Abstract
Purpose of Review
Antiretroviral therapy (ART) scale-up has dramatically reduced rates of pediatric HIV mortality and morbidity. Children living with perinatally acquired HIV (PHIV) are now expected to live through adolescence and well into adulthood, such that adolescents now represent the largest growing population living with HIV. This review aims to discuss the prevalence and mechanisms for cardiometabolic comorbidities in the setting of newer ART regimens and the research gaps that remain.
Recent Findings
Data highlight the continued risks of subclinical cardiometabolic complications in PHIV in the setting of newer ART. Novel techniques in imaging and omics may help identify early cardiometabolic abnormalities in this young population and potentially identify early changes in the mechanistic pathways related to these changes.
Summary
Further studies to determine risk and management strategies of the cardiometabolic effects in PHIV adolescents, beyond ART, are warranted. Focus should be on prevention of these complications in youth to avoid new epidemic of diabetes and cardiovascular disease when these youths become aging adults.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Organization TWH. Fact sheet HIV/AIDS. 2019.
Age limits and adolescents. Paediatr Child Health. 2003;8(9):577–8.
Centers for Disease Control and Prevention. HIV Surveillance Report. 2017.
Flynn PM, Abrams EJ. Growing up with perinatal HIV. AIDS (London, England). 2019;33(4):597–603.
Paula AA, Schechter M, Tuboi SH, Faulhaber JC, Luz PM, Veloso VG, et al. Continuous increase of cardiovascular diseases, diabetes, and non-HIV related cancers as causes of death in HIV-infected individuals in Brazil: an analysis of nationwide data. PloS one. 2014;9(4):e94636.
Elbirt D, Mahlab-Guri K, Bezalel-Rosenberg S, Gill H, Attali M, Asher I. HIV-associated neurocognitive disorders (HAND). Israel Med Assoc J: IMAJ. 2015;17(1):54–9.
Brady MT, Oleske JM, Williams PL, Elgie C, Mofenson LM, Dankner WM, et al. Declines in mortality rates and changes in causes of death in HIV-1-infected children during the HAART era. Journal of acquired immune deficiency syndromes (1999). 2010;53(1):86–94.
Patel K, Van Dyke RB, Mittleman MA, Colan SD, Oleske JM, Seage GR 3rd. The impact of HAART on cardiomyopathy among children and adolescents perinatally infected with HIV-1. AIDS (London, England). 2012;26(16):2027–37.
Savvoulidis P, Butler J, Kalogeropoulos A. Cardiomyopathy and heart failure in patients with HIV infection. Can J Cardiol. 2019;35(3):299–309.
Butler J, Greene SJ, Shah SH, Shah SJ, Anstrom KJ, Kim RJ, et al. Diastolic dysfunction in patients with human immunodeficiency virus receiving antiretroviral therapy: results from the CHART study. J Cardiac Fail. 2020;26(5):371–80.
• Lipshultz SE, Wilkinson JD, Thompson B, Cheng I, Briston DA, Shearer WT, et al. Cardiac effects of highly active antiretroviral therapy in perinatally HIV-infected children: The CHAART-2 Study. J Am Coll Cardiol. 2017;70(18):2240–7. This study compared echocardiograms from ART-exposed children to those of ART-unexposed children. Cardiac structure and function improved in PHIV children on ART compared to children in pre-ART area but did decline over time.
Wilkinson JD, Williams PL, Yu W, Colan SD, Mendez A, Zachariah JPV, et al. Cardiac and inflammatory biomarkers in perinatally HIV-infected and HIV-exposed uninfected children. AIDS (London, England). 2018;32(10):1267–77.
Namuyonga J, Lubega S, Musiime V, Lwabi P, Lubega I. Cardiac dysfunction among Ugandan HIV-infected children on antiretroviral therapy. Pediatr Infect Dis J. 2016;35(3):e85–8.
Majonga ED, Rehman AM, Simms V, McHugh G, Mujuru HA, Nathoo K, et al. High prevalence of echocardiographic abnormalities in older HIV-infected children taking antiretroviral therapy. AIDS (London, England). 2018;32(18):2739–48.
