Abstract
Purpose of Review
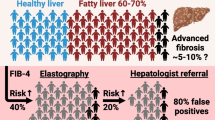
Aging-related comorbidities, including liver disease, represent the main drivers of morbidity and mortality in people with HIV (PWH). Nonalcoholic fatty liver disease (NAFLD) seems a frequent comorbidity in aging PWH nowadays. NAFLD results from a fat deposition into the liver parenchyma that may evolve to nonalcoholic steatohepatitis (NASH), a state of hepatocellular inflammation and injury in response to the accumulated fat leading to liver fibrosis and cirrhosis. We here review the current status of knowledge regarding this emerging comorbidity in PWH.
Recent Findings
Recent studies suggest that PWH are at higher risk for both NASH and NASH-related liver fibrosis. Several hypothesized pathogenic mechanisms may account for this finding, including increased metabolic comorbidities, hepatotoxic effect of lifelong antiretroviral therapy, and chronic HIV infection. In clinical practice, non-invasive diagnostic tests, such as serum biomarkers and elastography, may help identify patients with NASH-related fibrosis, thus improving risk stratification, and enhancing clinical management decisions, including early initiation of interventions such as lifestyle changes and potential pharmacologic interventions.
Summary
Clinicians should remain informed of the frequency, significance, and diagnostic and management approach to NASH in PWH.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Organization WH. https://www.who.int/gho/hiv/en/. Accessed 9 May 2020.
CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2015. HIV Surveillance Supplemental Report. 2017;22(2).
Lloyd-Smith E, Brodkin E, Wood E, Kerr T, Tyndall MW, Montaner JS, et al. Impact of HAART and injection drug use on life expectancy of two HIV-positive cohorts in British Columbia. AIDS. 2006;20(3):445–50.
Fang CT, Chang YY, Hsu HM, Twu SJ, Chen KT, Lin CC, et al. Life expectancy of patients with newly-diagnosed HIV infection in the era of highly active antiretroviral therapy. Qjm. 2007;100(2):97–105.
Lewden C, May T, Rosenthal E, Burty C, Bonnet F, Costagliola D, et al. Changes in causes of death among adults infected by HIV between 2000 and 2005: the “Mortalite 2000 and 2005” surveys (ANRS EN19 and Mortavic). J Acquir Immune Defic Syndr. 2008;48(5):590–8.
Smith CJ, Ryom L, Weber R, Morlat P, Pradier C, Reiss P, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet. 2014;384(9939):241–8.
Palmer AK, Klein MB, Raboud J, Cooper C, Hosein S, Loutfy M, et al. Cohort profile: the Canadian Observational Cohort collaboration. Int J Epidemiol. 2011;40(1):25–32.
Rosenthal E, Salmon-Ceron D, Lewden C, Bouteloup V, Pialoux G, Bonnet F, et al. Liver-related deaths in HIV-infected patients between 1995 and 2005 in the French GERMIVIC Joint Study Group Network (Mortavic 2005 study in collaboration with the Mortalite 2005 survey, ANRS EN19). HIV Med. 2009;10(5):282–9.
Sahasrabuddhe VV, Shiels MS, McGlynn KA, Engels EA. The risk of hepatocellular carcinoma among individuals with acquired immunodeficiency syndrome in the United States. Cancer. 2012.
• Kaspar MB, Sterling RK. Mechanisms of liver disease in patients infected with HIV. BMJ Open Gastroenterol. 2017;4(1):e000166 This is a comprehensive review focusing on pathogenic mechanisms of liver disease in the specific setting of HIV infection, including NAFLD.
Organization WH. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization; 2013. https://www.who.int/bulletin/volumes/97/2/18-213777/en/. Accessed 9 May 2020.
Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140(1):124–31.
Pagano G, Pacini G, Musso G, Gambino R, Mecca F, Depetris N, et al. Nonalcoholic steatohepatitis, insulin resistance, and metabolic syndrome: further evidence for an etiologic association. Hepatology. 2002;35(2):367–72.
