Abstract
Purpose of Review
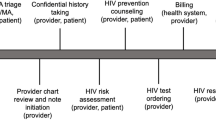
Shared decision-making is a process that involves bidirectional exchange of information between patients and providers to support patients in making individualized, evidence-based decisions about their healthcare. We review the evidence on patient-led decision-making, a form of shared decision-making that maximizes patient autonomy, as a framework for decisions about HIV preexposure prophylaxis (PrEP). We also assess the likelihood that patient-led decision-making occurs for PrEP and describe interventions to facilitate this process.
Recent Findings
Patient-led decision-making is likely to be uncommon for PrEP, in part because healthcare providers lack knowledge and training about PrEP. Few evidence-based interventions exist to facilitate patient-led decision-making for PrEP.
Summary
There is a need for rigorously developed interventions to increase knowledge of PrEP among patients and healthcare providers and support patient-led decision-making for PrEP, which will be increasingly important as the range of available PrEP modalities expands.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Chou R, Evans C, Hoverman A, Sun C, Dana T, Bougatsos C, et al. Preexposure prophylaxis for the prevention of HIV infection: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(22):2214–30 The United States Preventive Services Task Force issued a Grade A recommendation for the use of tenofovir disoproxil fumarate with emtricitabine as daily oral HIV preexposure prophylaxis (PrEP), indicating strong evidence of net clinical benefit for this regimen. This review summarizes the clinical evidence in support of the Grade A recommendation for PrEP, which can inform decision-support interventions for PrEP.
Volk JE, Marcus JL, Phengrasamy T, Blechinger D, Nguyen DP, Follansbee S, et al. No new HIV infections with increasing use of HIV preexposure prophylaxis in a clinical practice setting. Clin Infect Dis. 2015;61(10):1601–3.
Kanny D, Jeffries WL, Chapin-Bardales J, Denning P, Cha S, Finlayson T, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men - 23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(37):801–6.
• McFarland W, Lin J, Santos GM, Arayasirikul S, Raymond HF, Wilson E. Low PrEP Awareness and Use Among People Who Inject Drugs, San Francisco, 2018. AIDS Behav. 2020;24(5):1290–1293. https://doi.org/10.1007/s10461-019-02682-7. This study of people who inject drugs in San Francisco found that only 57% had heard of PrEP, 14% had discussed PrEP with a provider, and 3% had used PrEP in the prior year, highlighting a need for interventions to improve knowledge, patient-provider discussions, and use of PrEP for this key population.
Finlayson T, Cha S, Xia M, Trujillo L, Denson D, Prejean J, et al. Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men - 20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68(27):597–603.
Marcus JL, Hurley LB, Dentoni-Lasofsky D, Ellis CG, Silverberg MJ, Slome S, et al. Barriers to preexposure prophylaxis use among individuals with recently acquired HIV infection in Northern California. AIDS Care. 2019;31(5):536–44.
Hill LM, Lightfoot AF, Riggins L, Golin CE. Awareness of and attitudes toward pre-exposure prophylaxis among African American women living in low-income neighborhoods in a Southeastern city. AIDS Care. 2020;25:1–5. https://doi.org/10.1080/09540121.2020.1769834.
Qin Y, Price C, Rutledge R, Puglisi L, Madden LM, Meyer JP. Women's decision-making about PrEP for HIV prevention in drug treatment contexts. J Int Assoc Provid AIDS Care. 2020;19:2325958219900091.
Kimball D, Rivera D, Gonzales M 4th, Blashill AJ. Medical Mistrust and the PrEP Cascade Among Latino Sexual Minority Men. AIDS Behav. 2020;24(12):3456–3461. https://doi.org/10.1007/s10461-020-02916-z.
