Abstract
Purpose of Review
Symptomatic cerebrospinal fluid (CSF) HIV escape defines the presence of neurological disease in combination antiretroviral therapy (cART)-treated persons due to HIV replication in CSF despite systemic suppression or to higher viral replication in CSF than in plasma. The aim was to search for cases of recurrent symptomatic CSF escape and to define their characteristics.
Recent Findings
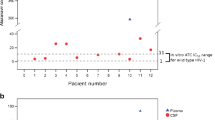
By review of the literature, we identified symptomatic CSF escape relapses in three patients who had shown clinical remission of a first escape episode following cART optimization. By examination of our cohort of 21 patients with symptomatic CSF escape, we identified five additional patients. In the latter, viral escape relapsed over a median follow-up of 108 months because of low adherence or upon treatment simplification of a previously optimized regimen. cART reoptimization based on resistance profile and potential drug neuropenetration and efficacy led to relapse resolution with no further episodes after a median follow-up of 50 months from relapse.
Summary
The observation that CSF escape may relapse highlights the importance of long-term neuro-suppressive regimens after a first episode and supports the role of the brain as a reservoir for HIV.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Mastrangelo A, Turrini F, de Zan Valentina CR, Gerevini S, Cinque P. Symptomatic cerebrospinal fluid escape. AIDS. 2019;33(Suppl 2):S159–69. Extensive review of the published cases of symptomatic cerebrospinal fluid escape.
• Winston A, Antinori A, Cinque P, Fox HS, Gisslen M, Henrich TJ, et al. Defining cerebrospinal fluid HIV RNA escape: editorial review. AIDS. 2019;33(Suppl 2):S107–11. A proposal of consensus definitions for cerebrospinal fluid escape.
• Canestri A, Lescure F-X, Jaureguiberry S, et al. Discordance between cerebral spinal fluid and plasma HIV replication in patients with neurological symptoms who are receiving suppressive antiretroviral therapy. Clin Infect Dis. 2010;50:773–8. First case series describing symptomatic cerebrospinal fluid escape.
Peluso MJ, Ferretti F, Peterson J, Lee E, Fuchs D, Boschini A, et al. Cerebrospinal fluid HIV escape associated with progressive neurologic dysfunction in patients on antiretroviral therapy with well controlled plasma viral load. AIDS. 2012;26:1765–74.
Kugathasan R, Collier DA, Haddow LJ, el Bouzidi K, Edwards SG, Cartledge JD, et al. Diffuse white matter signal abnormalities on magnetic resonance imaging are associated with human immunodeficiency virus type 1 viral escape in the central nervous system among patients with neurological symptoms. Clin Infect Dis. 2017;64:1059–65.
Dravid AN, Natrajan K, Kulkarni MM, et al. Discordant CSF/plasma HIV-1 RNA in individuals on virologically suppressive antiretroviral therapy in Western India. Medicine (Baltimore). 2018;97:e9969.
Wendel KA, McArthur JC. Acute meningoencephalitis in chronic human immunodeficiency virus (HIV) infection: putative central nervous system escape of HIV replication. Clin Infect Dis. 2003;37:1107–11.
Lescure F-X, Moulignier A, Savatovsky J, Amiel C, Carcelain G, Molina JM, et al. CD8 encephalitis in HIV-infected patients receiving cART: a treatable entity. Clin Infect Dis. 2013;57:101–8.
• Gray F, Lescure FX, Adle-Biassette H, Polivka M, Gallien S, Pialoux G, et al. Encephalitis with infiltration by CD8+ lymphocytes in HIV patients receiving combination antiretroviral treatment. Brain Pathol Zurich Switz. 2013;23:525–33. Thorough pathological description of CD8+ cell encephalitis.
Mukerji SS, Misra V, Lorenz D, Cervantes-Arslanian AM, Lyons J, Chalkias S, et al. Temporal patterns and drug resistance in CSF viral escape among ART-experienced HIV-1 infected adults. JAIDS J Acquir Immune Defic Syndr. 2017;75:246–55.
Tong CYW, Costelloe S, Hubb J, Mullen J, O'Shea S, Marta M, et al. Deep sequencing of HIV-1 in cerebrospinal fluid. Clin Infect Dis. 2015;61:1022–5.
