Abstract
Purpose of Review
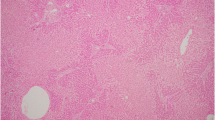
Idiosyncratic drug-induced liver injury (DILI) typically presents acutely with liver test abnormalities, sometimes with associated symptoms of abdominal pain, nausea, vomiting, jaundice, fevers, and rash. Histologic abnormalities in such cases of DILI typically range from lobular or portal hepatitis to hepatocyte necrosis. However, sometimes the drug-related liver injuries present with clinical and/or histological features atypical of garden variety DILI and they may be related to uncommon mechanisms of injury, histologic features, or clinical presentation.
Recent Findings
Multiple agents or classes of agents can result in uncommon forms of liver injury that are phenotypically unique and differ from commonly recognized acute DILI. These include unusual presentations of drugs commonly associated with typical acute DILI, such as drug-induced autoimmune hepatitis. Atypical DILI also includes histologically atypical manifestations of DILI, such as nodular regenerative hyperplasia, sinusoidal obstruction syndrome, granulomatous hepatitis, and steatosis/steatohepatitis.
Summary
Atypical DILI encompasses recognized patterns of injury associated with specific agents or drug classes. These can manifest by atypical biochemical, clinical, and histopathological signatures. An understanding of these types of liver injury is important for the timely recognition of such atypical DILI.
Similar content being viewed by others
Abbreviations
- DILI:
-
Drug-induced liver injury
- DILIN:
-
Drug-Induced Liver Injury Network
- NRH:
-
Nodular regenerative hyperplasia
- SOS:
-
Sinusoidal obstruction syndrome
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, Watkins PB, Navarro V, Barnhart H, Gu J, Serrano J, Ahmad J, Bach N, Bansal M, Barnhart HX, Beavers K, Bonkovsky H, Calvo FO, Chalasani N, Chang C, Conjeevaram H, Conner G, Darling J, de Boer Y, Dieterich D, DiPaola F, Durazo FA, (Jay) Everhart JE, Fontana RJ, Ghabril MS, Goldstein D, Gopalreddy V, Grewal P, Hayashi PH, Hoofnagle J, Kaplowitz N, Liangpunsakul S, Lichtman S, Liu L, Navarro VJ, Odin J, Rossi S, Russo M, Schiano T, Serrano J, Sherker AH, Stolz A, Vuppalanchi R, Watkins P, Zacks S, Balasco A, Chesney K, Corne A, Cummings S, Groseclose G, Hammett A, Hooker J, Kesar V, Mao S, Marks K, McFadden R, Melgoza Y, Mikhail S, Milstein S, Morlan W, Peacock V, Rosado N, Russell T, Vega M, Verma M, Walker P, Yalamanchili R, McClanahan-Crowder M, Galan K, (Sherry) Gu J, Chau T, Ragavan K, Rostami H, Puglisi-Scharenbroich C, Torrance RJ, van Raaphorst R Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology 2015;148:1340–1352 e7.
Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J, Drug Induced Liver Injury Network (DILIN) Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008;135:1924–34, 1934 e1–4, 1934.e4.
Chalasani NP, Hayashi PH, Bonkovsky HL, et al. ACG clinical guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am J Gastroenterol 2014;109:950–66; quiz 967, 966.
Haque T, Sasatomi E, Hayashi PH. Drug-induced liver injury: pattern recognition and future directions. Gut Liver. 2016;10:27–36.
Padda MS, Sanchez M, Akhtar AJ, Boyer JL. Drug-induced cholestasis. Hepatology. 2011;53:1377–87.
Martinez MA, Vuppalanchi R, Fontana RJ, Stolz A, Kleiner DE, Hayashi PH, Gu J, Hoofnagle JH, Chalasani N Clinical and histologic features of azithromycin-induced liver injury. Clin Gastroenterol Hepatol 2015;13:369–376 e3, 376.e3.