• Majonga ED, Rehman AM, McHugh G, Mujuru HA, Nathoo K, Odland JO, et al. Incidence and progression of echocardiographic abnormalities in older children with human immunodeficiency virus and adolescents taking antiretroviral therapy: a prospective cohort study. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2020;70(7):1372–8. Prospective longitudinal cohort in Zimbabwe of children on ART with echocardiograms at baseline and 18 months after; PHIV on ART have a high incidence of cardiac abnormalities that persist and progress over time.
• McCrary AW, Nyandiko WM, Ellis AM, Chakraborty H, Muehlbauer MJ, Koech MM, et al. Early cardiac dysfunction in children and young adults with perinatally acquired HIV. AIDS (London, England). 2020;34(4):539–48. In a large cohort in Kenya (n=643) with a mean age of 14 years old, echocardiogram was performed to assess for early cardiac dysfunction as measured by left ventricular strain and myocardial performance index. A total of 28% of children had early cardiac dysfunction. AZT exposure was independently association with strain.
Andrew McCrary WN, Michasel J Muehlbauer, Ibrahim Daug, Nathan M Thielman, Maggie Nguyen, Svati J. Shah, Gerald S. Bloomfield, editor Serum biomarkers identify cardiac dysfunction in youth living with HIV. CROI; 2021; Virtual.
Terai M, Ohishi M, Ito N, Takagi T, Tatara Y, Kaibe M, et al. Comparison of arterial functional evaluations as a predictor of cardiovascular events in hypertensive patients: the Non-Invasive Atherosclerotic Evaluation in Hypertension (NOAH) study. Hypertension research: official journal of the Japanese Society of Hypertension. 2008;31(6):1135–45.
Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113(5):657–63.
Shokawa T, Imazu M, Yamamoto H, Toyofuku M, Tasaki N, Okimoto T, et al. Pulse wave velocity predicts cardiovascular mortality: findings from the Hawaii-Los Angeles-Hiroshima study. Circ J. 2005;69(3):259–64.
McComsey GA, O’Riordan M, Hazen SL, El-Bejjani D, Bhatt S, Brennan ML, et al. Increased carotid intima media thickness and cardiac biomarkers in HIV infected children. AIDS (London, England). 2007;21(8):921–7.
Charakida M, Donald AE, Green H, Storry C, Clapson M, Caslake M, et al. Early structural and functional changes of the vasculature in HIV-infected children: impact of disease and antiretroviral therapy. Circulation. 2005;112(1):103–9.
Sainz T, Alvarez-Fuente M, Navarro ML, Diaz L, Rojo P, Blazquez D, et al. Subclinical atherosclerosis and markers of immune activation in HIV-infected children and adolescents: the CaroVIH study. Journal of acquired immune deficiency syndromes (1999). 2014;65(1):42–9.
Bonnet D, Aggoun Y, Szezepanski I, Bellal N, Blanche S. Arterial stiffness and endothelial dysfunction in HIV-infected children. AIDS (London, England). 2004;18(7):1037–41.
Chanthong P, Lapphra K, Saihongthong S, Sricharoenchai S, Wittawatmongkol O, Phongsamart W, et al. Echocardiography and carotid intima-media thickness among asymptomatic HIV-infected adolescents in Thailand. AIDS (London, England). 2014;28(14):2071–9.
Marsico F, Lo Vecchio A, Paolillo S, DʼAndrea C, De Lucia V, Bruzzese E, et al. Left ventricular function, epicardial adipose tissue, and carotid intima-media thickness in children and adolescents with vertical HIV infection. Journal of acquired immune deficiency syndromes (1999). 2019;82(5):462–7.
Charakida M, Loukogeorgakis SP, Okorie MI, Masi S, Halcox JP, Deanfield JE, et al. Increased arterial stiffness in HIV-infected children: risk factors and antiretroviral therapy. Antivir Ther. 2009;14(8):1075–9.
Eckard AR, Raggi P, Ruff JH, O’Riordan MA, Rosebush JC, Labbato D, et al. Arterial stiffness in HIV-infected youth and associations with HIV-related variables. Virulence. 2017;8(7):1265–73.