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50(8):1844–50.
Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53(2):372–84.
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55(6):2005–23.
Udompap P, Kim D, Kim WR. Current and future burden of chronic nonmalignant liver disease. Clin Gastroenterol Hepatol. 2015;13(12):2031–41.
Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141(4):1249–53.
Wong RJ, Aguilar M, Cheung R, Perumpail RB, Harrison SA, Younossi ZM, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547–55.
Younossi ZM. The epidemiology of nonalcoholic steatohepatitis. Clin Liver Dis (Hoboken). 2018;11(4):92–4.
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–21.
Taylor RS, Taylor RJ, Bayliss S, Hagstrom H, Nasr P, Schattenberg JM, et al. Association between fibrosis stage and outcomes of patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Gastroenterology. 2020;158(6):1611–25 e12.
Bedossa P, Consortium FP. Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology. 2014;60(2):565–75.
•• Maurice JB, Patel A, Scott AJ, Patel K, Thursz M, Lemoine M. Prevalence and risk factors of nonalcoholic fatty liver disease in HIV-monoinfection. AIDS. 2017;31(11):1621–32 This meta-analysis of 10 studies reports on prevalence and predictors of NAFLD, NASH, and liver fibrosis in HIV mono-infected patients.
Guaraldi G, Squillace N, Stentarelli C, Orlando G, D’Amico R, Ligabue G, et al. Nonalcoholic fatty liver disease in HIV-infected patients referred to a metabolic clinic: prevalence, characteristics, and predictors. Clin Infect Diseases : an official publication of the Infectious Diseases Society of America. 2008;47(2):250–7.
Nishijima T, Gatanaga H, Shimbo T, Komatsu H, Nozaki Y, Nagata N, et al. Traditional but not HIV-related factors are associated with nonalcoholic fatty liver disease in Asian patients with HIV-1 infection. PLoS One. 2014;9(1):e87596.
Macias J, Gonzalez J, Tural C, Ortega-Gonzalez E, Pulido F, Rubio R, et al. Prevalence and factors associated with liver steatosis as measured by transient elastography with controlled attenuation parameter in HIV-infected patients. AIDS. 2014;28(9):1279–87.
Lui G, Wong VW, Wong GL, Chu WC, Wong CK, Yung IM, et al. Liver fibrosis and fatty liver in Asian HIV-infected patients. Aliment Pharmacol Ther. 2016;44(4):411–21.
Lombardi R, Lever R, Smith C, Marshall N, Rodger A, Bhagani S, et al. Liver test abnormalities in patients with HIV mono-infection: assessment with simple noninvasive fibrosis markers. Ann Gastroenterol. 2017;30(3):349–56.
Price JC, Ma Y, Scherzer R, Korn N, Tillinghast K, Peters MG, et al. Human immunodeficiency virus-infected and uninfected adults with non-genotype 3 hepatitis C virus have less hepatic steatosis than adults with neither infection. Hepatology. 2017;65(3):853–63.
Lemoine M, Barbu V, Girard PM, Kim M, Bastard JP, Wendum D, et al. Altered hepatic expression of SREBP-1 and PPARgamma is associated with liver injury in insulin-resistant lipodystrophic HIV-infected patients. AIDS. 2006;20(3):387–95.
Crum-Cianflone N, Collins G, Medina S, Asher D, Campin R, Bavaro M, et al. Prevalence and factors associated with liver test abnormalities among human immunodeficiency virus-infected persons. Clin Gastroenterol Hepatol. 2010;8(2):183–91.
Ingiliz P, Valantin MA, Duvivier C, Medja F, Dominguez S, Charlotte F, et al. Liver damage underlying unexplained transaminase elevation in human immunodeficiency virus-1 mono-infected patients on antiretroviral therapy. Hepatology. 2009;49(2):436–42.
Sterling RK, Smith PG, Brunt EM. Hepatic steatosis in human immunodeficiency virus: a prospective study in patients without viral hepatitis, diabetes, or alcohol abuse. J Clin Gastroenterol. 2013;47(2):182–7.
