Abstract
Purpose of Review
Patterns of sexualized drug use, including stimulants (e.g., methamphetamine) and chemsex drugs, are key drivers of HIV incidence among sexual minority men (SMM). Although pre-exposure prophylaxis (PrEP) mitigates HIV risk, there is no consensus regarding the associations of substance use with the PrEP care continuum.
Recent Findings
SMM who use substances are as likely or more likely to use PrEP. Although SMM who use stimulants experience greater difficulties with daily oral PrEP adherence, some evidence shows that SMM who use stimulants or chemsex drugs may achieve better adherence in the context of recent condomless anal sex. Finally, SMM who use substances may experience greater difficulties with PrEP persistence (including retention in PrEP care).
Summary
SMM who use stimulants and other substances would benefit from more comprehensive efforts to support PrEP re-uptake, adherence, and persistence, including delivering behavioral interventions, considering event-based dosing, and providing injectable PrEP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For over two decades, patterns of sexualized drug use (SDU) have emerged worldwide as prominent drivers of HIV incidence among sexual minority men (SMM) — gay, bisexual, and other men who have sex with men [1,2,3,4,5]. This is evident in early findings from a cohort of SMM in Sydney, Australia, which showed that the use of methamphetamine and erectile dysfunction drugs was associated with an eightfold faster rate of HIV seroconversion from 2001 to 2007 [6]. Similarly, findings from a cohort of SMM in Bangkok, Thailand indicated that methamphetamine use and HIV were intertwining epidemics that disproportionately affected younger men and those who found casual partners on the internet [3]. Another recent study of over 9000 SMM from 7 European countries estimated that nearly 20% reported engaging in SDU and 5% reported using chemsex drugs, including mephedrone, methamphetamine, or gamma hydroxybutyrate (GHB) [2]. In the same study, chemsex drug use was associated with the greatest elevations in multiple indicators of HIV risk [2]. Although some evidence showed the declining use of mephedrone and GHB in the UK [7], SDU and chemsex drug use increased in a cohort of SMM in Amsterdam, Netherlands, from 2008 to 2018 [8]. Other recent findings from this Dutch cohort demonstrated that SMM classified as engaging in chemsex drug use had 15-fold greater odds of a sexually transmitted infection (STI) relative to those reporting no substance use [9]. Taken together, expanded HIV prevention efforts are needed for SMM engaging in SDU and chemsex drug use worldwide.
In the USA, longstanding patterns of SDU are linked to HIV incidence among SMM. Distinct combinations of stimulants (e.g., methamphetamine and powder cocaine), amyl nitrites (i.e., poppers), and erectile dysfunction drugs accounted for nearly two-thirds of HIV infections in a national cohort of SMM from 1998 to 2008 [4]. Currently, a resurgent epidemic of methamphetamine use among SMM in the USA is disproportionately affecting Black and Latino SMM [10,11,12,13]. Although methamphetamine use appeared to decline moderately in the USA after significant public health attention in the early to mid-2000s [14, 15], it is again on the rise [16,17,18,19,20,21]. The enduring consequences for the HIV epidemic are evidenced by recent findings from a cohort of sexual and gender minorities who have sex with men, showing 1 in 3 new HIV infections over 12 months occurring among those reporting methamphetamine use [5]. Although methamphetamine use continues to be strongly associated with engagement in condomless anal sex (CAS) [22, 23], emerging evidence shows that men who use methamphetamine and other stimulants display altered rectal cytokines/chemokines [24, 25]. Bearing in mind that 70% of all HIV infections among SMM occur during receptive CAS [26,27,28], the confluence of receptive CAS and dysregulated rectal immune function could explain heightened vulnerability to HIV among SMM who use stimulants.
To optimize HIV prevention efforts, there is a clear need to understand the dynamic interplay of structural, social, and psychological determinants of SDU among SMM. High rates of SDU and its social acceptability in urban SMM communities increase exposure risk through social and sexual networks [29,30,31,32]. Many SMM reside in concentrated neighborhoods within urban centers where the public health impact of SDU is amplified. This is compounded by sexual minority stress processes (e.g., discrimination) that affect the health of SMM [33,34,35,36,37,38], which can serve as obstacles to seeking HIV prevention services and substance use disorder treatment [39]. Consistent with the Cognitive Escape Model [40], SDU can function as a means of avoidant coping to manage sexual minority stress and HIV-related stress [41]. Guided by the syndemics theory, multiple psychosocial health comorbidities have also been shown to co-occur with SDU to synergistically heighten HIV risk among SMM [42,43,44,45,46,47]. For example, there is a dose–response association between a greater burden of syndemic conditions (i.e., stimulant use, polydrug use, heavy alcohol use, depression, and childhood sexual abuse) and faster HIV incidence among SMM [48]. Furthermore, it is well-established that difficulties in managing sexual thoughts, urges, and behaviors (i.e., sexual compulsivity) commonly co-occur with SDU and other syndemic conditions to amplify HIV risk among SMM [42, 49,50,51]. A recent meta-analysis of studies conducted with SMM revealed a modest association between sexual compulsivity with substance use (r = 0.09, SE = 0.02) and a medium association of sexual compulsivity with CAS (r = 0.13, SE = 0.02) [52]. Further research is needed to characterize the multi-level determinants of the intertwining epidemics of SDU and HIV in order to guide more comprehensive public health approaches to HIV prevention for SMM.
HIV Prevention Interventions for SMM Who Use Substances
There is a clear need for integrated pharmacologic and behavioral approaches for the treatment of stimulant use disorders, which are often chronic and relapsing conditions that require ongoing treatment. Placebo-controlled trials conducted to date have focused almost exclusively on methamphetamine use disorder given its association with markedly amplified risk for HIV infection [5]. Although mirtazapine and injectable naltrexone with oral bupropion have shown some promise for the treatment of methamphetamine use disorder [53,54,55], there is currently no sufficient evidence of the efficacy of pharmacotherapies in treating methamphetamine or cocaine disorders across trials [56, 57]. Most placebo-controlled trials have indicated modest rates of adherence to oral pharmacotherapies, with many integrating the delivery of pharmacotherapies with evidence-based behavioral treatments, such as cognitive-behavioral therapy. At this time, behavioral interventions are considered first-line treatments for SMM who use stimulants such as methamphetamine [58], and these can be delivered across the spectrum of stimulant use disorder symptom severity, including those engaging in binge and episodic patterns of use.
Behavioral interventions have demonstrated efficacy for SMM who use substances, but novel approaches are needed to maximize the benefits of pre-exposure prophylaxis (PrEP) [59]. Contingency management (CM), motivational interviewing (MI), and cognitive-behavioral interventions have demonstrated efficacy in decreasing substance use and CAS among SMM [59,60,61], but these effects are often modest and short-lived. The persistent nature of HIV risk in this population is supported by findings where SMM who use methamphetamine have fivefold greater odds of receiving a repeat prescription for post-exposure prophylaxis (PEP) and a threefold greater rate of HIV seroconversion [62]. Although supporting entry or re-entry into the PrEP care continuum is an essential first step, it is likely that many SMM who use substances will benefit from additional support for PrEP adherence and persistence. Even with the advent of injectable PrEP [63], efforts to address retention in PrEP care and PrEP persistence will remain essential components of HIV prevention in this high-priority population. It is also unclear whether SMM who use substances will experience difficulties in accessing injectable PrEP when suitable generic oral PrEP formulations are available as daily or event-based dosing [64].
Clinical research examining behavioral interventions to optimize the PrEP care continuum for SMM who use substances has focused mostly on formative and pilot projects to guide the development of interventions [65,66,67,68]. However, several randomized controlled trials are underway. These trials are largely focused on adapting and testing evidence-based behavioral approaches, such as CM, MI, and cognitive-behavioral interventions that have previously demonstrated efficacy in reducing substance use and CAS among SMM [59,60,61].