Vuppalanchi R, Hayashi PH, Chalasani N, Fontana RJ, Bonkovsky H, Saxena R, et al. Duloxetine hepatotoxicity: a case-series from the drug-induced liver injury network. Aliment Pharmacol Ther. 2010;32:1174–83.
Kleiner DECN, Conjeevaram HS, Bonkovsky H, Russo M, Davern T, McHutchison JG, et al. B for the drug-induced liver injury network (DILIN). Relationship of biochemical variables to histologic findings and the pathological pattern of injury among cases identified in the NIH DILIN study. Gastroenterology. 2007;132
• Kleiner DE, Chalasani NP, Lee WM, Fontana RJ, Bonkovsky HL, Watkins PB, et al. Hepatic histological findings in suspected drug-induced liver injury: systematic evaluation and clinical associations. Hepatology. 2014;59:661–70. This paper summarized the myriad hisotologic presentations of DILI as seen in the course of prospective study.
Rochon J, Protiva P, Seeff LB, Fontana RJ, Liangpunsakul S, Watkins PB, et al. Reliability of the Roussel Uclaf causality assessment method for assessing causality in drug-induced liver injury. Hepatology. 2008;48:1175–83.
Fontana RJ, Hayashi PH, Barnhart H, et al. Persistent liver biochemistry abnormalities are more common in older patients and those with cholestatic drug induced liver injury. Am J Gastroenterol. 2015;110:1450–9.
Elsharkawy AM, McPherson S, Masson S, Burt AD, Dawson RT, Hudson M. Cholestasis secondary to anabolic steroid use in young men. BMJ. 2012;344:e468.
Robles-Diaz M, Gonzalez-Jimenez A, Medina-Caliz I, Stephens C, García-Cortes M, García-Muñoz B, et al. Distinct phenotype of hepatotoxicity associated with illicit use of anabolic androgenic steroids. Aliment Pharmacol Ther. 2015;41:116–25.
Czaja AJ. Drug-induced autoimmune-like hepatitis. Dig Dis Sci. 2011;56:958–76.
Czaja AJ. Acute and acute severe (fulminant) autoimmune hepatitis. Dig Dis Sci. 2013;58:897–914.
Czaja AJ. Review article: the management of autoimmune hepatitis beyond consensus guidelines. Aliment Pharmacol Ther. 2013;38:343–64.
Czaja AJ, Carpenter HA. Progressive fibrosis during corticosteroid therapy of autoimmune hepatitis. Hepatology. 2004;39:1631–8.
Iqbal U, Siddiqui HU, Anwar H, et al. Allopurinol-induced granulomatous hepatitis: a case report and review of literature. J Investig Med High Impact Case Rep. 2017;5:2324709617728302.
Marin Zuluaga JI, Marin Castro AE, Perez Cadavid JC, Restrepo Gutierrez JC. Albendazole-induced granulomatous hepatitis: a case report. J Med Case Rep. 2013;7:201.
Adike A, Smith ML, Chervenak A, Vargas HE. Hydroxycut-related vanishing bile duct syndrome. Clin Gastroenterol Hepatol. 2017;15:142–4.
Balakrishnan A, Ledford R, Jaglal M. Temozolomide-induced biliary ductopenia: a case report. J Med Case Rep. 2016;10:33.
Bhayana H, Appasani S, Thapa BR, Das A, Singh K. Lamotrigine-induced vanishing bile duct syndrome in a child. J Pediatr Gastroenterol Nutr. 2012;55:e147–8.
Bjornsson ES, Jonasson JG. Idiosyncratic drug-induced liver injury associated with bile duct loss and vanishing bile duct syndrome: rare but has severe consequences. Hepatology. 2017;65:1091–3.
• Bonkovsky HL, Kleiner DE, Gu J, Odin JA, Russo MW, Navarro VM, et al. Clinical presentations and outcomes of bile duct loss caused by drugs and herbal and dietary supplements. Hepatology. 2017;65:1267–77. This recent study describes the evolution of vanishing bile duct syndrome in the ourse of drug-induced liver injury and highlights the prognostic impact of the degree of ductpenia.