Morse CG, McLaughlin M, Matthews L, Proschan M, Thomas F, Gharib AM, et al. Nonalcoholic steatohepatitis and hepatic fibrosis in HIV-1-monoinfected adults with elevated aminotransferase levels on antiretroviral therapy. Clin Infect Dis. 2015;60(10):1569–78.
• Vodkin I, Valasek MA, Bettencourt R, Cachay E, Loomba R. Clinical, biochemical and histological differences between HIV-associated NAFLD and primary NAFLD: a case-control study. Aliment Pharmacol Ther. 2015;41(4):368–78 This is the only case–control study comparing features of HIV-associated NAFLD and HIV-negative NAFLD. It showed that HIV-associated NAFLD has increased severity of liver disease and higher prevalence of NASH.
Vuille-Lessard E, Lebouche B, Lennox L, Routy JP, Costiniuk CT, Pexos C, et al. Nonalcoholic fatty liver disease diagnosed by transient elastography with controlled attenuation parameter in unselected HIV monoinfected patients. AIDS. 2016;30(17):2635–43.
Lombardi R, Sambatakou H, Mariolis I, Cokkinos D, Papatheodoridis GV, Tsochatzis EA. Prevalence and predictors of liver steatosis and fibrosis in unselected patients with HIV mono-infection. Dig Liver Dis. 2016;48(12):1471–7.
Prat LI, Roccarina D, Lever R, Lombardi R, Rodger A, Hall A, et al. Aetiology and severity of liver disease in HIV positive patients with suspected NAFLD: lessons from a cohort with available liver biopsies. J Acquir Immune Defic Syndr 2018.
Mohr R, Boesecke C, Dold L, Schierwagen R, Schwarze-Zander C, Wasmuth JC, et al. Return-to-health effect of modern combined antiretroviral therapy potentially predisposes HIV patients to hepatic steatosis. Medicine. 2018;97(17):e0462.
Perazzo H, Cardoso SW, Yanavich C, Nunes EP, Morata M, Gorni N, et al. Predictive factors associated with liver fibrosis and steatosis by transient elastography in patients with HIV mono-infection under long-term combined antiretroviral therapy. J Int AIDS Soc. 2018;21(11):e25201.
Benmassaoud A, Ghali P, Cox J, Wong P, Szabo J, Deschenes M, et al. Screening for nonalcoholic steatohepatitis by using cytokeratin 18 and transient elastography in HIV mono-infection. PLoS One. 2018;13(1):e0191985.
Feldstein AE, Wieckowska A, Lopez AR, Liu YC, Zein NN, McCullough AJ. Cytokeratin-18 fragment levels as noninvasive biomarkers for nonalcoholic steatohepatitis: a multicenter validation study. Hepatology. 2009;50(4):1072–8.
Rivero-Juarez A, Camacho A, Merchante N, Perez-Camacho I, Macias J, Ortiz-Garcia C, et al. Incidence of liver damage of uncertain origin in HIV patients not co-infected with HCV/HBV. PLoS One. 2013;8(7):e68953.
Sebastiani G, Rollet-Kurhajec KC, Pexos C, Gilmore N, Klein MB. Incidence and predictors of hepatic steatosis and fibrosis by serum biomarkers in a large cohort of human immunodeficiency virus mono-infected patients. Open forum Infect Diseases. 2015;2(1):ofv015.
• Pembroke T, Deschenes M, Lebouche B, Benmassaoud A, Sewitch M, Ghali P, et al. Hepatic steatosis progresses faster in HIV mono-infected than HIV/HCV co-infected patients and is associated with liver fibrosis. J Hepatol. 2017;67(4):801–8 One of the very few studies investigating the natural history of fatty liver in HIV-infected patients. In particular, they found that HIV mono-infected patients have faster fatty liver progression than HIV/HCV co-infected patients.