CM targets extrinsic motivation by providing tangible incentives as positive reinforcement for performing health behaviors [69], and it has also been successfully utilized to promote HIV-related health behavior change in people who use substances [70,71,72,73,74,75]. CM for stimulant abstinence has demonstrated some benefits for supporting PEP course completion by SMM [76], and ongoing trials are examining the benefits of CM for facilitating (re-)entry into the PrEP care continuum [77], as well as improving PrEP adherence of SMM who inject methamphetamine [78]. Although CM can achieve moderate, short-term reductions in stimulant use [69], there are enduring concerns about the durability of behavior change following the termination of tangible incentives [79]. In our recently completed trial, we observed that delivering a five-session positive affect intervention during CM for stimulant abstinence achieved durable and clinically meaningful reductions in viral load among SMM living with HIV who use methamphetamine [80]. An ongoing trial is examining the efficacy of this positive affect intervention for boosting and extending the benefits of CM for PrEP adherence by SMM who use stimulants [81].
MI is an evidence-based counseling intervention targeting intrinsic motivation for health behavior change that generally yields small but durable improvements in outcomes [79]. Consistent with MI, one recent pilot randomized controlled trial in the STI clinic setting demonstrated the preliminary efficacy of a two-session motivational enhancement and problem-focused intervention compared to treatment as usual for PrEP-naive SMM [82]. Although most men enrolled in this trial reported substance use in the past 12 months, there is a clear need for ongoing trials by our team and others to test MI interventions targeting PrEP use in the context of ongoing SDU and CAS [77, 83, 84].
Cognitive-behavioral interventions are evidence-based approaches to improving adherence in people living with HIV [85]. One pilot randomized controlled trial provided support for the feasibility and acceptability of a six-session, cognitive-behavioral Life-Steps intervention for PrEP adherence [86]. An ongoing trial is testing the efficacy of a stepped care intervention with two-way text messaging in improving PrEP adherence in SMM with one or more syndemic conditions (including stimulant use) [87]. Among participants randomized to the intervention condition, those who do not display improved PrEP adherence in response to text messages will receive the Life-Steps intervention.
Where are Interventions to Optimize the PrEP Care Continuum Needed in Substance-Using SMM?
Despite the ongoing efforts to develop, test, and implement behavioral interventions to maximize the clinical and public health benefits of PrEP for SMM who use substances, there are fundamental gaps in our understanding of whether and how distinct typologies of SDU and other substance use are linked to difficulties in navigating the PrEP care continuum. SDU broadly encompasses various classes of substances, such as stimulants (e.g., mephedrone, methamphetamine, powder cocaine), poppers, GHB, and erectile dysfunction drugs that are generally used for sexual enhancement motives [41]. SMM also display substantial heterogeneity in their patterns of SDU, ranging from recreational, binge, or episodic use to symptoms consistent with substance use disorders. In this evidence-based review, we had two primary objectives. First, we sought to enumerate studies examining the associations of substance use with the PrEP care continuum: awareness/willingness, use, adherence, and persistence (including retention in care). Second, we evaluated the state of the evidence for the associations of substance use with PrEP use, adherence, and persistence (including retention in care) among SMM. We hypothesized that stimulant use would be more reliably associated with lower PrEP adherence and persistence across studies.
Methods
We performed a systematic review of the associations of stimulant use with the PrEP care continuum. The search strategy was developed by an academic health science librarian (J.R.) in consultation with the rest of the research team and was reviewed by a medical librarian (see the “Acknowledgments” section) using the Peer Review for Electronic Search Strategies (PRESS) tool [88]. The search strategy was written for Ovid Medline and translated using each database’s syntax, controlled vocabulary, and search fields. MeSH terms, EMTREE, CINAHL, and other subject terms, as well as text words, were used for the concepts of preexposure prophylaxis, PrEP medications, stimulants, substance abuse, drug-related behaviors, and their synonyms. We searched Ovid Medline (including Epub-Ahead-of-Print, In-Process & Other Non-Indexed Citations, and Daily, 1946–present), Embase (Elsevier, Embase.com, 1947–present), Cochrane CENTRAL (Cochrane Library, Wiley, earliest to present), CINAHL with Full Text (Ebsco, 1937–present), Scopus (Elsevier, 1823–present), and the Web of Science platform (Clarivate: Science Citation Index Expanded, Social Sciences Citation Index, Arts & Humanities Citation Index, Conference Proceedings Citation Index-Science, Conference Proceedings Citation Index-Social Science & Humanities, Emerging Sources Citation Index, KCI-Korean Journal Database, Russian Science Citation Index, SciELO Citation Index, BIOSIS, and Zoological Abstracts). No language, date, or other limits were applied at the search phase. The primary search strategy was adapted for other databases in part with the use of the Institute for Evidence Based Healthcare’s Polyglot Search translator [89]. All databases were searched on October 6, 2020 and updated using the same strategies on January 27, 2022. All database records were uploaded to Covidence web-based software for deduplication, screening, and full-text evaluation. We contacted the authors of published abstracts for additional data. One member of our research team (J.R.) checked the Retraction Watch database through EndNote citation management software [90] for retractions of the included studies.
Results
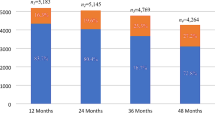
As of January 27, 2022, we identified a total of 4027 articles through our database search after deduplication. Of these, 2397 articles were excluded because (1) the studies did not examine outcomes relevant to the PrEP care continuum, (2) most participants of the studies were not SMM, and (3) the studies did not examine associations of substance use with any indicators of the PrEP care continuum. This resulted in 552 full-text articles that were reviewed by three members of our research team (M.V., D.G., and A.W.C.). Of these full-text articles, 78 were included in our review. As shown in Fig. 1, these studies examined the associations of substance use with 94 outcomes relevant to the PrEP care continuum: awareness/willingness (30), PrEP use (30), PrEP adherence (23), and PrEP persistence (including retention in care, 11).
Thirty studies examined associations of substance use with PrEP use. As shown in Table 1, 18 of these studies (60%) found that SMM who used substances were more likely to use PrEP. Most studies were cross-sectional (n = 18), 14 were conducted exclusively in the USA, and none included biomarker confirmation of PrEP use. The findings generally indicated that SMM who used stimulants, such as methamphetamine, and those who engaged in chemsex drug use were more likely to use PrEP. There was also some mixed evidence regarding whether men who used poppers were more likely to use PrEP.
Thirty-three studies examined the associations of substance use with PrEP adherence or persistence (see Table 2). Approximately half (n = 16) were conducted exclusively in the USA. Demonstration projects or clinic-based cohorts were the most common designs (n = 18). Although 12 studies included biomarkers of PrEP adherence (most commonly tenofovir-diphosphate), only 4 included biomarkers of alcohol or substance use. There were 18 studies that examined associations of stimulants, chemsex drug use, or club drug use with PrEP adherence. More than two-thirds of these studies (n = 13) found that stimulants, chemsex drugs, or club drug use were associated with lower PrEP adherence. In contrast, three studies documented associations of stimulant use or chemsex drug use with better PrEP adherence, particularly in the context of recent CAS. There was no evidence that cannabis use was associated with lower PrEP adherence. Stimulant use, cannabis use, and substance use were associated with decreased PrEP persistence (including retention in PrEP care) in 5 of the 11 studies. One study showed that SMM with an alcohol use disorder had lower odds of PrEP persistence.
Conclusions
In this systematic review, we identified 78 published research articles examining the associations of substance use with indicators of the PrEP care continuum among SMM. Based on this review, we draw three main conclusions. First, SMM who use substances are as likely and, in some instances, more likely to take PrEP, indicating that this high-priority population does not experience substantial barriers to accessing PrEP care. Second, SMM who use stimulants, chemsex drugs, or club drugs can experience greater difficulties with daily oral PrEP adherence; however, some evidence shows that SMM who use stimulants or chemsex drugs may achieve better PrEP adherence in the context of recent CAS. Third, SMM who use substances may be at greater risk of dropping out of PrEP care or discontinuing PrEP. These findings collectively underscore that SMM who use stimulants and other substances may be “running with scissors” along the PrEP care continuum. Although there seems to be no substantial barriers to initiating PrEP, subsequently, an increased risk of difficulties with adherence and persistence could compromise the benefits of PrEP and increase HIV risk. Taken together, SMM who use stimulants and other substances would benefit from more comprehensive efforts to support PrEP re-uptake, adherence, and persistence, such as implementing evidence-based behavioral interventions, considering the potential benefits of event-based PrEP, and providing access to injectable PrEP.