•• Pleuhs B, Quinn KG, Walsh JL, Petroll AE, John SA. Health care provider barriers to HIV pre-exposure prophylaxis in the United States: a systematic review. AIDS Patient Care STDS. 2020;34(3):111–23 In this systematic review of healthcare provider barriers to PrEP provision in the United States, the authors identified several themes of barriers to PrEP. These themes included providers’ knowledge gaps, discordance in beliefs between HIV specialists and primary care providers on who should prescribe PrEP, interpersonal stigma, and concerns about PrEP costs, patient adherence, and behavioral and health consequences of PrEP use. These barriers represent important targets for interventions to improve providers’ engagement in patient-led decision-making for PrEP.
Goparaju L, Praschan NC, Warren-Jeanpiere L, Experton LS, Young MA, Kassaye S. Stigma, Partners, Providers and Costs: Potential Barriers to PrEP Uptake among US Women. J AIDS Clin Res. 2017;8(9):730. https://doi.org/10.4172/2155-6113.1000730.
Marcus JL, Katz KA, Krakower DS, Calabrese SK. Risk compensation and clinical decision making - the case of HIV preexposure prophylaxis. N Engl J Med. 2019;380(6):510–2.
Elwyn G, Laitner S, Coulter A, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7.
Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681–92.
(2001) Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC).
Kon AA. The shared decision-making continuum. JAMA. 2010;304(8):903–4.
Chen M, Lindley A, Kimport K, Dehlendorf C. An in-depth analysis of the use of shared decision making in contraceptive counseling. Contraception. 2019;99(3):187–91.
Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301–12.
Elwyn G, Frosch D, Rollnick S. Dual equipoise shared decision making: definitions for decision and behaviour support interventions. Implement Sci. 2009;4:75.
Marcus JL, Snowden JM. Words matter: putting an end to "unsafe" and "risky" sex. Sex Transm Dis. 2020;47(1):1–3.
Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94(3):291–309.
Legare F, Ratte S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals' perceptions. Patient Educ Couns. 2008;73(3):526–35.
Blanc X, Collet TH, Auer R, Fischer R, Locatelli I, Iriarte P, et al. Publication trends of shared decision making in 15 high impact medical journals: a full-text review with bibliometric analysis. BMC Med Inform Decis Mak. 2014;14:71.
Blumenthal J, Jain S, Krakower D, Sun X, Young J, Mayer K, et al. Knowledge is power! Increased provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19(5):802–10.
Seidman D, Carlson K, Weber S, Witt J, Kelly PJ. United States family planning providers' knowledge of and attitudes towards preexposure prophylaxis for HIV prevention: a national survey. Contraception. 2016;93(5):463–9.
Tellalian D, Maznavi K, Bredeek UF, Hardy WD. Pre-exposure prophylaxis (PrEP) for HIV infection: results of a survey of HIV healthcare providers evaluating their knowledge, attitudes, and prescribing practices. AIDS Patient Care STDs. 2013;27(10):553–9.
•• Zhang C, McMahon J, Fiscella K, Przybyla S, Braksmajer A, LeBlanc N, et al. HIV pre-exposure prophylaxis implementation cascade among health care professionals in the United States: implications from a systematic review and meta-analysis. AIDS Patient Care STDS. 2019;33(12):507–27 The authors conducted a systematic review to characterize the PrEP implementation cascade (i.e., awareness, willingness, consultation, and prescription) among health care professionals in the United States. Only two-thirds of professionals were aware or willing to prescribe PrEP, and only about one-third had engaged patients in PrEP consultations, suggesting a need to prepare more providers to engage patients in discussions and decision-making about PrEP.
Haynes RB, Devereaux PJ, Guyatt GH. Physicians' and patients' choices in evidence based practice. BMJ. 2002;324(7350):1350.
Bazzi AR, Biancarelli DL, Childs E, Drainoni ML, Edeza A, Salhaney P, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDs. 2018;32(12):529–37.
Misra K, Udeagu CC. Disparities in awareness of HIV postexposure and preexposure prophylaxis among notified partners of HIV-positive individuals, New York City 2015-2017. J Acquir Immune Defic Syndr. 2017;76(2):132–40.
Roth AM, Tran NK, Piecara BL, Shinefeld J, Brady KA. Pre-exposure prophylaxis (PrEP) awareness is low among heterosexual people of color who might benefit from PrEP in Philadelphia. J Prim Care Community Health. 2019;10:2150132719847383.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34.
McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60.
U.S. Food and Drug Administration. FDA Briefing Information for the August 7, 2019 Meeting of the Antimicrobial Drugs Advisory Committee. Available at: https://www.fda.gov/media/129607/download.
Mayer KH, Molina JM, Thompson MA, Anderson PL, Mounzer KC, De Wet JJ, et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet. 2020;396(10246):239–54.
FDA approves second drug to prevent HIV infection as part of ongoing efforts to end the HIV epidemic. FDA news release. October 3, 2019. Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-second-drug-prevent-hiv-infection-part-ongoing-efforts-end-hiv-epidemic. .
World Health Organization. What’s the 2+1+1? Event-driven oral pre-exposure prophylaxis to prevent HIV for men who have sex with men: update to WHO’s recommendation on oral PrEP [Internet]. 2019. Available from: https://www.who.int/hiv/pub/prep/211/en/.
Cottrell ML, Yang KH, Prince HMA, Sykes C, White N, Malone S, et al. A translational pharmacology approach to predicting outcomes of preexposure prophylaxis against HIV in men and women using tenofovir disoproxil fumarate with or without Emtricitabine. J Infect Dis. 2016;214(1):55–64.
Baeten JM, Palanee-Phillips T, Brown ER, Schwartz K, Soto-Torres LE, Govender V, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med. 2016;375(22):2121–32.
Nel A, van Niekerk N, Kapiga S, Bekker L-G, Gama C, Gill K, et al. Safety and efficacy of a dapivirine vaginal ring for HIV prevention in women. N Engl J Med. 2016;375(22):2133–43.
European Medicines Agency. Dapivirine vaginal ring 25 mg. July 24, 2020. Available at: https://www.ema.europa.eu/en/dapivirine-vaginal-ring-25-mg-h-w-2168.
PrEPWatch. Dapivarine vaginal ring. July 24, 2020. Available at: https://www.prepwatch.org/nextgen-prep/dapivirine-vaginal-ring/.
Long-acting injectable cabotegravir is highly effective for the prevention of HIV infection in cisgender men and transgender women who have sex with men. HIV Prevention Trials Network news release. May 18, 2020. Available at: https://www.hptn.org/news-and-events/press-releases/long-acting-injectable-cabotegravir-highly-effective-prevention-hiv#:~:text=Overall%2C%20HPTN%20083%20enrolled%204%2C570,%2C%20Vietnam%2C%20and%20South%20Africa.&text=These%20results%20demonstrate%20that%20CAB,cisgender%20men%20and%20transgender%20women.
• Calabrese SK, Krakower DS, Mayer KH. Integrating HIV preexposure prophylaxis (PrEP) into routine preventive health care to avoid exacerbating disparities. Am J Public Health. 2017;107(12):1883–9 In this commentary, the authors propose routine offering of PrEP as part of preventive health care as a way to reduce inequities in PrEP awareness, access and use.
• Calabrese SK, Earnshaw VA, Underhill K, Krakower DS, Magnus M, Hansen NB, et al. Prevention paradox: medical students are less inclined to prescribe HIV pre-exposure prophylaxis for patients in highest need. J Int AIDS Soc. 2018;21(6):e25147 The authors presented medical students with hypothetical scenarios about patients who may benefit from PrEP use and found that students indicted lower prescribing intentions for patients with higher risk of HV acquisition, such as those who intended not to use condoms. These findings suggest that prescribers’ biases about what constitutes appropriate sexual health behaviors could negatively impact patient autonomy in PrEP decisions.
Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226–40.
Chan SS, Chappel AR, Maddox KEJ, Hoover KW, Huang YA, Zhu W, et al. Pre-exposure prophylaxis for preventing acquisition of HIV: a cross-sectional study of patients, prescribers, uptake, and spending in the United States, 2015-2016. PLoS Med. 2020;17(4):e1003072.
Gavin L, Pazol K. Update: providing quality family planning services — recommendations from CDC and the U.S. Office of Population Affairs, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:231–4.