Gleason RL Jr, Caulk AW, Seifu D, Rosebush JC, Shapiro AM, Schwartz MH, et al. Efavirenz and ritonavir-boosted lopinavir use exhibited elevated markers of atherosclerosis across age groups in people living with HIV in Ethiopia. J Biomech. 2016;49(13):2584–92.
•• Hanna DB, Guo M, Buzkova P, Miller TL, Post WS, Stein JH, et al. HIV infection and carotid artery intima-media thickness: pooled analyses across 5 cohorts of the NHLBI HIV-CVD collaborative. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;63(2):249–56. Through a NHLBI research consortium, this study analyzed IMT measurements from 5 studies and >2000 HIV+ individuals, including 221 6–29-year-old HIV+ and 58 HIV-. There was higher IMT in this group when compared to uninfected participants and the increase in IMT in HIV+ was strengthened when limited to PHIV.
• Dirajlal-Fargo S, Albar Z, Bowman E, Labbato D, Sattar A, Karungi C, et al. Subclinical vascular disease in children with human immunodeficiency virus in Uganda is associated with intestinal barrier dysfunction. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2020;71(12):3025–32. In a cross-sectional study, Ugandan PHIV, virally suppressed on ART, had evidence of higher IMT compared to HIV- which was independently associated with alteration in gut barrier.
Majonga ED, Chiesa ST, McHugh G, Mujuru H, Nathoo K, Odland JO, et al. Carotid intima media thickness in older children and adolescents with HIV taking antiretroviral therapy. Medicine. 2020;99(17):e19554.
Abd-Elmoniem KZ, Unsal AB, Eshera S, Matta JR, Muldoon N, McAreavey D, et al. Increased coronary vessel wall thickness in HIV-infected young adults. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2014;59(12):1779–86.
Poredos P. Endothelial dysfunction in the pathogenesis of atherosclerosis. International angiology: a journal of the International Union of Angiology. 2002;21(2):109–16.
Widlansky ME, Gokce N, Keaney JF Jr, Vita JA. The clinical implications of endothelial dysfunction. J Am Coll Cardiol. 2003;42(7):1149–60.
Gokce N, Keaney JF Jr, Hunter LM, Watkins MT, Nedeljkovic ZS, Menzoian JO, et al. Predictive value of noninvasively determined endothelial dysfunction for long-term cardiovascular events in patients with peripheral vascular disease. J Am Coll Cardiol. 2003;41(10):1769–75.
Hijmering ML, Stroes ES, Pasterkamp G, Sierevogel M, Banga JD, Rabelink TJ. Variability of flow mediated dilation: consequences for clinical application. Atherosclerosis. 2001;157(2):369–73.
Mahtab S, Zar HJ, Ntusi NAB, Joubert S, Asafu-Agyei NAA, Luff NJ, et al. Endothelial dysfunction in South African youth living with perinatally acquired human immunodeficiency virus on antiretroviral therapy. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2020;71(10):e672–9.
Dirajlal-Fargo S, Sattar A, Kulkarni M, Bowman E, Funderburg N, McComsey GA. HIV-positive youth who are perinatally infected have impaired endothelial function. AIDS (London, England). 2017;31(14):1917–24.
Bush KNV, Teel JL, Watts JA, Gore RS, Alvarado G, Harper NL, et al. Association of endothelial dysfunction and antiretroviral therapy in early HIV infection. JAMA Network Open. 2019;2(10):e1913615-e.
Domingo P, Estrada V, López-Aldeguer J, Villaroya F, Martínez E. Fat redistribution syndromes associated with HIV-1 infection and combination antiretroviral therapy. AIDS Rev. 2012;14(2):112–23.
Mallon PW, Miller J, Cooper DA, Carr A. Prospective evaluation of the effects of antiretroviral therapy on body composition in HIV-1-infected men starting therapy. AIDS (London, England). 2003;17(7):971–9.