In contrast to studies conducted predominantly with heterosexual people who inject drugs [91], SMM who use substances do not appear to experience substantial barriers to initiating PrEP. Prevention campaigns targeting SMM have long emphasized the link between the use of methamphetamine or other substances with amplified HIV risk [14, 15]. Among SMM who use substances, PrEP could represent an important harm reduction tool to mitigate the risk of HIV in the context of ongoing SDU and CAS. However, greater recognition of an amplified HIV risk may not be sufficient to mitigate the deleterious associations of substance use with daily oral PrEP adherence and lower PrEP persistence that are observed across studies. Expanded efforts are needed to develop, test, and implement scalable behavioral interventions to support rapid PrEP re-uptake by SMM who use substances.
Our findings have important implications for comprehensive approaches to the improvement of PrEP adherence in SMM who use substances. SMM who use stimulants and club drugs could benefit from behavioral interventions to support their adherence to daily oral PrEP. At the same time, providers should consider the potential benefits of event-based PrEP dosing for SMM who use stimulants and chemsex drugs. Although there is no evidence that SMM who use chemsex drugs display a strong preference for event-based dosing [92], those engaging in episodic or binge patterns of use may be suitable candidates for event-based dosing to improve adherence surrounding CAS episodes. However, SMM who are highly sexually active will likely need daily oral PrEP or injectable PrEP. Further research is needed to guide the implementation of event-based PrEP and injectable PrEP for SMM who use substances.
There is emerging evidence across studies that substance use is linked to difficulties with continued engagement in PrEP care or to lower PrEP persistence among SMM. This underscores the need for behavioral interventions targeting these key behaviors that will remain essential for optimizing HIV prevention efforts among SMM who use substances in the era of injectable PrEP. This is consistent with the longer-term need to support HIV prevention efforts for SMM who use substances. Behavioral interventions for SMM who use substances should focus on re-engagement in PrEP care for those who discontinue PrEP, as well as support for long-term retention in PrEP care and PrEP persistence for those currently taking PrEP.
Transformative HIV prevention approaches for SMM who use substances will require a broader, multi-level framework that delineates intersecting structural, social, psychological, and biological determinants of HIV risk in this high-priority population. It is reductionistic to assume that the observational studies included in this evidence-based review provide evidence for causal, dose–response relationships between substance use and difficulties in navigating the PrEP care continuum. Among SMM, substance use often co-occurs with structural and social determinants of health, such as poverty, housing instability, criminal justice involvement, and intersectional stigma that have important implications for HIV prevention [93]. This is further compounded by multiple, co-occurring syndemic conditions, such as childhood sexual abuse, depression, and sexual compulsivity, which synergistically fuel substance use and HIV risk among SMM [42,43,44,45,46,47, 49,50,51]. These intertwining structural, social, and psychological determinants could modify the associations of substance use with difficulties in navigating the PrEP care continuum and amplify rectal immune dysregulation that would increase biological vulnerability to HIV [24, 25]. There is a clear need for prospective, community-based cohorts to examine multi-level factors that moderate or mediate the associations of substance use with difficulties in navigating the PrEP care continuum and heightened HIV risk. This multi-level approach is urgently needed in response to the resurgent methamphetamine epidemic that is fueling one-third of new HIV infections among SMM [5]. Guiding the implementation of more comprehensive public health approaches to maximize the benefits of PrEP for SMM who use methamphetamine is essential to catalyze the success of the “Prevent Strategy” of Ending the HIV Epidemic Initiative in the USA [94].
It is noteworthy that many of the studies included in this review focused on SMM residing in large urban centers, and there is clear evidence that patterns of SDU can vary substantially by region. Future studies should attempt to characterize geographic hotspots for the intersection of SDU and HIV risk among SMM across the globe to guide the targeted deployment of limited public health resources to optimize the benefits of PrEP in this high-priority population. In particular, research is needed to examine the intersection of SDU and HIV risk among SMM residing outside of major urban centers around the globe to inform the development of scalable, telehealth approaches targeting the intersection of SDU and HIV risk. In the USA, SMM who use methamphetamine remain a high-priority population for the Ending the HIV Epidemic Initiative. Developing broader understanding of multi-level determinants of difficulties in navigating the PrEP care continuum and amplified HIV risk is urgently needed to guide transformative HIV prevention efforts in SMM who use methamphetamine.
The findings from this systematic review should be interpreted in the context of some notable limitations. First, due to the substantial heterogeneity in the measurement of distinct typologies of substance use, we were unable to conduct a meta-analysis. Greater consensus is needed in the measurement of specific classes and patterns of substance use across studies. Future studies should attempt to examine distinct patterns of problematic substance use, such as those consistent with a substance use disorder, to identify the relevant threshold(s) where specific classes of substance use have negative consequences for the PrEP care continuum. Although many studies included biomarkers of PrEP adherence, few had biomarkers of recent substance use. Including biomarkers of PrEP and substance use would enhance the scientific rigor of future studies by mitigating misclassification based on self-report. Furthermore, although tenofovir-diphosphate is a validated biomarker of daily oral PrEP adherence, novel approaches (e.g., digital pills) could assist in objectively measuring event-based PrEP adherence [95]. There were also relatively few studies that employed event-level measurements of substance use, PrEP adherence, and CAS [96, 97]. Further research is needed to integrate ecological momentary assessment to better characterize the event-level associations of substance use, PrEP adherence, and CAS. This is particularly important to demonstrate the clinical relevance of PrEP non-adherence that occurs in the context of ongoing CAS (i.e., HIV acquisition risk). Finally, we recognize that other methods of PrEP delivery, including injectable, may soon enter the market on a large scale. Given the novelty of injectable PrEP when this review was conducted, demonstration projects are clearly needed to determine whether and how difficulties in PrEP persistence among SMM who use substances can be addressed in the delivery of injectable PrEP.
This evidence-based review demonstrated that SMM who use substances access PrEP clinical services but could benefit from tailored interventions to support PrEP re-uptake, as well as PrEP adherence, persistence, and retention in care. Multiple randomized controlled trials are testing the efficacy of adapted behavioral interventions to optimize success of SMM who use substances along the PrEP care continuum, and further research is needed to guide the implementation of behavioral interventions that demonstrate efficacy. Providers should also consider the merits of event-based dosing in improving PrEP adherence in SMM who use stimulants or chemsex drugs, as well as provide SMM who use substances with assistance in accessing injectable PrEP.
References
Donnadieu-Rigole H, Peyriere H, Benyamina A, Karila L. Complications related to sexualized drug use: what can we learn from literature? Front Neurosci. 2020;14:548704.
Guerras JM, Hoyos Miller J, Agusti C, Chanos S, Pichon F, Kuske M, Cigan B, Fuertes R, Stefanescu R, Ooms L, et al. Association of sexualized drug use patterns with HIV/STI transmission risk in an internet sample of men who have sex with men from seven European countries. Arch Sex Behav. 2021;50(2):461–77.
Piyaraj P, van Griensven F, Holtz TH, Mock PA, Varangrat A, Wimonsate W, Thienkrua W, Tongtoyai J, McNamara A, Chonwattana W, et al. The finding of casual sex partners on the internet, methamphetamine use for sexual pleasure, and incidence of HIV infection among men who have sex with men in Bangkok, Thailand: an observational cohort study. Lancet HIV. 2018;5(7):e379–89.
Ostrow DG, Plankey MW, Cox C, Li X, Shoptaw S, Jacobson LP, Stall RC. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J Acquir Immune Defic Syndr. 2009;51(3):349–55.