Lallukka-Bruck S, Isokuortti E, Luukkonen PK, Hakkarainen A, Lundbom N, Sutinen J, et al. Natural course of nonalcoholic fatty liver disease and type 2 diabetes in patients with human immunodeficiency virus with and without combination antiretroviral therapy-associated lipodystrophy: a 16-year follow-up study. Clin Infect Dis. 2020;70(8):1708–16.
Gariani K, Philippe J, Jornayvaz FR. Non-alcoholic fatty liver disease and insulin resistance: from bench to bedside. Diabetes Metab. 2013;39(1):16–26.
Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55(7):434–8.
Diehl AM, Goodman Z, Ishak KG. Alcohollike liver disease in nonalcoholics. A clinical and histologic comparison with alcohol-induced liver injury. Gastroenterology. 1988;95(4):1056–62.
de Ledinghen V, Vergniol J, Gonzalez C, Foucher J, Maury E, Chemineau L, et al. Screening for liver fibrosis by using FibroScan((R)) and FibroTest in patients with diabetes. Dig Liver Dis. 2012;44(5):413–8.
Kwok R, Choi KC, Wong GL, Zhang Y, Chan HL, Luk AO, et al. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: a prospective cohort study. Gut. 2016;65(8):1359–68.
Doycheva I, Cui J, Nguyen P, Costa EA, Hooker J, Hofflich H, et al. Non-invasive screening of diabetics in primary care for NAFLD and advanced fibrosis by MRI and MRE. Aliment Pharmacol Ther. 2016;43(1):83–95.
European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–402.
Introduction. Standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S1-S2.
Brown TT, Cole SR, Li X, Kingsley LA, Palella FJ, Riddler SA, et al. Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern Med. 2005;165(10):1179–84.
Guaraldi G, Lonardo A, Maia L, Palella FJ Jr. Metabolic concerns in aging HIV-infected persons: from serum lipid phenotype to fatty liver. AIDS. 2017;31(Suppl 2):S147–S56.
Feeney ER, Mallon PW. HIV and HAART-associated dyslipidemia. Open Cardiovasc Med J. 2011;5:49–63.
Hadigan C, Meigs JB, Corcoran C, Rietschel P, Piecuch S, Basgoz N, et al. Metabolic abnormalities and cardiovascular disease risk factors in adults with human immunodeficiency virus infection and lipodystrophy. Clin Infect Dis. 2001;32(1):130–9.
Crum-Cianflone N, Roediger MP, Eberly L, Headd M, Marconi V, Ganesan A, et al. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PLoS One. 2010;5(4):e10106.
•• Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–57 These are clinically useful guidelines about all major aspects of NAFLD including disease definitions and treatment recommendations.
Ivanov AV, Valuev-Elliston VT, Ivanova ON, Kochetkov SN, Starodubova ES, Bartosch B, et al. Oxidative stress during HIV infection: mechanisms and consequences. Oxidative Med Cell Longev. 2016;2016:8910396.
Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40(12):1461–5.
Dold L, Luda C, Schwarze-Zander C, Boesecke C, Hansel C, Nischalke HD, et al. Genetic polymorphisms associated with fatty liver disease and fibrosis in HIV positive patients receiving combined antiretroviral therapy (cART). PLoS One. 2017;12(6):e0178685.
Polyzos SA, Kountouras J, Mantzoros CS. Adipokines in nonalcoholic fatty liver disease. Metab Clin Exp. 2016;65(8):1062–79.
Boursier J, Diehl AM. Nonalcoholic fatty liver disease and the gut microbiome. Clin Liver Dis. 2016;20(2):263–75.
Zevin AS, McKinnon L, Burgener A, Klatt NR. Microbial translocation and microbiome dysbiosis in HIV-associated immune activation. Curr Opin HIV AIDS. 2016;11(2):182–90.
Kazankov K, Barrera F, Moller HJ, Rosso C, Bugianesi E, David E, et al. The macrophage activation marker sCD163 is associated with morphological disease stages in patients with non-alcoholic fatty liver disease. Liver Int. 2016;36(10):1549–57.