Cames C, Pascal L, Ba A, Mbodj H, Ouattara B, Diallo NF, et al. Low prevalence of lipodystrophy in HIV-infected Senegalese children on long-term antiretroviral treatment: the ANRS 12279 MAGGSEN Pediatric Cohort Study. BMC Infect Dis. 2018;18(1):374.
Bwakura-Dangarembizi M, Musiime V, Szubert AJ, Prendergast AJ, Gomo ZA, Thomason MJ, et al. Prevalence of lipodystrophy and metabolic abnormalities in HIV-infected African children after 3 years on first-line antiretroviral therapy. Pediatr Infect Dis J. 2015;34(2):e23-31.
Crum-Cianflone N, Roediger MP, Eberly L, Headd M, Marconi V, Ganesan A, et al. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PloS one. 2010;5(4):e10106.
Crum-Cianflone N, Tejidor R, Medina S, Barahona I, Ganesan A. Obesity among patients with HIV: the latest epidemic. AIDS Patient Care STDS. 2008;22(12):925–30.
Koethe JR, Lagathu C, Lake JE, Domingo P, Calmy A, Falutz J, et al. HIV and antiretroviral therapy-related fat alterations. Nat Rev Dis Primers. 2020;6(1):48.
Jacobson DL, Lindsey JC, Coull BA, Mulligan K, Bhagwat P, Aldrovandi GM. The association of fat and lean tissue with whole body and spine bone mineral density is modified by HIV status and sex in children and youth. Pediatr Infect Dis J. 2018;37(1):71–7.
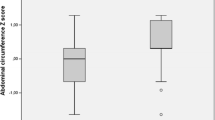
Jacobson DL, Patel K, Siberry GK, Van Dyke RB, DiMeglio LA, Geffner ME, et al. Body fat distribution in perinatally HIV-infected and HIV-exposed but uninfected children in the era of highly active antiretroviral therapy: outcomes from the Pediatric HIV/AIDS Cohort Study. Am J Clin Nutr. 2011;94(6):1485–95.
•• Sharma TS, Somarriba G, Arheart KL, Neri D, Mathew MS, Graham PL, et al. Longitudinal changes in body composition by dual-energy radiograph absorptiometry among perinatally HIV-infected and HIV-uninfected youth: Increased Risk of Adiposity Among HIV-infected Female Youth. Pediatr Infect Dis J. 2018;37(10):1002–7. PHIV on ART and HIV- controls were prospectively enrolled and DXA scans were obtained in a longitudinal fashion over a median of 2.5 years; PHIV females had significant increases in total percent body and trunk fat compared to HIV- females and PHIV males.
Aurpibul L, Namwongprom S, Sudjaritruk T, Ounjaijean S. Metabolic syndrome, biochemical markers, and body composition in youth living with perinatal HIV infection on antiretroviral treatment. PloS one. 2020;15(3):e0230707.
• Cohen S, Innes S, Geelen SP, Wells JC, Smit C, Wolfs TF, et al. Long-term changes of subcutaneous fat mass in HIV-infected children on antiretroviral therapy: a retrospective analysis of longitudinal data from two pediatric HIV-cohorts. PloS one. 2015;10(7):e0120927. A total of 218 PHIV children in South Africa and the Netherlands underwent DXA scans over a period of 3.5 years. Findings highlight ongoing subcutaneous fat loss in PHIV on ART associated with prior stavudine exposure.
Arpadi SM, Bethel J, Horlick M, Sarr M, Bamji M, Abrams EJ, et al. Longitudinal changes in regional fat content in HIV-infected children and adolescents. AIDS (London, England). 2009;23(12):1501–9.
Food and Drug Administration. FDA News Release: FDA approves drug to treat infants and children with HIV 2020 [Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-drug-treat-infants-and-children-hiv.
Bourgi K, Rebeiro PF, Turner M, Castilho JL, Hulgan T, Raffanti SP, et al. Greater weight gain in treatment naive persons starting dolutegravir-based antiretroviral therapy. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2019;70(7):1267–74.
Sax PE, Erlandson KM, Lake JE, McComsey GA, Orkin C, Esser S, et al. Weight gain following initiation of antiretroviral therapy: risk factors in randomized comparative clinical trials [published online ahead of print, 2019 Oct 14]. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2019;ciz999.
