uncontrolled despite the use of three or more antihypertensive medications from different classes, including a diuretic).
Recent Findings
Sleep disturbances, particularly obstructive sleep apnea (OSA), are highly prevalent among adults who have resistant hypertension. Randomized controlled trials indicate that treating OSA has modest effects on blood pressure lowering among those with the highest initial blood pressure. There is a paucity of research on the association of habitual sleep and other sleep disturbances with resistant hypertension. Of note, the most recent observational studies describing the association of OSA with resistant hypertension are comprised primarily of non-white race/ethnic groups who are far more likely to have resistant hypertension.
Summary
OSA is associated with resistant hypertension, but there is limited data on associations between sleep characteristics and resistant hypertension. Future studies should investigate whether treating OSA can reduce disparities in resistant hypertension and whether other aspects of sleep also contribute to resistant hypertension.
Similar content being viewed by others
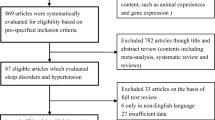
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Carey RM, Sakhuja S, Calhoun DA, et al. Prevalence of apparent treatment-resistant hypertension in the United States. Hypertension. 2019;73(2):424–31. This paper describes the prevalence of treatment resistant hypertension in the US population.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127–248.
• Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5):e53–90. This paper provides current treatment guidelines for managing resistant hypertension including recommendations for screening for obstructive sleep apnea.
Noubiap JJ, Nansseu JR, Nyaga UF, Sime PS, Francis I, Bigna JJ. Global prevalence of resistant hypertension: a meta-analysis of data from 3.2 million patients. Heart. 2019;105(2):98–105.
Acelajado MC, Pisoni R, Dudenbostel T, Dell’Italia LJ, Cartmill F, Zhang B, et al. Refractory hypertension: definition, prevalence, and patient characteristics. J Clin Hypertens (Greenwich). 2012;14(1):7–12.
National Center for Health Statistics. Summary health statistics tables for US adults: National Health Interview Survey 2014. 2016. (http://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2014_SHS_Table_A-1.pdf). (Accessed September 28 2016).
Tarver-Carr ME, Powe NR, Eberhardt MS, et al. Excess risk of chronic kidney disease among African-American versus white subjects in the United States: a population-based study of potential explanatory factors. J Am Soc Nephrol. 2002;13(9):2363–70.
Muntner P, Newsome B, Kramer H, Peralta CA, Kim Y, Jacobs DR, et al. Racial differences in the incidence of chronic kidney disease. Clin J Am Soc Nephrol. 2012;7(1):101–7.
Fryar CD, Ostchega Y, Hales CM, et al. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data Brief. 2017;289:1–8.
Zhao B, Jose PO, Pu J, et al. Racial/ethnic differences in hypertension prevalence, treatment, and control for outpatients in northern California 2010-2012. Am J Hypertens. 2015;28(5):631–9.
Sorlie PD, Allison MA, Avilés-Santa ML, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic community health study/study of Latinos. Am J Hypertens. 2014;27(6):793–800.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24(2):215–33.
Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144(7):485–95.
Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–62.
In: Colten HR, Altevogt BM, eds. Sleep disorders and sleep deprivation: an unmet public health problem. Washington (DC), 2006.
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17.
Zamarrón C, Valdés Cuadrado L, Álvarez-Sala R. Pathophysiologic mechanisms of cardiovascular disease in obstructive sleep apnea syndrome. Pulmonary Medicine. 2013;2013:521087.
Jean-Louis G, Zizi F, Clark LT, et al. Obstructive sleep apnea and cardiovascular disease: role of the metabolic syndrome and its components. J Clin Sleep Med. 2008;4(3):261–72.
Pedrosa RP, Drager LF, Gonzaga CC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811–7.
Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L, Manios Y, et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes. 2011;35(10):1308–17.
Riegel B, Moelter ST, Ratcliffe SJ, Pressler SJ, de Geest S, Potashnik S, et al. Excessive daytime sleepiness is associated with poor medication adherence in adults with heart failure. J Card Fail. 2011;17(4):340–8.
Marcus JA, Pothineni A, Marcus CZ, Bisognano JD. The role of obesity and obstructive sleep apnea in the pathogenesis and treatment of resistant hypertension. Curr Hypertens Rep. 2014;16(1):411.
Goncalves SC, Martinez D, Gus M, et al. Obstructive sleep apnea and resistant hypertension: a case-control study. Chest. 2007;132(6):1858–62.
Demede M, Pandey A, Zizi F, et al. Resistant hypertension and obstructive sleep apnea in the primary-care setting. Int J Hypertens. 2011;2011:340929.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension 2018;71(6):e13-e115.
•• Bhandari SK, Shi J, Molnar MZ, et al. Comparisons of sleep apnoea rate and outcomes among patients with resistant and non-resistant hypertension. Respirology. 2016;21(8):1486–92. This is one of two new original research manuscripts to describe the association of obstructive sleep apnea defined using clinical diagnosis codes with hypertension in a large managed care system.
•• Johnson DA, Thomas SJ, Abdalla M, et al. Association between sleep apnea and blood pressure control among blacks: Jackson Heart Sleep Study. Circulation. 2018;. This is one of two new original research studies to describe the association of obstructive sleep apnea as diagnosed using a type 3 apnea screening device with hypertension in a cohort study comprised exclusively of African Americans.
Carnethon MR, Pu J, Howard G, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393–423.
Alajmi M, Mulgrew AT, Fox J, Davidson W, Schulzer M, Mak E, et al. Impact of continuous positive airway pressure therapy on blood pressure in patients with obstructive sleep apnea hypopnea: a meta-analysis of randomized controlled trials. Lung. 2007;185(2):67–72.