Lemoine M, Lacombe K, Bastard JP, Sebire M, Fonquernie L, Valin N, et al. Metabolic syndrome and obesity are the cornerstones of liver fibrosis in HIV-monoinfected patients: results of the METAFIB study. AIDS. 2017;31:1955–64.
Kirkegaard-Klitbo DM, Mejer N, Knudsen TB, Moller HJ, Moestrup SK, Poulsen SD, et al. Soluble CD163 predicts incident chronic lung, kidney and liver disease in HIV infection. AIDS. 2017;31(7):981–8.
Kovari H, Weber R. Influence of antiretroviral therapy on liver disease. Curr Opin HIV AIDS. 2011;6(4):272–7.
Kong L, Cardona Maya W, Moreno-Fernandez ME, Ma G, Shata MT, Sherman KE, et al. Low-level HIV infection of hepatocytes. Virol J. 2012;9:157.
El-Sadr WM, Lundgren JD, Neaton JD, Gordin F, Abrams D, Arduino RC, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355(22):2283–96.
Singhania R, Kotler DP. Lipodystrophy in HIV patients: its challenges and management approaches. HIV AIDS (Auckl). 2011;3:135–43.
Falutz J. Management of fat accumulation in patients with HIV infection. Curr HIV/AIDS Rep. 2011;8(3):200–8.
Ryan P, Blanco F, Garcia-Gasco P, Garcia-Merchan J, Vispo E, Barreiro P, et al. Predictors of severe hepatic steatosis using abdominal ultrasound in HIV-infected patients. HIV Med. 2009;10(1):53–9.
Nunez M. Clinical syndromes and consequences of antiretroviral-related hepatotoxicity. Hepatology. 2010;52(3):1143–55.
Sulkowski MS, Mehta SH, Chaisson RE, Thomas DL, Moore RD. Hepatotoxicity associated with protease inhibitor-based antiretroviral regimens with or without concurrent ritonavir. AIDS. 2004;18(17):2277–84.
Sulkowski MS, Mehta SH, Torbenson M, Afdhal NH, Mirel L, Moore RD, et al. Hepatic steatosis and antiretroviral drug use among adults coinfected with HIV and hepatitis C virus. AIDS. 2005;19(6):585–92.
Eron JJ, Young B, Cooper DA, Youle M, Dejesus E, Andrade-Villanueva J, et al. Switch to a raltegravir-based regimen versus continuation of a lopinavir-ritonavir-based regimen in stable HIV-infected patients with suppressed viraemia (SWITCHMRK 1 and 2): two multicentre, double-blind, randomised controlled trials. Lancet. 2010;375(9712):396–407.
Bourgi K, Rebeiro PF, Turner M, Castilho JL, Hulgan T, Raffanti SP, et al. Greater weight gain in treatment naive persons starting dolutegravir-based antiretroviral therapy. Clin Infect Dis. 2019.
Cervo A, Milic J, Mazzola G, Schepis F, Petta S, Krahn T, Lebouche B, Deschenes M, Cascio A, Guaraldi G, Sebastiani G Prevalence, predictors and severity of lean non-alcoholic fatty liver disease in HIV-infected patients. Clin Infect Dis 2020.
Dulai PS, Singh S, Patel J, Soni M, Prokop LJ, Younossi Z, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65(5):1557–65.
Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13(4):643–54 e1–9; quiz e39–40.
Cai J, Sebastiani G. HIV, elevated transaminases, fatty liver: the perfect storm? J Acquir Immune Defic Syndr. 2019;81(1):e23–e5.
Cai J, Osikowicz M, Sebastiani G. Clinical significance of elevated liver transaminases in HIV-infected patients. AIDS. 2019;33(8):1267–82.
Allen AM, Therneau TM, Larson JJ, Coward A, Somers VK, Kamath PS. Nonalcoholic fatty liver disease incidence and impact on metabolic burden and death: a 20 year-community study. Hepatology. 2018;67(5):1726–36.