Venter WDF, Moorhouse M, Sokhela S, Fairlie L, Mashabane N, Masenya M, et al. Dolutegravir plus two different prodrugs of tenofovir to treat HIV. N Engl J Med. 2019;381(9):803–15.
Lamorde M, Atwiine M, Owarwo NC, Ddungu A, Laker EO, Mubiru F, et al. Dolutegravir-associated hyperglycaemia in patients with HIV [published online ahead of print, 2020 Feb 24]. Lancet HIV. 2020;S2352–3018(20)30042–4.
Sahera Dirajlal-fargo WLAK, Matthew E. Levy, Anne K. Monroe, Amanda D. Castel, Natella Rakhmanina, editor Effect of integrase inhibitors on weight gain in children and adolescents with HIV. CROI; 2020 03/2020; Virtual.
Giacomet V, Lazzarin S, Manzo A, Paradiso L, Maruca K, Barera G, et al. Body fat distribution and metabolic changes in a cohort of adolescents living with HIV switched to an antiretroviral regimen containing dolutegravir. Pediatr Infect Dis J. 2021;40(5):457–9.
• Turkova A, editor Dolutegravir-based ART is superior to NNRI/PI-based ART in children and adolescents. CROI; 2021; virtual. Findings from ODYSSEY trial, an open-label multicountry randomized trial presented at CROI 2021. PHIV randomized to DTG highlighted a slight but significant increase in BMI compared to standard of care.
Erlandson KM, Lake JE. Fat matters: understanding the role of adipose tissue in health in HIV infection. Curr HIV/AIDS Rep. 2016;13(1):20–30.
Alexopoulos N, Katritsis D, Raggi P. Visceral adipose tissue as a source of inflammation and promoter of atherosclerosis. Atherosclerosis. 2014;233(1):104–12.
El Kamari V, Moser C, Hileman CO, Currier JS, Brown TT, Johnston L, et al. Lower pretreatment gut integrity is independently associated with fat gain on antiretroviral therapy. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2019;68(8):1394–401.
Gojanovich GS, Jacobson DL, Jao J, Russell JS, Van Dyke RB, Libutti DE, et al. Mitochondrial dysfunction and insulin resistance in pubertal youth living with perinatally acquired HIV. AIDS Res Hum Retroviruses. 2020;36(9):703–11.
Hulgan T, Ramsey BS, Koethe JR, Samuels DC, Gerschenson M, Libutti DE, et al. Relationships between adipose mitochondrial function, serum adiponectin, and insulin resistance in persons with HIV after 96 weeks of antiretroviral therapy. Journal of acquired immune deficiency syndromes (1999). 2019;80(3):358–66.
Jao J, Jacobson DL, Russell JS, Wang J, Yu W, Gojanovich GS, et al. Perinatally acquired HIV infection is associated with abnormal blood mitochondrial function during childhood/adolescence. AIDS (London, England). 2021;Publish Ahead of Print.
McComsey GA, Daar ES, O’Riordan M, Collier AC, Kosmiski L, Santana JL, et al. Changes in fat mitochondrial DNA and function in subjects randomized to abacavir-lamivudine or tenofovir DF-emtricitabine with atazanavir-ritonavir or efavirenz: AIDS Clinical Trials Group study A5224s, substudy of A5202. J Infect Dis. 2013;207(4):604–11.
Bouter KE, van Raalte DH, Groen AK, Nieuwdorp M. Role of the gut microbiome in the pathogenesis of obesity and obesity-related metabolic dysfunction. Gastroenterology. 2017;152(7):1671–8.
Koay WLA, Lindsey JC, Uprety P, Bwakura-Dangarembizi M, Weinberg A, Levin MJ, et al. Intestinal integrity biomarkers in early antiretroviral-treated perinatally HIV-1-infected infants. J Infect Dis. 2018;218(7):1085–9.