Hla KM, Young T, Finn L, Peppard PE, Szklo-Coxe M, Stubbs M. Longitudinal association of sleep-disordered breathing and nondipping of nocturnal blood pressure in the Wisconsin sleep cohort study. Sleep. 2008;31(6):795–800.
• Liu L, Cao Q, Guo Z, Dai Q. Continuous positive airway pressure in patients with obstructive sleep apnea and resistant hypertension: a meta-analysis of randomized controlled trials. J Clin Hypertens (Greenwich). 2016;18(2):153–8. This meta-analysis of five studies describes a positive association of treatment of obstructive sleep apnea with 24-hour blood pressure values.
• Lei Q, Lv Y, Li K, Ma L, du G, Xiang Y, et al. Effects of continuous positive airway pressure on blood pressure in patients with resistant hypertension and obstructive sleep apnea: a systematic review and meta-analysis of six randomized controlled trials. Jornal brasileiro de pneumologia : publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia. 2017;43(5):373–9. This meta-analysis that includes six studies that describe a positive association of treatment of obstructive sleep apnea with 24-hour blood pressure parameters.
Thomas SJ, Calhoun D. Sleep, insomnia, and hypertension: current findings and future directions. Journal of the American Society of Hypertension : JASH. 2017;11(2):122–9.
Jarrin DC, Alvaro PK, Bouchard MA, Jarrin SD, Drake CL, Morin CM. Insomnia and hypertension: a systematic review. Sleep Med Rev. 2018;41:3–38.
Egan KJ, Knutson KL, Pereira AC, von Schantz M. The role of race and ethnicity in sleep, circadian rhythms and cardiovascular health. Sleep Med Rev. 2017;33:70–8.
Czeisler CA, Duffy JF, Shanahan TL, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 1999;284(5423):2177–81.
Kawachi I, Colditz GA, Stampfer MJ, Willett WC, Manson JAE, Speizer FE, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92(11):3178–82.
Chung MH, Kuo TB, Hsu N, et al. Sleep and autonomic nervous system changes - enhanced cardiac sympathetic modulations during sleep in permanent night shift nurses. Scand J Work Environ Health. 2009;35(3):180–7.
Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–9.
Vyas MV, Garg AX, Iansavichus AV, Costella J, Donner A, Laugsand LE, et al. Shift work and vascular events: systematic review and meta-analysis. BMJ. 2012;345:e4800.
Scheer FA, Hilton MF, Mantzoros CS, et al. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009;106(11):4453–8.
Knutson KL, Van Cauter E, Rathouz PJ, et al. Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med. 2009;169(11):1055–61.
Grandner MA, Perlis ML. Short sleep duration and insomnia associated with hypertension incidence. Hypertens Res. 2013;36(11):932–3.
Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143–72.
Seravalle G, Mancia G, Grassi G. Sympathetic nervous system, sleep, and hypertension. Curr Hypertens Rep. 2018;20(9):74.
Buford TW. Hypertension and aging. Ageing Res Rev. 2016;26:96–111.
• St-Onge MP, Grandner MA, Brown D, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation. 2016;134(18):e367–e86. This is a scientific statement from the American Heart Association describing the correlation of multiple domains of sleep health with cardiovascular diseases, including a description of mechanisms.
Tan X, Chapman CD, Cedernaes J, Benedict C. Association between long sleep duration and increased risk of obesity and type 2 diabetes: a review of possible mechanisms. Sleep Med Rev. 2018;40:127–34.
Spiegel K, Tasali E, Penev P, Cauter EV. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–50.
Chaput JP. Sleep patterns, diet quality and energy balance. Physiol Behav. 2014;134:86–91.
Atkinson G, Davenne D. Relationships between sleep, physical activity and human health. Physiol Behav. 2007;90(2–3):229–35.
•• McEwen BS, Karatsoreos IN. Sleep deprivation and circadian disruption: stress, allostasis, and allostatic load. Sleep Med Clin. 2015;10(1):1–10. This is the first published randomized controlled trial testing whether an intervention for poor self-reported sleep was associated with blood pressure lowering. While the study showed positive associations on sleep, there was no difference in blood pressure.
Foster RG, Peirson SN, Wulff K, et al. Sleep and circadian rhythm disruption in social jetlag and mental illness. Prog Mol Biol Transl Sci. 2013;119:325–46.
McGrath ER, Espie CA, Power A, et al. Sleep to lower elevated blood pressure: a randomized controlled trial (SLEPT). Am J Hypertens. 2017;30(3):319–27.
Carnethon MR, De Chavez PJ, Zee PC, et al. Disparities in sleep characteristics by race/ethnicity in a population-based sample: Chicago area sleep study. Sleep Med. 2016;18:50–5.
Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18.
Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5):e53–90.
Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: the multi-ethnic study of atherosclerosis (MESA). Sleep. 2015;38(6):877–88.
Rasmussen-Torvik LJ, De Chavez PJ, Kershaw KN, et al. The mediation of racial differences in hypertension by sleep characteristics: Chicago area sleep study. Am J Hypertens. 2016:hpw093.
Curtis DS, Fuller-Rowell TE, El-Sheikh M, et al. Habitual sleep as a contributor to racial differences in cardiometabolic risk. Proc Natl Acad Sci U S A. 2017;114(33):8889–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep and Hypertension
Rights and permissions
About this article
Cite this article
Carnethon, M.R., Johnson, D.A. Sleep and Resistant Hypertension. Curr Hypertens Rep 21, 34 (2019). https://doi.org/10.1007/s11906-019-0941-z
Published:
DOI: https://doi.org/10.1007/s11906-019-0941-z