Benmassaoud A, Nitulescu R, Pembroke T, Halme AS, Ghali P, Deschenes M, et al. Liver-related events in human immunodeficiency virus-infected persons with occult cirrhosis. Clin Infect Dis. 2019;69(8):1422–30.
Akuta N, Kawamura Y, Arase Y, Saitoh S, Fujiyama S, Sezaki H, et al. Hepatocellular carcinoma is the most common liver-related complication in patients with histopathologically-confirmed NAFLD in Japan. BMC Gastroenterol. 2018;18(1):165.
Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. 2017;66(6):1138–53.
Valenti L, Fracanzani AL, Fargion S. The immunopathogenesis of alcoholic and nonalcoholic steatohepatitis: two triggers for one disease? Semin Immunopathol. 2009;31(3):359–69.
Golabi P, Otgonsuren M, Cable R, Felix S, Koenig A, Sayiner M, et al. Non-alcoholic fatty liver disease (NAFLD) is associated with impairment of health related quality of life (HRQOL). Health Qual Life Outcomes. 2016;14:18.
Sebastiani G, Alshaalan R, Wong P, Rubino M, Salman A, Metrakos P, et al. Prognostic value of non-invasive fibrosis and steatosis tools, hepatic venous pressure gradient (HVPG) and histology in nonalcoholic steatohepatitis. PLoS One. 2015;10(6):e0128774.
Sinn DH, Kang D, Jang HR, Gu S, Cho SJ, Paik SW, et al. Development of chronic kidney disease in patients with non-alcoholic fatty liver disease: a cohort study. J Hepatol. 2017;67(6):1274–80.
Petta S, Valenti L, Marchesini G, Di Marco V, Licata A, Camma C, et al. PNPLA3 GG genotype and carotid atherosclerosis in patients with non-alcoholic fatty liver disease. PLoS One. 2013;8(9):e74089.
Weinstein G, Zelber-Sagi S, Preis SR, Beiser AS, De Carli C, Speliotes EK, et al. Association of nonalcoholic fatty liver disease with lower brain volume in healthy middle-aged adults in the Framingham Study. JAMA Neurol. 2017.
Mantovani A, Byrne CD, Bonora E, Targher G. Nonalcoholic fatty liver disease and risk of incident type 2 diabetes: a meta-analysis. Diabetes Care. 2018;41(2):372–82.
Boyd MA, Mocroft A, Ryom L, Monforte AD, Sabin C, El-Sadr WM, et al. Cardiovascular disease (CVD) and chronic kidney disease (CKD) event rates in HIV-positive persons at high predicted CVD and CKD risk: a prospective analysis of the D:A:D observational study. PLoS Med. 2017;14(11):e1002424.
Saylor D, Dickens AM, Sacktor N, Haughey N, Slusher B, Pletnikov M, et al. HIV-associated neurocognitive disorder - pathogenesis and prospects for treatment. Nat Rev Neurol. 2016;12(5):309.
Triant VA. Cardiovascular disease and HIV infection. Curr HIV/AIDS Rep. 2013;10(3):199–206.
Krahn T, Martel M, Sapir-Pichhadze R, Kronfli N, Falutz J, Guaraldi G, et al. Non-alcoholic fatty liver disease predicts development of metabolic comorbidities in HIV-infected patients. J Infect Dis. 2020;222:787–97.
Ryom L, Boesecke C, Bracchi M, Ambrosioni J, Pozniak A, Arribas J, et al. Highlights of the 2017 European AIDS Clinical Society (EACS) Guidelines for the treatment of adult HIV-positive persons version 9.0. HIV Med. 2018;19(5):309–15.
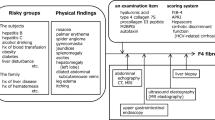
Sebastiani G, Cocciolillo S, Mazzola G, Malagoli A, Falutz J, Cervo A, et al. Application of guidelines for the management of nonalcoholic fatty liver disease in three prospective cohorts of HIV-monoinfected patients. HIV Med. 2020;21(2):96–108.
Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40(6):1387–95.
Gawrieh S, Wilson LA, Cummings OW, Clark JM, Loomba R, Hameed B, et al. Histologic findings of advanced fibrosis and cirrhosis in patients with nonalcoholic fatty liver disease who have normal aminotransferase levels. Am J Gastroenterol. 2019;114(10):1626–35.
Sebastiani G, Gkouvatsos K, Plebani M. Non-invasive assessment of liver fibrosis: it is time for laboratory medicine. Clin Chem Lab Med : CCLM / FESCC. 2011;49(1):13–32.
Myers RP, Fong A, Shaheen AA. Utilization rates, complications and costs of percutaneous liver biopsy: a population-based study including 4275 biopsies. Liver Int : official journal of the International Association for the Study of the Liver. 2008;28(5):705–12.
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. Liver biopsy. Hepatology. 2009;49(3):1017–44.
Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156(5):1264–81 e4.
Price JC, Dodge JL, Ma Y, Scherzer R, Korn N, Tillinghast K, et al. Controlled attenuation parameter and magnetic resonance spectroscopy-measured liver steatosis are discordant in obese HIV-infected adults. AIDS. 2017;31(15):2119–25.
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–402.
Morse CG, McLaughlin M, Proschan M, Koh C, Kleiner DE, Heller T, et al. Transient elastography for the detection of hepatic fibrosis in HIV-monoinfected adults with elevated aminotransferases on antiretroviral therapy. AIDS. 2015;29(17):2297–302.
Sebastiani G, Alberti A. How far is noninvasive assessment of liver fibrosis from replacing liver biopsy in hepatitis C? J Viral Hepat. 2012;19(Suppl 1):18–32.
Sebastiani G. Non-invasive assessment of liver fibrosis in chronic liver diseases: implementation in clinical practice and decisional algorithms. World J Gastroenterol. 2009;15(18):2190–203.
Myers RP, Shah H, Burak KW, Cooper C, Feld JJ. An update on the management of chronic hepatitis C: 2015 Consensus guidelines from the Canadian Association for the Study of the Liver. Can J Gastroenterol Hepatol. 2015;29(1):19–34.
•• Lemoine M, Assoumou L, De Wit S, Girard PM, Valantin MA, Katlama C, et al. Diagnostic accuracy of noninvasive markers of steatosis, NASH, and liver fibrosis in HIV-monoinfected individuals at risk of nonalcoholic fatty liver disease (NAFLD): results from the ECHAM Study. J Acquir Immune Defic Syndr. 2019;80(4):e86–94 The only study that assessed the accuracy of several non-invasive methods for the diagnosis of NAFLD, NASH, and liver fibrosis in HIV mono-infected patients, using liver histology as the reference.
Kirkegaard-Klitbo DM, Bendtsen F, Lundgren J, Nielsen SD, Benfield T, group Cs. Poor concordance between liver stiffness and noninvasive fibrosis scores in HIV infection without viral hepatitis. Clin Gastroenterol Hepatol. 2019;S1542-3565(19):31169–3.
de Franchis R, Baveno VIF. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–52.
Merchante N, Saroli Palumbo C, Mazzola G, Pineda JA, Tellez F, Rivero-Juarez A, et al. Prediction of esophageal varices by liver stiffness and platelets in persons with HIV infection and compensated advanced chronic liver disease. Clin Infect Dis. 2019.
Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367–78 e5 quiz e14–5.
Zelber-Sagi S, Ivancovsky-Wajcman D, Fliss Isakov N, Webb M, Orenstein D, Shibolet O, et al. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J Hepatol. 2018;68(6):1239–46.
Properzi C, O’Sullivan TA, Sherriff JL, Ching HL, Jeffrey GP, Buckley RF, et al. Ad libitum Mediterranean and low-fat diets both significantly reduce hepatic steatosis: a randomized controlled trial. Hepatology. 2018;68(5):1741–54.