Robinson W, Habr F, Manlolo J, Bhattacharya B. Moxifloxacin associated vanishing bile duct syndrome. J Clin Gastroenterol. 2010;44:72–3.
Schumaker AL, Okulicz JF. Meropenem-induced vanishing bile duct syndrome. Pharmacotherapy. 2010;30:953.
Tekin F, Celik F, Nart D, Akarca U. The first report of oxcarbazepine-induced vanishing bile duct syndrome. J Gastrointestin Liver Dis. 2014;23:222–3.
Vuppalanchi R, Chalasani N, Saxena R. Restoration of bile ducts in drug-induced vanishing bile duct syndrome due to zonisamide. Am J Surg Pathol. 2006;30:1619–23.
Nijhawan R, Wierzbicki AS, Tozer R, Lascelles PT, Patsalos PN. Antiepileptic drugs, hepatic enzyme induction and raised serum alkaline phosphatase isoenzymes. Int J Clin Pharmacol Res. 1990;10:319–23.
Murphy JV. Valproate-induced hyperammonemic encephalopathy. Epilepsia. 2003;44:268. author reply 268
Satapathy SK, Kuwajima V, Nadelson J, Atiq O, Sanyal A. Drug-induced fatty liver disease: an overview of pathogenesis and management. Ann Hepatol. 2015;14:789–806.
Amacher DE, Chalasani N. Drug-induced hepatic steatosis. Semin Liver Dis. 2014;34:205–14.
Ryan P, Nanji S, Pollett A, Moore M, Moulton CA, Gallinger S, et al. Chemotherapy-induced liver injury in metastatic colorectal cancer: semiquantitative histologic analysis of 334 resected liver specimens shows that vascular injury but not steatohepatitis is associated with preoperative chemotherapy. Am J Surg Pathol. 2010;34:784–91.
Dash A, Figler RA, Sanyal AJ, Wamhoff BR. Drug-induced steatohepatitis. Expert Opin Drug Metab Toxicol. 2017;13:193–204.
Cupido AJ, Reeskamp LF, Kastelein JJP. Novel lipid modifying drugs to lower LDL cholesterol. Curr Opin Lipidol. 2017;28:367–73.
Gouni-Berthold I, Berthold HK. Mipomersen and lomitapide: two new drugs for the treatment of homozygous familial hypercholesterolemia. Atheroscler Suppl. 2015;18:28–34.
Miyares MA. Progression to hepatitis and fibrosis secondary to lomitapide use: selecting the next course of action. JAMA Intern Med. 2014;174:1522.
Rader DJ, Kastelein JJ. Lomitapide and mipomersen: two first-in-class drugs for reducing low-density lipoprotein cholesterol in patients with homozygous familial hypercholesterolemia. Circulation. 2014;129:1022–32.
Ishak KG. Hepatic lesions caused by anabolic and contraceptive steroids. Semin Liver Dis. 1981;1:116–28.
Laurent A, Dokmak S, Nault JC, Pruvot FR, Fabre JM, Letoublon C, et al. European experience of 573 liver resections for hepatocellular adenoma: a cross-sectional study by the AFC-HCA-2013 study group. HPB (Oxford). 2016;18:748–55.
Nault JC, Bioulac-Sage P, Zucman-Rossi J. Hepatocellular benign tumors-from molecular classification to personalized clinical care. Gastroenterology. 2013;144:888–902.
Nault JC, Paradis V, Cherqui D, Vilgrain V, Zucman-Rossi J. Molecular classification of hepatocellular adenoma in clinical practice. J Hepatol. 2017;67:1074–83.
Mays ET, Christopherson W. Hepatic tumors induced by sex steroids. Semin Liver Dis. 1984;4:147–57.
van Aalten SM, de Man RA, JN IJ, et al. Systematic review of haemorrhage and rupture of hepatocellular adenomas. Br J Surg. 2012;99:911–6.