Grov C, Westmoreland D, Morrison C, Carrico AW, Nash D. The crisis we are not talking about: one-in-three annual HIV seroconversions among sexual and gender minorities were persistent methamphetamine users. J Acquir Immune Defic Syndr. 2020;85(3):272–9.
Prestage G, Jin F, Kippax S, Zablotska I, Imrie J, Grulich A. Use of illicit drugs and erectile dysfunction medications and subsequent HIV infection among gay men in Sydney, Australia. J Sex Med. 2009;6(8):2311–20.
Sewell J, Cambiano V, Speakman A, Lampe FC, Phillips A, Stuart D, Gilson R, Asboe D, Nwokolo N, Clarke A, et al. Changes in chemsex and sexual behaviour over time, among a cohort of MSM in London and Brighton: findings from the AURAH2 study. Int J Drug Policy. 2019;68:54–61.
Coyer L, Boyd A, Davidovich U, van Bilsen WPH, Prins M, Matser A. Increase in recreational drug use between 2008 and 2018: results from a prospective cohort study among HIV-negative men who have sex with men. Addiction. 2022;117(3):656–65.
Achterbergh RCA, de Vries HJC, Boyd A, Davidovich U, Druckler S, Hoornenborg E, Prins M, Matser A. Identification and characterization of latent classes based on drug use among men who have sex with men at risk of sexually transmitted infections in Amsterdam, the Netherlands. Addiction. 2020;115(1):121–33.
Hoenigl M, Chaillon A, Moore DJ, Morris SR, Smith DM, Little SJ. Clear links between starting methamphetamine and increasing sexual risk behavior: a cohort study among men who have sex with men. J Acquir Immune Deficiency Syndr. 2016;71(5):551.
Rivera AV, Harriman G, Carrillo SA, Braunstein SL. Trends in methamphetamine use among men who have sex with men in New York City, 2004–2017. AIDS Behav. 2021;25(4):1210–8.
Carrico AW, Storholm ED, Flentje A, Arnold EA, Pollack LM, Neilands TB, Rebchook GM, Peterson JL, Eke A, Johnson W, et al. Spirituality/religiosity, substance use, and HIV testing among young black men who have sex with men. Drug Alcohol Depend. 2017;174:106–12.
Martino RJ, Shiau S, Krause KD, Halkitis PN. Event-level patterns of methamphetamine and poly-drug use among millennial sexual minority men: the P18 Cohort Study. Addict Behav. 2021;117:106831.
Pantalone DW, Bimbi DS, Holder CA, Golub SA, Parsons JT. Consistency and change in club drug use by sexual minority men in New York City, 2002 to 2007. Am J Public Health. 2010;100:1892–5.
Grov C, Parsons JT, Bimbi DS. In the shadows of a prevention campaign: Sexual risk in the absence of crystal methamphetamine. AIDS Educ Prev. 2008;20:42–55.
Reback CJ, Shoptaw S, Grella CE. Methamphetamine use trends among street-recruited gay and bisexual maleS, from 1999 to 2007. J Urban Health. 2008;85(6):874.
Reback CJ, Fletcher JB, Shoptaw S, Grella CE. Methamphetamine and other substance use trends among street-recruited men who have sex with men, from 2008 to 2011. Drug Alcohol Depend. 2013;133(1):262–5.
Kuo I, Patrick R, Opoku J, Rawls A, Magnus M, Peterson J, Kharfen MAG. Changing pattern of crystal meth use in black & white MSM, Washington, DC, 2008–2014. In: Conference on Retroviruses and Opportunistic Infections: 2017; Seattle, WA; 2017.
Hood JE, Buskin SE, Golden MR, Glick SN, Banta-Green C, Dombrowski JC. The changing burden of HIV attributable to methamphetamine among men who have sex with men in King County, Washington. AIDS Patient Care STDs. 2018;32(6):223–33.
CDC. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 20 U.S. Cities, 2014. In.; 2016.
Pantalone DW, Bimbi DS, Holder CA, Golub SA, Parsons JT. Consistency and change in club drug use by sexual minority men in New York City, 2002 to 2007. Am J Public Health. 2010;100(10):1892–5.
Hammoud MA, Jin F, Maher L, Bourne A, Haire B, Saxton P, Vaccher S, Lea T, Degenhardt L, Prestage G. Biomedical HIV protection among gay and bisexual men who use crystal methamphetamine. AIDS Behav. 2020;24(5):1400–13.
Nerlander LMC, Hoots BE, Bradley H, Broz D, Thorson A, Paz-Bailey G, Group N. HIV infection among MSM who inject methamphetamine in 8 US cities. Drug Alcohol Depend. 2018;190:216–23.
Fulcher JA, Shoptaw S, Makgoeng SB, Elliott J, Ibarrondo FJ, Ragsdale A, Brookmeyer R, Anton PA, Gorbach PM. Brief report: recent methamphetamine use is associated with increased rectal mucosal inflammatory cytokines, regardless of HIV-1 serostatus. J Acquir Immune Defic Syndr. 2018;78(1):119–23.
Tapia GR, Glynn TR, Miller C, Manuzak JA, Broedlow CA, McGaugh A, Cherenack EM, Bauermeister JA, Grov C, Dilworth SE, et al. Syndemics and preexposure prophylaxis are independently associated with rectal immune dysregulation in sexual minority men. AIDS. 2021;35(8):1295–300.
Kelley CF, Kraft CS, de Man TJ, Duphare C, Lee HW, Yang J, Easley KA, Tharp GK, Mulligan MJ, Sullivan PS, et al. The rectal mucosa and condomless receptive anal intercourse in HIV-negative MSM: implications for HIV transmission and prevention. Mucosal Immunol. 2017;10(4):996–1007.
Hladik F, McElrath MJ. Setting the stage: host invasion by HIV. Nat Rev Immunol. 2008;8(6):447–57.
Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–62.
Halkitis PN, Fischgrund BN, Parsons JT. Explanations for methamphetamine use among gay and bisexual men in New York City. Subst Use Misuse. 2005;40(9–10):1331–45.
Braine N, Acker CJ, Van Sluytman L, Friedman S, Jarlais DCD. Drug use, community action, and public health: gay men and crystal meth in NYC. Subst Use Misuse. 2011;46(4):368–80.
Treloar C, Hopwood M, Drysdale K, Lea T, Holt M, Dowsett GW, Aggleton P, Bryant J. Stigma as understood by key informants: a social ecological approach to gay and bisexual men’s use of crystal methamphetamine for sex. Int J Drug Policy. 2021;94:103229.
Aguilar JP, Sen S. The culture of methamphetamine: reframing gay men’s methamphetamine use. J Hum Behav Soc Environ. 2013;23(3):370–82.
Bostwick WB, Boyd CJ, Hughes TL, West B. Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. Am J Orthopsychiatry. 2014;84(1):35–45.
Balaji AB, Bowles KE, Hess KL, Smith JC, Paz-Bailey G, Taussig J, Gern R, Hoyte T, Salazar L, White J, et al. Association between enacted stigma and HIV-related risk behavior among MSM, National HIV Behavioral Surveillance System, 2011. AIDS Behav. 2017;21(1):227–37.
Lee JH, Gamarel KE, Bryant KJ, Zaller ND, Operario D. Discrimination, mental health, and substance use disorders among sexual minority populations. LGBT Health. 2016;3(4):258–65.
Mays VM, Cochran SD. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. Am J Public Health. 2001;91(11):1869–76.
Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: does disadvantaged social statuses confer more stress and fewer coping resources? Soc Sci Med. 2008;67(3):368–79.
Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995;36:38–56.
HIV and all gay and bisexual men. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; 2021 [cited 2022 Jun13]. Available from: https://www.cdc.gov/hiv/group/msm/index.html.
McKirnan DJ, Ostrow DG, Hope B. Sex, drugs and escape: a psychological model of HIV-risk sexual behaviours. AIDS Care. 1996;8(6):655–70.