Seidman D, Weber S, Carlson K, Witt J. Family planning providers' role in offering PrEP to women. Contraception. 2018;97(6):467–70.
Seidman D, Weber S. Integrating Preexposure prophylaxis for human immunodeficiency virus prevention into women's health care in the United States. Obstet Gynecol. 2016;128(1):37–43.
Dehlendorf C, Fitzpatrick J, Steinauer J, Swiader L, Grumbach K, Hall C, et al. Development and field testing of a decision support tool to facilitate shared decision making in contraceptive counseling. Patient Educ Couns. 2017;100(7):1374–81.
Dehlendorf C, Grumbach K, Schmittdiel JA, Steinauer J. Shared decision making in contraceptive counseling. Contraception. 2017;95(5):452–5.
Gilkey MB, Marcus JL, Garrell JM, Powell VE, Maloney KM, Krakower DS. Using HIV risk prediction tools to identify candidates for pre-exposure prophylaxis: perspectives from patients and primary care providers. AIDS Patient Care STDs. 2019;33(8):372–8.
• Nunn AS, Goedel WC, Gomillia CE, Coats CS, Patel RR, Murphy MJ, Chu CT, Chan PA, Mena LA. False information on PrEP in direct-to-consumer advertising. Lancet HIV. 2020;7(7):e455-e456. https://doi.org/10.1016/S2352-3018(20)30034-5. This study identified false information about PrEP on social media platforms, which could jeopardize effective patient-led decision-making about PrEP. Patients and providers need to be aware that information about PrEP on social media may be inaccurate, and these decision-makers need access to sources of unbiased information about PrEP.
Miltz A, Lampe F, McCormack S, Dunn D, White E, Rodger A, et al. Prevalence and correlates of depressive symptoms among gay, bisexual and other men who have sex with men in the PROUD randomised clinical trial of HIV pre-exposure prophylaxis. BMJ Open. 2019;9(12):e031085.
Grov C, Rendina HJ, John SA, Parsons JT. Determining the roles that club drugs, marijuana, and heavy drinking play in PrEP medication adherence among gay and bisexual men: implications for treatment and research. AIDS Behav. 2019;23(5):1277–86.
Hojilla JC, Vlahov D, Glidden DV, Amico KR, Mehrotra M, Hance R, et al. Skating on thin ice: stimulant use and sub-optimal adherence to HIV pre-exposure prophylaxis. J Int AIDS Soc. 2018;21(3):e25103.
Hoenigl M, Jain S, Moore D, Collins D, Sun X, Anderson PL, Corado K, Blumenthal JS, Daar ES, Milam J, Dubé MP, Morris S; California Collaborative Treatment Group 595 Team. Substance Use and Adherence to HIV Preexposure Prophylaxis for Men Who Have Sex with Men1. Emerg Infect Dis. 2018;24(12):2292–302. https://doi.org/10.3201/eid2412.180400.
Storholm ED, Volk JE, Marcus JL, Silverberg MJ, Satre DD. Risk perception, sexual behaviors, and PrEP adherence among substance-using men who have sex with men: a qualitative study. Prev Sci. 2017;18(6):737–47.
Dehlendorf C, Fitzpatrick J, Fox E, Holt K, Vittinghoff E, Reed R, et al. Cluster randomized trial of a patient-centered contraceptive decision support tool, My Birth Control. Am J Obstet Gynecol. 2019;220(6):565.e1–e12.
Weymiller AJ, Montori VM, Jones LA, Gafni A, Guyatt GH, Bryant SC, et al. Helping patients with type 2 diabetes mellitus make treatment decisions: statin choice randomized trial. Arch Intern Med. 2007;167(10):1076–82.
•• Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:Cd001431 This Cochrane Database Systematic Review found that people exposed to decision aids before health care decisions tended to feel better informed and clearer about their values, and may have had a more active role in decision making and more accurate risk perceptions. Because the review identified no adverse effects on health outcomes or satisfaction, this review provides strong evidence that decision aids can improve patient-led decision-making in general and thus potentially for PrEP.