•• Dirajlal-Fargo S, El-Kamari V, Weiner L, Shan L, Sattar A, Kulkarni M, et al. Altered intestinal permeability and fungal translocation in Ugandan children with HIV. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2019. In this cross-sectional study performed in Uganda, PHIV had evidence of alteration in intestinal permeability compared to HIV- and HEU children despite viral suppression on ART. In PHIV, these markers correlated with systemic inflammation.
Sahera Dirajlal-Fargo DJ, Wendy Yu, Ayesha Mirza, Mitchell E. Geffner, Jennifer Jao, Grace A. McComsey , on behalf of the Pediatric HIV/AIDS Cohort Study (PHACS). Gut markers’ associations with body fat in youth living with perinatally-acquired HIV. Conference of Retroviruses and Opportunistic Infections-2021; Virtual2021.
Blázquez D, Ramos-Amador JT, Saínz T, Mellado MJ, García-Ascaso M, De José MI, et al. Lipid and glucose alterations in perinatally-acquired HIV-infected adolescents and young adults. BMC Infect Dis. 2015;15:119.
Espiau M, Yeste D, Noguera-Julian A, González-Tomé MI, Falcón-Neyra L, Gavilán C, et al. Metabolic syndrome in children and adolescents living with HIV. Pediatr Infect Dis J. 2016;35(6):e171–6.
Espiau M, Yeste D, Noguera-Julian A, Soler-Palacín P, Fortuny C, Ferrer R, et al. Adiponectin, leptin and inflammatory markers in HIV-associated metabolic syndrome in children and adolescents. Pediatr Infect Dis J. 2017;36(2):e31–7.
Frigati LJ, Jao J, Mahtab S, Asafu Agyei NA, Cotton MF, Myer L, et al. Insulin resistance in South African youth living with perinatally acquired HIV receiving antiretroviral therapy. AIDS Res Hum Retroviruses. 2019;35(1):56–62.
Geffner ME, Patel K, Jacobson DL, Wu J, Miller TL, Hazra R, et al. Changes in insulin sensitivity over time and associated factors in HIV-infected adolescents. AIDS (London, England). 2018;32(5):613–22.
Innes S, Abdullah KL, Haubrich R, Cotton MF, Browne SH. High prevalence of dyslipidemia and insulin resistance in HIV-infected prepubertal African children on antiretroviral therapy. Pediatr Infect Dis J. 2016;35(1):e1-7.
Paganella MP, Cohen RA, Harris DR, de Souza Kuchenbecker R, Sperhacke RD, Kato SK, et al. Association of dyslipidemia and glucose abnormalities with antiretroviral treatment in a cohort of HIV-infected Latin American children. Journal of acquired immune deficiency syndromes (1999). 2017;74(1):e1-e8.
Santiprabhob J, Chokephaibulkit K, Khantee P, Maleesatharn A, Phonrat B, Phongsamart W, et al. Adipocytokine dysregulation, abnormal glucose metabolism, and lipodystrophy in HIV-infected adolescents receiving protease inhibitors. Cytokine. 2020;136:155145.
Santiprabhob J, Tanchaweng S, Maturapat S, Maleesatharn A, Lermankul W, Sricharoenchai S, et al. Metabolic disorders in HIV-infected adolescents receiving protease inhibitors. Biomed Res Int. 2017;2017:7481597.
Takemoto JK, Miller TL, Wang J, Jacobson DL, Geffner ME, Van Dyke RB, et al. Insulin resistance in HIV-infected youth is associated with decreased mitochondrial respiration. AIDS (London, England). 2017;31(1):15–23.
Dirajlal-Fargo S, Musiime V, Cook A, Mirembe G, Kenny J, Jiang Y, et al. Insulin resistance and markers of inflammation in HIV-infected Ugandan children in the CHAPAS-3 trial. Pediatr Infect Dis J. 2017;36(8):761–7.
Dirajlal-Fargo S, Shan L, Sattar A, Bowman E, Gabriel J, Kulkarni M, et al. Insulin resistance and intestinal integrity in children with and without HIV infection in Uganda. HIV Med. 2020;21(2):119–27.
Moran A, Jacobs DR Jr, Steinberger J, Steffen LM, Pankow JS, Hong CP, et al. Changes in insulin resistance and cardiovascular risk during adolescence: establishment of differential risk in males and females. Circulation. 2008;117(18):2361–8.