Bourne A, Weatherburn P. Substance use among men who have sex with men: patterns, motivations, impacts and intervention development need. Sex Transm Infect. 2017;93(5):342–6.
Parsons JT, Millar BM, Moody RL, Starks TJ, Rendina HJ, Grov C. Syndemic conditions and HIV transmission risk behavior among a HIV-negative gay and bisexual men in a U.S. national sample. Health Psychol. 2017;36:695–671.
Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Pollack L, Binson D, Osmond D, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42.
O’Leary A, Jemmott JB III, Stevens R, Rutledge SE, Icard LD. Optimism and education buffer the effects of syndemic conditions on HIV status among African American men who have sex with men. AIDS Behav. 2014;18:2080–8.
Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–7.
van den Berg JJ, Fernández MI, Fava JL, Operario D, Rudy BJ, Wilson PA. Using syndemics theory to investigate risk and protective factors associated with condomless sex amonG youth living with HIV in 17 US cities. AIDS Behav. 2017;21:833–44.
Wim VB, Christiana N, Marie L. Syndemic and other risk factors for unprotected anal Intercourse among an online sample of Belgian HIV negative men who have sex with men. AIDS Behav. 2014;18(1):50–8.
Mimiaga MJ, O’Cleirigh C, Biello KB, Robertson AM, Safren SA, Coates TJ, Koblin BA, Chesney MA, Donnell DJ, Stall RD, et al. The effect of psychosocial syndemic production on 4-year HIV incidence and risk behavior in a large cohort of sexually active men who have sex with men. J Acquir Immune Defic Syndr. 2015;68(3):329–36.
Parsons JT, Rendina HJ, Ventuneac A, Moody RL, Grov C. Syndemic production and sexual compulsivity/hypersexuality in a cohort of highly sexually active gay and bisexual men: further evidence of a three group conceptualization. Arch Sex Behav. 2015;44:1903–13.
Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am J Public Health. 2012;102:156–62.
Woolf-King SE, Rice TM, Truong HM, Woods WJ, Jerome RC, Carrico AW. Substance use and HIV risk behavior among men who have sex with men: the role of sexual compulsivity. J Urban Health. 2013;90(5):948–52.
Rooney BM, Tulloch TG, Blashill AJ. Psychosocial syndemic correlates of sexual compulsivity among men who have sex with men: a meta-analysis. Arch Sex Behav. 2018;47(1):75–93.
Colfax GN, Santos GM, Das M, Santos DM, Matheson T, Gasper J, Shoptaw S, Vittinghoff E. Mirtazapine to reduce methamphetamine use: a randomized controlled trial. Arch Gen Psychiatry. 2011;68(11):1168–75.
Coffin PO, Santos GM, Hern J, Vittinghoff E, Walker JE, Matheson T, Santos D, Colfax G, Batki SL. Effects of mirtazapine for methamphetamine use disorder among cisgender men and transgender women who have sex with men: a placebo-controlled randomized clinical trial. JAMA Psychiatry. 2020;77(3):246–55.
Trivedi MH, Walker R, Ling W, Dela Cruz A, Sharma G, Carmody T, Ghitza UE, Wahle A, Kim M, Shores-Wilson K, et al. Bupropion and naltrexone in methamphetamine use disorder. N Engl J Med. 2021;384(2):140–53.
Chan B, Freeman M, Kondo K, Ayers C, Montgomery J, Paynter R, Kansagara D. Pharmacotherapy for methamphetamine/amphetamine use disorder-a systematic review and meta-analysis. Addiction. 2019;114(12):2122–36.
Chan B, Kondo K, Freeman M, Ayers C, Montgomery J, Kansagara D. Pharmacotherapy for cocaine use disorder-a systematic review and meta-analysis. J Gen Intern Med. 2019;34(12):2858–73.
AshaRani PV, Hombali A, Seow E, Ong WJ, Tan JH, Subramaniam M. Non-pharmacological interventions for methamphetamine use disorder: a systematic review. Drug Alcohol Depend. 2020;212:108060.
Carrico AW, Zepf R, Meanley S, Batchelder A, Stall R. When the party is over: a systematic review of behavioral interventions for substance-using men who have sex with men. J Acquir Immune Defic Syndr. 2016;73:299–302.
Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, Amass L. Contingency management among homeless, out-of-treatment men who have sex with men. J Subst Abuse Treat. 2010;39(3):255–63.
Mimiaga MJ, Pantalone DW, Biello KB, Hughto JMW, Frank J, O’Cleirigh C, Reisner SL, Restar A, Mayer KH, Safren SA. An initial randomized controlled trial of behavioral activation for treatment of concurrent crystal methamphetamine dependence and sexual risk for HIV acquisition among men who have sex with men. AIDS Care. 2019;31(9):1083–95.
Oldenburg CE, Jain S, Mayer KH, Mimiaga MJ. Post-exposure prophylaxis use and recurrent exposure to HIV among men who have sex with men who use crystal methamphetamine. Drug Alcohol Depend. 2015;146:75–80.
Landovitz RJ, Donnell D, Clement ME, Hanscom B, Cottle L, Coelho L, Cabello R, Chariyalertsak S, Dunne EF, Frank I, et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385(7):595–608.
Buchbinder SP. Maximizing the benefits of HIV preexposure prophylaxis. Top Antivir Med. 2018;25(4):138–42.
McMahan VM, Frank N, Buckler S, Violette LR, Baeten JM, Banta-Green CJ, Barnabas RV, Simoni J, Stekler JD. Protocol development for HMU! (HIV prevention for methamphetamine users), a study of peer navigation and text messaging to promote pre-exposure prophylaxis adherence and persistence among people who use methamphetamine: qualitative focus group and interview study. JMIR Form Res. 2020;4(9):e18118.
McMahan VM, Martin A, Garske L, Violette LR, Andrasik MP, Baeten JM, Banta-Green C, Stekler JD. Development of a targeted educational intervention to increase pre-exposure prophylaxis uptake among cisgender men and transgender individuals who have sex with men and use methamphetamine in Seattle (WA, USA). Sex Health. 2019;16(2):139–47.
Reback CJ, Clark KA, Runger D, Fehrenbacher AE. A promising PrEP navigation intervention for transgender women and men who have sex with men experiencing multiple syndemic health disparities. J Community Health. 2019;44(6):1193–203.
Closson EF, Mitty JA, Malone J, Mayer KH, Mimiaga MJ. Exploring strategies for PrEP adherence and dosing preferences in the context of sexualized recreational drug use among MSM: a qualitative study. AIDS Care. 2018;30(2):191–8.
Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101(11):1546–60.
Haug NA, Sorensen JL. Contingency management interventions for HIV-related behaviors. Curr HIV/AIDS Rep. 2006;3(4):154–9.
Sorensen JL, Haug NA, Delucchi KL, Gruber V, Kletter E, Batki SL, Tulsky JP, Barnett P, Hall S. Voucher reinforcement improves medication adherence in HIV-positive methadone patients: a randomized trial. Drug Alcohol Depend. 2007;88(1):54–63.
Petry NM, Weinstock J, Alessi SM, Lewis MW, Dieckhaus K. Group-based randomized trial of contingencies for health and abstinence in HIV patients. J Consult Clin Psychol. 2010;78(1):89–97.
Metsch LR, Feaster DJ, Gooden L, Matheson T, Stitzer M, Das M, Jain MK, Rodriguez AE, Armstrong WS, Lucas GM, et al. Effect of patient navigation with or without financial incentives on viral suppression among hospitalized patients with HIV infection and substance use: a randomized clinical trial. JAMA. 2016;316(2):156–70.
Carrico AW, Neilands TB, Dilworth SE, Evans JL, Gomicronmez W, Jain JP, Gandhi M, Shoptaw S, Horvath KJ, Coffin L, et al. Randomized controlled trial of a positive affect intervention to reduce HIV viral load among sexual minority men who use methamphetamine. J Int AIDS Soc. 2019;22(12):e25436.