O’Connor AM (2006) Ottawa decision Suport framework to address decisional conflict. Ottawa Hosp. Res. Inst. Available at: https://decisionaid.ohri.ca/docs/develop/ODSF.pdf.
Hoenigl M, Weibel N, Mehta SR, Anderson CM, Jenks J, Green N, et al. Development and validation of the San Diego early test score to predict acute and early HIV infection risk in men who have sex with men. Clin Infect Dis. 2015;61(3):468–75.
Krakower D, Powell VE, Maloney K, Wong JB, Wilson IB, Mayer K. Impact of a Personalized Clinical Decision Aid on Informed Decision-Making about HIV Preexposure Prophylaxis among Men who have Sex with Men. 2018. 13th International Conference on HIV Treatment and Prevention Adherence. Miami, FL. 2018;8–10.
Powell VE, Mayer K, Maloney KM, Wong JB, Wilson IB, Krakower D. Impact of a Clinical Decision Aid for Prescribing HIV Preexposure Prophylaxis to Men who have Sex with Men on Primary Care Provider Knowledge and Intentions. 2018. 13th International Conference on HIV Treatment and Prevention Adherence. Miami, FL. 2018;8–10.
NIH Research Portfolio Online Reporting Tools (RePORT). 5R01MD013565. Offering women PrEP with education, shared decision-making and trauma-informed care: the OPENS Trial. Available at: https://projectreporter.nih.gov/project_info_description.cfm?aid=9892890&icde=51187754&ddparam=&ddvalue=&ddsub=&cr=1&csb=default&cs=ASC&pball=.
• Skolnik AA, Bokhour BG, Gifford AL, Wilson BM, Van Epps P. Roadblocks to PrEP: What medical records reveal about access to HIV pre-exposure prophylaxis. J Gen Intern Med. 2020;35(3):832–8. https://doi.org/10.1007/s11606-019-05475-9. In this qualitative study of clinic notes from the Veterans Health Affairs system, nearly all (94%) of PrEP conversations were initiated by patients, one-third of patients experienced delays receiving PrEP, and 70% of patients faced barriers to accessing PrEP. Barriers to PrEP included provider knowledge gaps about PrEP, confusion or disagreement over clinic purview for PrEP, and stigma associated with patients seeking PrEP. These results indicate a need to improve providers’ skills in communicating with patients about PrEP and prescribing to those patients who decide to initiate PrEP.
• Patel RR, Chan PA, Harrison LC, Mayer KH, Nunn A, Mena LA, et al. Missed opportunities to prescribe HIV pre-exposure prophylaxis by primary care providers in Saint Louis, Missouri. LGBT Health. 2018;5(4):250–6 This study found that nearly half of the patients seeking PrEP at an academic infectious diseases clinic in St. Louis, Missouri had previously asked their primary care providers about PrEP but were not prescribed it. These findings suggest that there are many missed opportunities for patient-led decision-making for PrEP in primary care.
Funding
This publication was made possible with the support from the Harvard University Center for AIDS Research, an NIH-funded program (P30 AI060354), the National Institute of Allergy and Infectious Diseases (K01 AI122853 to JLM), and Harvard Pilgrim Health Care Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Douglas Krakower has conducted research with project support from Gilead Sciences; has received honoraria for authoring or presenting continuing medical education content for Medscape, MED-IQ, and DKBMed; and has received royalties for authoring content for UpToDate, Inc. Julia Marcus has consulted for Kaiser Permanente Northern California on a research grant from Gilead Sciences. Whitney Sewell, Patricia Solleveld, Christine Dehlendorf and Dominika Seidman declare no conflicts.
Human and Animal Rights and Informed Consent
All reported studies with human subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Implementation Science
Rights and permissions
About this article
Cite this article
Sewell, W.C., Solleveld, P., Seidman, D. et al. Patient-Led Decision-Making for HIV Preexposure Prophylaxis. Curr HIV/AIDS Rep 18, 48–56 (2021). https://doi.org/10.1007/s11904-020-00535-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-020-00535-w