Piconi S, Foschi A, Malagoli A, Carli F, Zona S, Milic J, et al. Impact of prolonged maraviroc treatment on non-AIDS-related comorbidities in HIV-positive patients: a retrospective cohort study. J Antimicrob Chemother. 2019;74(9):2723–31.
Macias J, Mancebo M, Merino D, Tellez F, Montes-Ramirez ML, Pulido F, et al. Changes in liver steatosis after switching from efavirenz to raltegravir among human immunodeficiency virus-infected patients with nonalcoholic fatty liver disease. Clin Infect Dis. 2017;65(6):1012–9.
•• Guaraldi G, Maurice JB, Marzolini C, Monteith K, Milic J, Tsochatzis E, et al. New drugs for NASH and HIV infection: great expectations for a great need. Hepatology. 2020;71(5):1831–44 This is an opinion paper about pharmacologic treatments for NASH, either already available or under investigation, focused on HIV-infected population. It highlights the aspect of drug–drug interactions with antiretroviral therapy and supports the need for wider inclusion of this population in large trials.
Matthews L, Kleiner DE, Chairez C, McManus M, Nettles MJ, Zemanick K, et al. Pioglitazone for hepatic steatosis in HIV/hepatitis C virus coinfection. AIDS Res Hum Retrovir. 2015;31(10):961–6.
Ajmera VH, Cachay E, Ramers C, Vodkin I, Bassirian S, Singh S, et al. MRI assessment of treatment response in HIV-associated NAFLD: a randomized trial of a stearoyl-coenzyme-A-desaturase-1 inhibitor (ARRIVE Trial). Hepatology. 2019;70(5):1531–45.
• Sebastiani G, Saeed S, Lebouche B, de Pokomandy A, Szabo J, Haraoui LP, et al. Vitamin E is an effective treatment for nonalcoholic steatohepatitis in HIV mono-infected patients. AIDS, 2020;34(2):237–44 This study shows that vitamin E supplementation, administered at the dose recommended in HIV-negative NASH, improves significantly liver transaminases and fatty liver in HIV mono-infected patients with NASH.
Stanley TL, Fourman LT, Feldpausch MN, Purdy J, Zheng I, Pan CS, et al. Effects of tesamorelin on non-alcoholic fatty liver disease in HIV: a randomised, double-blind, multicentre trial. Lancet HIV. 2019;6(12):e821–e30.
Sharma P, McCarty TR, Ngu JN, O’Donnell M, Njei B. Impact of bariatric surgery in patients with HIV infection: a nationwide inpatient sample analysis, 2004-2014. AIDS. 2018;32(14):1959–65.
Amouyal C, Buyse M, Lucas-Martini L, Hirt D, Genser L, Torcivia A, et al. Sleeve gastrectomy in morbidly obese HIV patients: focus on anti-retroviral treatment absorption after surgery. Obes Surg. 2018;28(9):2886–93.
Funding
GS is supported by a Junior 1 and 2 Salary Award from FRQS (#27127 and #267806) and research salary from the Department of Medicine of McGill University.
Author information
Authors and Affiliations
Contributions
AC contributed to the conception, study design, data, and interpretation of the data. GS contributed to the conception, study design, data, and interpretation of the data and first draft of the manuscript. MS and KP contributed to the interpretation of data. All authors approved the final version of the article.
Corresponding author
Ethics declarations
Conflict of Interest
KP is an advisory board/consultant for Gilead Sciences, Intercept, Novartis, and Eli Lilly, and received research funding from Gilead Sciences. GS has acted as speaker for Merck, Gilead, Abbvie, Novonordisk, and Novartis, served as an advisory board member for Merck, Novartis, Gilead, and Intercept, and has received unrestricted research funding from Merck and Theratec. AC and MS have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Co-infections and Comorbidity
Rights and permissions
About this article
Cite this article
Cervo, A., Shengir, M., Patel, K. et al. NASH in HIV. Curr HIV/AIDS Rep 17, 601–614 (2020). https://doi.org/10.1007/s11904-020-00531-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-020-00531-0