Stoner MCD, Kilburn K, Godfrey-Faussett P, Ghys P, Pettifor AE. Cash transfers for HIV prevention: a systematic review. PLoS Med. 2021;18(11):e1003866.
Landovitz RJ, Fletcher JB, Shoptaw S, Reback CJ. Contingency management facilitates the use of postexposure prophylaxis among stimulant-using men who have sex with men. Open Forum Infect Dis. 2015;2(1):ofu114.
PrEP Readiness Interventions for Supporting Motivation (PRISM) [cited 2022 Jun 13]. Available from: https://clinicaltrials.gov/ct2/show/NCT04205487.
PrEP Intervention for People Who Inject Substances and Use Methamphetamine [cited 2022 Jun 13]. Available from: https://clinicaltrials.gov/ct2/show/NCT04523519
Sayegh CS, Huey SJ, Zara EJ, Jhaveri K. Follow-up treatment effects of contingency management and motivational interviewing on substance use: a meta-analysis. Psychol Addict Behav. 2017;31:403–10.
Carrico AW, Neilands TB, Dilworth SE, Evans JL, Gomez W, Jain J, Gandhi M, Shoptaw S, Horvath KJ, Coffin L, et al. Randomized controlled trial of a positive affect intervention to reduce viral load in methamphetamine-using sexual minority men. In: International AIDS Society Conference on HIV Science Mexico City, Mexico; 2019.
PrEP Affect Regulation Treatment Innovation [cited 2022 Jun 13]. Available from: https://clinicaltrials.gov/ct2/show/NCT04899024
Chan PA, Nunn A, van den Berg JJ, Cormier K, Sowemimo-Coker G, Napoleon SC, Arnold T, Moitra E. A randomized trial of a brief behavioral intervention for PrEP uptake among men who have sex with men at increased risk for HIV infection. J Acquir Immune Defic Syndr. 2021;87(3):937–43.
Parsons JT, Starks T, Gurung S, Cain D, Marmo J, Naar S. Clinic-based delivery of the Young Men’s Health Project (YMHP) targeting HIV risk reduction and substance use among young men who have sex with men: protocol for a type 2, hybrid implementation-effectiveness trial. JMIR Res Protoc. 2019;8(5):e11184.
Starks TJ, Robles G, Pawson M, Jimenez RH, Gandhi M, Parsons JT, Millar BM. Motivational interviewing to reduce drug use and HIV incidence among young men who have sex with men in relationships and are high priority for pre-exposure prophylaxis (Project PARTNER): randomized controlled trial protocol. JMIR Res Protoc. 2019;8(7):e13015.
Safren SA, Otto MW, Worth JL. Life-steps: applying cognitive behavioral therapy to HIV medication adherence. Cogn Behav Pract. 1999;6(4):332–41.
Mayer KH, Safren SA, Elsesser SA, Psaros C, Tinsley JP, Marzinke M, Clarke W, Hendrix C, Wade Taylor S, Haberer J, et al. Optimizing pre-exposure antiretroviral prophylaxis adherence in men who have sex with men: results of a pilot randomized controlled trial of “Life-Steps for PrEP.” AIDS Behav. 2017;21(5):1350–60.
Safren S. Life-steps counseling to enhance adherence and engagement in PrEP care. 2022.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6.
Clark JM, Sanders S, Carter M, Honeyman D, Cleo G, Auld Y, Booth D, Condron P, Dalais C, Bateup S, et al. Improving the translation of search strategies using the Polyglot Search Translator: a randomized controlled trial. J Med Libr Assoc. 2020;108(2):195–207.
The EndNote Team: EndNote. In., Version: EndNote 20 edn. Philadelphia, PA: Clarivate; 2021.
Mistler CB, Copenhaver MM, Shrestha R. The pre-exposure prophylaxis (PrEP) care cascade in people who inject drugs: a systematic review. AIDS Behav. 2021;25(5):1490–506.
Hoornenborg E, Achterbergh RC, van der Loeff MFS, Davidovich U, van der Helm JJ, Hogewoning A, van Duijnhoven YT, Sonder GJ, de Vries HJ, Prins M, et al. Men who have sex with men more often chose daily than event-driven use of pre-exposure prophylaxis: baseline analysis of a demonstration study in Amsterdam. J Int AIDS Soc. 2018;21(3):e25105.
Shoptaw S, Montgomery B, Williams CT, El-Bassel N, Aramrattana A, Metsch L, Metzger DS, Kuo I, Bastos FI, Strathdee SA. Not just the needle: the state of HIV-prevention science among substance users and future directions. J Acquir Immune Defic Syndr. 2013;63 Suppl 2:S174-178.
Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–5.
Chai PR, Mohamed Y, Bustamante MJ, Goodman GR, Najarro J, Castillo-Mancilla J, Baez A, Bronzi O, Sullivan MC, Pereira LM, et al. DigiPrEP: a pilot trial to evaluate the feasibility, acceptability, and accuracy of a digital pill system to measure PrEP adherence in men who have sex with men who use substances. J Acquir Immune Defic Syndr. 2022;89(2):e5–15.
Grov C, Rendina HJ, John SA, Parsons JT. Determining the roles that club drugs, marijuana, and heavy drinking play in PrEP medication adherence among gay and bisexual men: implications for treatment and research. AIDS Behav. 2019;23(5):1277–86.
Wray TB, Chan PA, Kahler CW, Simpanen EM, Liu T, Mayer KH. Vulnerable periods: characterizing patterns of sexual risk and substance use during lapses in adherence to HIV pre-exposure prophylaxis among men who have sex with men. J Acquir Immune Defic Syndr. 2019;80(3):276–83.
Blair KJ, Segura ER, Garner A, Lai J, Ritterbusch A, Leon-Giraldo S, Guilamo-Ramos V, Lake JE, Clark J, Holloway IW. PrEP awareness, use, intention to use, and information source among geosocial networking application users in Mexico in 2018–2019. AIDS Behav. 2021;25(9):2743–54.
Eaton LA, Matthews DD, Bukowski LA, Friedman MR, Chandler CJ, Whitfield DL, Sang JM, Stall RD, Team PS. Elevated HIV prevalence and correlates of PrEP use among a community sample of black men who have sex with men. J Acquir Immune Defic Syndr. 2018;79(3):339–46.
Feldman MB, Kepler KL, Montero N, Hoffman S, Irvine MK. Pre-exposure prophylaxis use among crystal methamphetamine-usinG MSM who receive community-based harm reduction services in New York City: a retrospective chart review. J Assoc Nurses AIDS Care. 2020;31(6):701–9.
Flores Anato JL, Panagiotoglou D, Greenwald ZR, Trottier C, Vaziri M, Thomas R, Maheu-Giroux M. Chemsex practices and pre-exposure prophylaxis (PrEP) trajectories among individuals consulting for PrEP at a large sexual health clinic in Montreal, Canada (2013–2020). Drug Alcohol Depend. 2021;226:108875.
Hambrick HR, Park SH, Schneider JA, Mayer KH, Carrico AW, Sherman SE, Duncan DT. Poppers and PrEP: use of pre-exposure prophylaxis among men who have sex with men who use inhaled nitrites. AIDS Behav. 2018;22(11):3658–72.
Hammoud MA, Vaccher S, Jin F, Bourne A, Maher L, Holt M, Bavinton BR, Haire B, Degenhardt L, Grulich A, et al. HIV pre-exposure prophylaxis (PrEP) uptake among gay and bisexual men in Australia and factors associated with the nonuse of PrEP among eligible men: results from a prospective cohort study. J Acquir Immune Defic Syndr. 2019;81(3):e73–84.
Hanum N, Cambiano V, Sewell J, Phillips AN, Rodger AJ, Speakman A, Nwokolo N, Asboe D, Gilson R, Clarke A, et al. Use of HIV pre-exposure prophylaxis among men who have sex with men in England: data from the AURAH2 prospective study. Lancet Public Health. 2020;5(9):e501–11.