Hannon TS, Janosky J, Arslanian SA. Longitudinal study of physiologic insulin resistance and metabolic changes of puberty. Pediatr Res. 2006;60(6):759–63.
Dimock D, Thomas V, Cushing A, Purdy JB, Worrell C, Kopp JB, et al. Longitudinal assessment of metabolic abnormalities in adolescents and young adults with HIV-infection acquired perinatally or in early childhood. Metabolism: clinical and experimental. 2011;60(6):874–80.
• Jao J, Yu W, Patel K, Miller TL, Karalius B, Geffner ME, et al. Improvement in lipids after switch to boosted atazanavir or darunavir in children/adolescents with perinatally acquired HIV on older protease inhibitors: results from the Pediatric HIV/AIDS Cohort Study. HIV Med. 2018;19(3):175–83. PHIV enrolled in PHACS who switched to ATV/r or DRV/r compared to those who remained on older PI had a more rappid reduction in lipids.
Rutstein RM, Samson P, Fenton T, Fletcher CV, Kiser JJ, Mofenson LM, et al. Long-term safety and efficacy of atazanavir-based therapy in HIV-infected infants, children and adolescents: the Pediatric AIDS Clinical Trials Group Protocol 1020A. Pediatr Infect Dis J. 2015;34(2):162–7.
Munger AM, Chow DC, Playford MP, Parikh NI, Gangcuangco LM, Nakamoto BK, et al. Characterization of lipid composition and high-density lipoprotein function in HIV-infected individuals on stable antiretroviral regimens. AIDS Res Hum Retroviruses. 2015;31(2):221–8.
Wong G, Trevillyan JM, Fatou B, Cinel M, Weir JM, Hoy JF, et al. Plasma lipidomic profiling of treated HIV-positive individuals and the implications for cardiovascular risk prediction. PloS one. 2014;9(4):e94810.
• Dirajlal-Fargo S, Sattar A, Yu J, Albar Z, Chaves FC, Riedl K, et al. Lipidome association with vascular disease and inflammation in HIV+ Ugandan children. AIDS (London, England). 2021. In this small pilot study, Ugandan PHIV (n=20) compared to HIV- (n=20) had evidence of altered lipidomic panel and increased lipid species known to be inflammatory and associated with CVD.
Bowman ER, Kulkarni M, Gabriel J, Cichon MJ, Riedl K, Belury MA, et al. Altered lipidome composition is related to markers of monocyte and immune activation in antiretroviral therapy treated human immunodeficiency virus (HIV) infection and in uninfected persons. Front Immunol. 2019;10:785.
Puri P, Wiest MM, Cheung O, Mirshahi F, Sargeant C, Min HK, et al. The plasma lipidomic signature of nonalcoholic steatohepatitis. Hepatology (Baltimore, MD). 2009;50(6):1827–38.
Taramasso L, Di Biagio A, Bovis F, Forlanini F, Albani E, Papaioannu R, et al. Switching to integrase inhibitors unlinked to weight increase in perinatally HIV-infected young adults and adolescents: a 10-year observational study. Microorganisms. 2020;8(6):864.
al TNe, editor Optimization to dolutegravir-based ART in a cohort of virally suppressed adolescents is associated with an increase in the rate of BMI change and odds of becoming overweight. AIDS 2020; 2020; virtual.
Yeoh DK, Campbell AJ, Bowen AC. Increase in body mass index in children with HIV, switched to tenofovir alafenamide fumarate or dolutegravir containing antiretroviral regimens. Pediatr Infect Dis J. 2021;40(5):e215–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Complications of HIV and Antiretroviral Therapy
Rights and permissions
About this article
Cite this article
Dirajlal-Fargo, S., McComsey, G.A. Cardiometabolic Complications in Youth With Perinatally Acquired HIV in the Era of Antiretroviral Therapy. Curr HIV/AIDS Rep 18, 424–435 (2021). https://doi.org/10.1007/s11904-021-00574-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-021-00574-x