Kudo M. Malignant transformation of hepatocellular adenoma: how frequently does it happen? Liver Cancer. 2015;4:1–5.
Kwok WY, Hagiwara S, Nishida N, Watanabe T, Sakurai T, Ida H, et al. Malignant transformation of hepatocellular adenoma. Oncology. 2017;92(Suppl 1):16–28.
Torbenson M. Hepatic adenomas: classification, controversies, and consensus. Surg Pathol Clin. 2018;11:351–66.
Shapiro P, Ikeda RM, Ruebner BH, Connors MH, Halsted CC, Abildgaard CF. Multiple hepatic tumors and peliosis hepatis in Fanconi's anemia treated with androgens. Am J Dis Child. 1977;131:1104–6.
https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm279174.htm. Volume 2017: FDA, 2017.
Force J, Saxena R, Schneider BP, Storniolo AM, Sledge GW Jr, Chalasani N, et al. Nodular regenerative hyperplasia after treatment with trastuzumab emtansine. J Clin Oncol. 2016;34:e9–e12.
Vuppalanchi R, Saxena R, Storniolo AMV, Chalasani N. Pseudocirrhosis and liver failure in patients with metastatic breast cancer after treatment with palbociclib. Hepatology. 2017;65:1762–4.
Hillaire S, Bonte E, Denninger MH, Casadevall N, Cadranel JF, Lebrec D, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension in the west: a re-evaluation in 28 patients. Gut. 2002;51:275–80.
Steiner PE. Nodular regenerative hyperplasia of the liver. Am J Pathol. 1959;35:943–53.
Nakanuma Y, Hoso M, Sasaki M, et al. Histopathology of the liver in non-cirrhotic portal hypertension of unknown aetiology. Histopathology. 1996;28:195–204.
Shastri S, Dubinsky MC, Fred Poordad F, Vasiliauskas EA, Geller SA. Early nodular hyperplasia of the liver occurring with inflammatory bowel diseases in association with thioguanine therapy. Arch Pathol Lab Med. 2004;128:49–53.
Hartleb M, Gutkowski K, Milkiewicz P. Nodular regenerative hyperplasia: evolving concepts on underdiagnosed cause of portal hypertension. World J Gastroenterol. 2011;17:1400–9.
Naber AH, Van Haelst U, Yap SH. Nodular regenerative hyperplasia of the liver: an important cause of portal hypertension in non-cirrhotic patients. J Hepatol. 1991;12:94–9.
• Ghabril M, Vuppalanchi R. Drug-induced nodular regenerative hyperplasia. Semin Liver Dis 2014;34:240–5. The broad range of agents associated with nodular regenerative hyperplasia are described
• DeLeve LD, Shulman HM, McDonald GB. Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome (veno-occlusive disease). Semin Liver Dis. 2002;22:27–42. This increasingly recognized form of drug-induced liver injury is unusual in its presentation and is well summarized in this review paper.
Kumar S, DeLeve LD, Kamath PS, et al. Hepatic veno-occlusive disease (sinusoidal obstruction syndrome) after hematopoietic stem cell transplantation. Mayo Clin Proc. 2003;78:589–98.
DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of the liver. Hepatology. 2009;49:1729–64.
Hoofnagle JH, Serrano J, Knoben JE, Navarro VJ. LiverTox: a website on drug-induced liver injury. Hepatology. 2013;57:873–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Raj Vuppalanchi and Marwan Ghabril declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Drug-Induced Liver Injury
Rights and permissions
About this article
Cite this article
Vuppalanchi, R., Ghabril, M. Uncommon Presentations of Idiosyncratic Drug-Induced Liver Injury. Curr Hepatology Rep 17, 254–259 (2018). https://doi.org/10.1007/s11901-018-0417-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-018-0417-7