Hardy C, Fairley CK, Ong JJ, et al. Drug and Alcohol Use with Condomless Anal Sex among Men Who Have Sex with Men in Melbourne, Australia: A Retrospective Data Analysis from 2011 to 2017. Arch Sex Behav. 2021. https://doi.org/10.1007/s10508-021-01966-1.
Hibbert MP, Brett CE, Porcellato LA, Hope VD. Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sex Transm Infect. 2019;95(5):342–50.
Holloway IW, Dougherty R, Gildner J, Beougher SC, Pulsipher C, Montoya JA, Plant A, Leibowitz A. Brief report: PrEP uptake, adherence, and discontinuation among California YMSM using geosocial networking applications. J Acquir Immune Defic Syndr. 2017;74(1):15–20.
Hulstein SH, Matser A, van der Loeff MFS, Hoornenborg E, Prins M, de Vries HJC. Eligibility for HIV preexposure prophylaxis, intention to use preexposure prophylaxis, and informal use of preexposure prophylaxis among men who have sex with men in Amsterdam, the Netherlands. Sex Transm Dis. 2021;48(2):86–93.
Khaw C, Zablotska-Manos I, Boyd MA. Men who have sex with men and chemsex: a clinic-based cross-sectional study in South Australia. Sex Res Soc Policy. 2021;18:1014–22.
Kota KK, Mansergh G, Stephenson R, Hirshfield S, Sullivan P. Sociodemographic characteristics of HIV pre-exposure prophylaxis use and reasons for nonuse among gay, bisexual, and other men who have sex with men from three US cities. AIDS Patient Care STDS. 2021;35(5):158–66.
Maksut JL, Gicquelais RE, Jackman KM, Eaton LA, Friedman MR, Matthews DD, Bukowski LA, Stall RD. Injection drug use, unknown HIV positive status, and self-reported current PrEP use among Black men who have sex with men attending U.S. Black pride events, 2014–2017. Drug Alcohol Depend. 2020;207:107808.
Mansergh G, Stephenson R, Hirshfield S, Sullivan P. Understanding HIV sexual protection and its association with substance use during sex among MSM in an era of multiple primary prevention products. J Acquir Immune Defic Syndr. 2020;85(4):e67.
Maxwell S, Gafos M, Moncrieff M, Shahmanesh M, Stirrup O. Pre-exposure prophylaxis use among men who have sex with men who have experienced problematic chemsex. Int J STD AIDS. 2020;31(5):474–80.
Morgan E, Moran K, Ryan DT, Mustanski B, Newcomb ME. Threefold increase in PrEP uptake over time with high adherence among young men who have sex with men in Chicago. AIDS Behav. 2018;22(11):3637–44.
Onwubiko U, Holland D, Ajoku S, Taylor J, Childs A, Wilson D, Chamberlain AT. Using PrEP to #STOPHIVATL: findings from a cross-sectional survey among gay men and transgender women participating in gay pride events in Atlanta, Georgia, 2018. Arch Sex Behav. 2020;49(6):2193–204.
Okafor CN, Gorbach PM, Ragsdale A, Quinn B, Shoptaw S. Correlates of preexposure prophylaxis (PrEP) use among men who have sex with men (MSM) in Los Angeles, California. J Urban Health. 2017;94(5):710–5.
Okafor CN, Hucks-Ortiz C, Hightow-Weidman LB, Magnus M, Emel L, Beauchamp G, Kuo I, Hendrix C, Mayer KH, Shoptaw SJ. Brief report: associations between self-reported substance use behaviors and PrEP acceptance and adherence among black MSM in the HPTN 073 study. J Acquir Immune Defic Syndr. 2020;85(1):23–9.
Plotzker R, Seekaew P, Jantarapakde J, Pengnonyang S, Trachunthong D, Linjongrat D, Janyam S, Nakpor T, Charoenying S, Mills S, et al. Importance of risk perception: predictors of PrEP acceptance among Thai MSM and TG women at a community-based health service. J Acquir Immune Defic Syndr. 2017;76(5):473–81.
Ramautarsing RA, Meksena R, Sungsing T, Chinbunchorn T, Sangprasert T, Fungfoosri O, Meekrua D, Sumalu S, Pasansai T, Bunainso W, et al. Evaluation of a pre-exposure prophylaxis programme for men who have sex with men and transgender women in Thailand: learning through the HIV prevention cascade lens. J Int AIDS Soc. 2020;23 Suppl 3:e25540.
Serota DP, Rosenberg ES, Sullivan PS, Thorne AL, Rolle CM, Del Rio C, Cutro S, Luisi N, Siegler AJ, Sanchez TH, et al. Pre-exposure prophylaxis uptake and discontinuation among young black men who have sex with men in Atlanta, Georgia: A Prospective Cohort Study. Clin Infect Dis. 2020;71(3):574–82.
Schecke H, Lea T, Bohn A, Kohler T, Sander D, Scherbaum N, Deimel D. Crystal methamphetamine use in sexual settings among German men who have sex with men. Front Psychiatry. 2019;10:886.
Shover CL, Javanbakht M, Shoptaw S, Bolan RK, Lee SJ, Parsons JT, Rendina J, Gorbach PM. HIV preexposure prophylaxis initiation at a large community clinic: differences between eligibility, awareness, and uptake. Am J Public Health. 2018;108(10):1408–17.
Wheeler DP, Fields SD, Beauchamp G, Chen YQ, Emel LM, Hightow-Weidman L, Hucks-Ortiz C, Kuo I, Lucas J, Magnus M, et al. Pre-exposure prophylaxis initiation and adherence among Black men who have sex with men (MSM) in three US cities: results from the HPTN 073 study. J Int AIDS Soc. 2019;22(2):e25223.
Whitfield THF, Parsons JT, Rendina HJ. Rates of pre-exposure prophylaxis use and discontinuation among a large U.S. national sample of sexual minority men and adolescents. Arch Sex Behav. 2020;49(1):103–12.
Wong NS, Kwan TH, Lee KCK, Lau JYC, Lee SS. Delineation of chemsex patterns of men who have sex with men in association with their sexual networks and linkage to HIV prevention. Int J Drug Policy. 2020;75:102591.
Coyer L, van den Elshout MAM, Achterbergh RCA, Matser A, Schim van der Loeff MF, Davidovich U, de Vries HJC, Prins M, Hoornenborg E, Boyd A, et al. Understanding pre-exposure prophylaxis (PrEP) regimen use: switching and discontinuing daily and event-driven PrEP among men who have sex with men. EClinicalMedicine. 2020;29–30:100650.
De Franca FAP, Barros De, SIlva PG, De Franca Fonteles MM. The impact of alcohol and Illicit drug use on adherence to HIV pre-exposure prophylaxis among men who have sex with men. J Young Pharmacists. 2021;13(3):251–6.
Goodman-Meza D, Beymer MR, Kofron RM, Amico KR, Psaros C, Bushman LR, Anderson PL, Bolan R, Jordan WC, Rooney JF, et al. Effective use of pre-exposure prophylaxis (PrEP) among stimulant users with multiple condomless sex partners: a longitudinal study of men who have sex with men in Los Angeles. AIDS Care. 2019;31(10):1228–33.
Grinsztejn B, Hoagland B, Moreira RI, Kallas EG, Madruga JV, Goulart S, Leite IC, Freitas L, Martins LMS, Torres TS, et al. Retention, engagement, and adherence to pre-exposure prophylaxis for men who have sex with men and transgender women in PrEP Brasil: 48 week results of a demonstration study. Lancet HIV. 2018;5(3):e136–45.
Hoenigl M, Jain S, Moore D, Collins D, Sun X, Anderson PL, Corado K, Blumenthal JS, Daar ES, Milam J, Dubé MP. Substance use and adherence to HIV preexposure prophylaxis for men who have sex with men. Emerging infectious diseases. 2018;24(12):2292–302.