Gutmann C, Cusini A, Günthard HF, Fux C, Hirschel B, Decosterd LA, et al. Randomized controlled study demonstrating failure of LPV/r monotherapy in HIV: the role of compartment and CD4-nadir. AIDS. 2010;24:2347–54.
Pasquet A, Ajana F, Melliez H, Giurca C, Poissy J, Yazdanpanah Y. Central nervous system HIV replication and HIV-related pachymeningitis in a patient on protease inhibitor monotherapy despite an undetectable plasma viral load. AIDS. 2012;26:1726–8.
Mangioni D, Muscatello A, Sabbatini F, Soria A, Rossi M, Bisi L, et al. A case of cerebrospinal fluid viral escape on a dual antiretroviral regimen: worth the risk? Clin Infect Dis. 2014;59:1655–6.
Martins J, Santos E, Salgado P, Maia L, Dias D, Marta M, et al. Recurrent cerebrospinal fluid escape in an HIV-1-infected patient receiving antiretroviral therapy. AIDS. 2016;30:1143–4.
Salam S, Mihalova T, Ustianowski A, McKee D, Siripurapu R. Relapsing CD8+ encephalitis-looking for a solution. BMJ Case Rep. 2016; Published online.
Moloney PB, Hutchinson S, Heskin J, Mulcahy F, Langan Y, Conlon NP, et al. Possible N-methyl-D-aspartate receptor antibody-mediated encephalitis in the setting of HIV cerebrospinal fluid escape. J Neurol. 2020;267:1348–52.
Dravid AN, Gawali R, Betha TP, et al. Two treatment strategies for management of neurosymptomatic cerebrospinal fluid HIV escape in Pune, India. Medicine (Baltimore). 2020;99:e20516.
Portegies P, Enting RH, de Gans J, et al. Presentation and course of AIDS dementia complex: 10 years of follow-up in Amsterdam. Netherlands AIDS. 1993;7:669–75.
Vago L, Castagna A, Lazzarin A, Trabattoni G, Cinque P, Costanzi G. Reduced frequency of HIV-induced brain lesions in AIDS patients treated with zidovudine. J Acquir Immune Defic Syndr. 1993;6:42–5.
Gisslén M, Norkrans G, Svennerholm B, Hagberg L. The effect on human immunodeficiency virus type 1 RNA levels in cerebrospinal fluid after initiation of zidovudine or didanosine. J Infect Dis. 1997;175:434–7.
Pierotti C, Nebuloni M, Bestetti A, et al. Presence of nucleotide excision resistance mutations in cerebrospinal fluid is associated with reduced prevalence of HIV-related brain lesions. In: Program and abstracts of the 11th Conference on Retroviruses and Opportunistic Infections (San Francisco). 2004.
Acknowledgments
We wish to thank the colleagues at the Department of Infectious Diseases, San Raffaele Hospital, for help with the patients’ management and follow-up.
Funding
This work was supported by the Italian Gilead Sciences Fellowship Program and by the National Institutes of Health (National Institute of Allergy and Infectious Diseases, R01NS094067-01) to PC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
NG reports personal fees from Gilead Sciences, Janssen Cilag, ViiV Healthcare, and Merck Sharp and Dohme. AL reports personal fees from Gilead Sciences, Janssen Cilag, ViiV Healthcare, and Merck Sharp and Dohme. PC reports personal fees from Gilead Sciences, Janssen Cilag, ViiV Healthcare, Pfizer, and Shire. The remaining authors have no conflict of interest to declare.
Human and Animal Rights and Informed Consent
The patients from our clinic were followed by standard diagnostic and treatment procedures. However, they were part of a study approved by the Ethical Committee of our Institute and gave written permission to the use of clinical data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Central Nervous System and Cognition
Rights and permissions
About this article
Cite this article
Ferretti, F., De Zan, V., Gerevini, S. et al. Relapse of Symptomatic Cerebrospinal Fluid HIV Escape. Curr HIV/AIDS Rep 17, 522–528 (2020). https://doi.org/10.1007/s11904-020-00526-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-020-00526-x