Hoenigl M, Hassan A, Moore DJ, Anderson PL, Corado K, Dube MP, Ellorin EE, Blumenthal J, Morris SR. California Collaborative Treatment Group T: Predictors of long-term HIV pre-exposure prophylaxis adherence after study participation in men who have sex with men. J Acquir Immune Defic Syndr. 2019;81(2):166–74.
Hoagland B, Moreira RI, De Boni RB, Kallas EG, Madruga JV, Vasconcelos R, Goulart S, Torres TS, Marins LMS, Anderson PL, et al. High pre-exposure prophylaxis uptake and early adherence among men who have sex with men and transgender women at risk for HIV Infection: the PrEP Brasil demonstration project. J Int AIDS Soc. 2017;20(1):21472.
Hojilla JC, Vlahov D, Crouch PC, Dawson-Rose C, Freeborn K, Carrico A. HIV pre-exposure prophylaxis (PrEP) uptake and retention among men who have sex with men in a community-based sexual health clinic. AIDS Behav. 2018;22(4):1096–9.
Hojilla JC, Vlahov D, Glidden DV, Amico KR, Mehrotra M, Hance R, Grant RM, Carrico AW. Skating on thin ice: stimulant use and sub-optimal adherence to HIV pre-exposure prophylaxis. J Int AIDS Soc. 2018;21(3):e25103.
Hojilla JC, Satre DD, Glidden DV, McMahan VM, Gandhi M, Defechereux P, Guanira JV, Mehrotra M, Grant RM, Carrico AW. Cocaine use and pre-exposure prophylaxis: adherence, care engagement, and kidney function. J Acquir Immune Defic Syndr. 2019;81:78–82.
Holtz TH, Chitwarakorn A, Hughes JP, Curlin ME, Varangrat A, Li M, Amico KR, Mock PA, Grant RM, Thai HAST. HPTN 067/ADAPT: correlates of sex-related pre-exposure prophylaxis adherence, Thai men who have sex with men, and transgender women, 2012–2013. J Acquir Immune Defic Syndr. 2019;82(2):e18–26.
Jin F, Amin J, Guy R, Vaccher S, Selvey C, Zablotska I, Holden J, Price K, Yeung B, Ogilvie E, et al. Adherence to daily HIV pre-exposure prophylaxis in a large-scale implementation study in New South Wales, Australia. AIDS. 2021;35(12):1987–96.
Krakower D, Maloney KM, Powell VE, Levine K, Grasso C, Melbourne K, Marcus JL, Mayer KH. Patterns and clinical consequences of discontinuing HIV preexposure prophylaxis during primary care. J Int AIDS Soc. 2019;22(2):e25250.
Monteiro Spindola Marins L, Silva Torres T, Luz PM, Moreira RI, Leite IC, Hoagland B, Kallas EG, Madruga JV, Grinsztejn B, Veloso VG, et al. Factors associated with self-reported adherence to daily oral pre-exposure prophylaxis among men who have sex with man and transgender women: PrEP Brasil study. Int J STD AIDS. 2021;32(13):1231–41.
Mounzer K, Petroll A, Carter C, Johnson B, Binford M, Mayer G, Dbrahimi R, Shao Y, Thrun M, Das M. Substance use was common in persons at-risk for and diagnosed with HIV in a trial of F/TAF for PrEP (DISCOVER). Sex Transm Dis. 2020;47:S86-87.
Mugo PM, Sanders EJ, Mutua G, van der Elst E, Anzala O, Barin B, Bangsberg DR, Priddy FH, Haberer JE. Understanding adherence to daily and intermittent regimens of oral HIV pre-exposure prophylaxis among men who have sex with men in Kenya. AIDS Behav. 2015;19(5):794–801.
Myers JJ, Kang Dufour MS, Koester KA, Udoh I, Frazier R, Packard R, Kennedy K, Erguera X, Horowitz J, Grant R, et al. Adherence to PrEP among young men who have sex with men participating in a sexual health services demonstration project in Alameda County, California. J Acquir Immune Defic Syndr. 2019;81(4):406–13.
O’Halloran C, Rice B, White E, Desai M, Dunn DT, McCormack S, Sullivan AK, White D, McOwan A, Gafos M. Chemsex is not a barrier to self-reported daily PrEP adherence among PROUD study participants. Int J Drug Policy. 2019;74:246–54.
Roux P, Fressard L, Suzan-Monti M, Chas J, Sagaon-Teyssier L, Capitant C, Meyer L, Tremblay C, Rojas-Castro D, Pialoux G, et al. Is on-demand HIV Pre-exposure prophylaxis a suitable tool for men who have sex with men who practice chemsex? Results from a substudy of the ANRS-IPERGAY Trial. J Acquir Immune Defic Syndr. 2018;79(2):e69–75.
Scott HM, Spinelli M, Vittinghoff E, Morehead-Gee A, Hirozawa A, James C, Hammer H, Liu A, Gandhi M, Buchbinder S. Racial/ethnic and HIV risk category disparities in preexposure prophylaxis discontinuation among patients in publicly funded primary care clinics. AIDS. 2019;33(14):2189–95.
Shuper PA, Joharchi N, Bogoch II, Loutfy M, Crouzat F, El-Helou P, Knox DC, Woodward K, Rehm J. Alcohol consumption, substance use, and depression in relation to HIV pre-exposure prophylaxis (PrEP) nonadherence among gay, bisexual, and other men-who-have-sex-with-men. BMC Public Health. 2020;20(1):1782.
Spinelli MA, Scott HM, Vittinghoff E, Liu AY, Gonzalez R, Morehead-Gee A, Gandhi M, Buchbinder SP. Missed visits associated with future preexposure prophylaxis (PrEP) discontinuation among PrEP users in a municipal primary care health network. Open Forum Infect Dis. 2019;6(4):ofz101.
Tao J, Montgomery MC, Williams R, Patil P, Rogers BG, Sosnowy C, Murphy M, Zanowick-Marr A, Maynard M, Napoleon SC, et al. Loss to follow-up and re-engagement in HIV pre-exposure prophylaxis care in the United States, 2013–2019. AIDS Patient Care STDS. 2021;35(7):271–7.
Vuylsteke B, Reyniers T, Nostlinger C, Smekens T, Kenyon C, Laga M. Can we predict incorrect PrEP use in high HIV risk situations among men who have sex with men? An analysis of Be-PrEP-ared, the Belgian PrEP demonstration study. J Acquir Immune Defic Syndr. 2021;88(1):36–44.
Wu HJ, Wen-Wei KuS, Chang HH, Li CW, Ko NY, Strong C. Imperfect adherence in real life: a prevention-effective perspective on adherence to daily and event-driven HIV pre-exposure prophylaxis among men who have sex with men - a prospective cohort study in Taiwan. J Int AIDS Soc. 2021;24(5):e25733.
Zucker J, Carnevale C, Richards P, Slowikowski J, Borsa A, Gottlieb F, Vakkur I, Hyden C, Olender S, Cohall A, et al. Predictors of disengagement in care for individuals receiving pre-exposure prophylaxis (PrEP). J Acquir Immune Defic Syndr. 2019;81(4):e104–8.
Acknowledgements
The authors thank Tara Brigham, MLIS, from the Mayo Clinic Libraries in Jacksonville, FL, for the peer review of the Medline database search strategy.
Funding
This work was supported by the National Institute on Drug Abuse (R34-DA046367; R01-051848) and the National Institute for Allergy and Infectious Diseases (UG3-AI169652). Additional support for this project was provided by the Miami Center for AIDS Research (P30-AI073961; Pahwa, PI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
Because this review focused only on published studies, there were no human subjects, and this project was exempt.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Behavioral-Bio-Medical Interface
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Viamonte, M., Ghanooni, D., Reynolds, J.M. et al. Running with Scissors: a Systematic Review of Substance Use and the Pre-exposure Prophylaxis Care Continuum Among Sexual Minority Men. Curr HIV/AIDS Rep 19, 235–250 (2022). https://doi.org/10.1007/s11904-022-00608-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-022-00608-y