Abstract
Purpose of Review
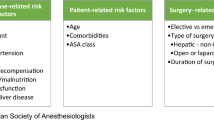
Cirrhotic patients have an increased risk of surgical complications and higher perioperative morbidity and mortality based on the severity of their liver disease. Liver disease predisposes patients to perioperative coagulopathies, volume overload, and encephalopathy. The goal of this paper is to discuss the surgical risk of cirrhotic patients undergoing elective surgeries and to discuss perioperative optimization strategies.
Recent Findings
Literature thus far varies by surgery type and the magnitude of surgical risk. CTP and MELD classification scores allow for the assessment of surgical risk in cirrhotic patients.
Summary
Once the decision has been made to undergo elective surgery, cirrhotic patients can be optimized pre-procedure with the help of a checklist and by the involvement of a multidisciplinary team. Elective surgeries should be performed at hospital centers staffed by healthcare providers experienced in caring for cirrhotic patients. Further research is needed to develop ways to prepare this complicated patient population before elective surgery.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
O'Leary JG, Yachimski PS, Friedman LS. Surgery in the patient with liver disease. Clin Liver Dis. 2009;13(2):211–31. https://doi.org/10.1016/j.cld.2009.02.002.
Patel T. Surgery in the patient with liver disease. Mayo Clin Proc. 1999;74(6):593–9. https://doi.org/10.4065/74.6.593.
Telem DA, Schiano T, Divino CM. Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: management and outcome. Surgery. 2010;148(3):538–43. https://doi.org/10.1016/j.surg.2010.01.002.
Neeff H, Mariaskin D, Spangenberg HC, Hopt UT, Makowiec F. Perioperative mortality after non-hepatic general surgery in patients with liver cirrhosis: an analysis of 138 operations in the 2000s using Child and MELD scores. J Gastrointest Surg. 2011;15(1):1–11. https://doi.org/10.1007/s11605-010-1366-9.
Andraus W, Pinheiro RS, Lai Q, Haddad LBP, Nacif LS, D'Albuquerque LAC, et al. Abdominal wall hernia in cirrhotic patients: emergency surgery results in higher morbidity and mortality. BMC Surg. 2015;15:65. https://doi.org/10.1186/s12893-015-0052-y.
Salamone G, Licari L, Guercio G, Campanella S, Falco N, Scerrino G, et al. The abdominal wall hernia in cirrhotic patients: a historical challenge. World J Emerg Surg. 2018;13:35. https://doi.org/10.1186/s13017-018-0196-z.
Petro CC, Haskins IN, Perez AJ, Tastaldi L, Strong AT, Ilie RN, et al. Hernia repair in patients with chronic liver disease - a 15-year single-center experience. Am J Surg. 2019;217(1):59–65. https://doi.org/10.1016/j.amjsurg.2018.10.020.
•• Im GY, Lubezky N, Facciuto ME, Schiano TD. Surgery in patients with portal hypertension: a preoperative checklist and strategies for attenuating risk. Clin Liver Dis. 2014;18(2):477–505. https://doi.org/10.1016/j.cld.2014.01.006. This paper discusses ways to optimize and manage patients with liver disease undergoing elective surgeries, similar to this review.
• Tan HH, Schiano TD. Effects of liver disease on drug metabolism in humans. In: Encyclopedia of drug metabolism and interactions. Hoboken: John Wiley and Sons; 2013. p. 1–46. This chapter is a comprehensive review of drug metabolism in liver disease.
Cowan RE, Jackson BT, Grainger SL, Thompson RP. Effects of anesthetic agents and abdominal surgery on liver blood flow. Hepatology. 1991;14(6):1161–6.
Afdhal N, McHutchison J, Brown R, Jacobson I, Manns M, Poordad F, et al. Thrombocytopenia associated with chronic liver disease. J Hepatol. 2008;48(6):1000–7. https://doi.org/10.1016/j.jhep.2008.03.009.
Greenwood SM, Leffler CT, Minkowitz S. The increased mortality rate of open liver biopsy in alcoholic hepatitis. Surg Gynecol Obstet. 1972;134(4):600–4.
Powell-Jackson P, Greenway B, Williams R. Adverse effects of exploratory laparotomy in patients with unsuspected liver disease. Br J Surg. 1982;69(8):449–51. https://doi.org/10.1002/bjs.1800690805.
Mikkelsen WP. Therapeutic portacaval shunt. Preliminary data on controlled trial and morbid effects of acute hyaline necrosis. Arch Surg. 1974;108(3):302–5. https://doi.org/10.1001/archsurg.1974.01350270036007.
•• Adamson DT, Bozeman MC, Benns MV, Burton A, Davis EG, Jones CM. Operative considerations for the general surgeon in patients with chronic liver disease. Am Surg. 2019;85(2):234–44. This paper is a comprehensive surgical perspective on the management of liver patients undergoing elective surgeries.
Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1–85.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–9. https://doi.org/10.1002/bjs.1800600817.
Garrison RN, Cryer HM, Howard DA, Polk HC Jr. Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann Surg. 1984;199(6):648–55. https://doi.org/10.1097/00000658-198406000-00003.
Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997;122(4):730–5; discussion 5-6. https://doi.org/10.1016/S0039-6060(97)90080-5.
Telem DA, Schiano T, Goldstone R, Han DK, Buch KE, Chin EH, et al. Factors that predict outcome of abdominal operations in patients with advanced cirrhosis. Clin Gastroenterol Hepatol. 2010;8(5):451–7, quiz e58. https://doi.org/10.1016/j.cgh.2009.12.015.
Costa BP, Sousa FC, Serodio M, Carvalho C. Value of MELD and MELD-based indices in surgical risk evaluation of cirrhotic patients: retrospective analysis of 190 cases. World J Surg. 2009;33(8):1711–9. https://doi.org/10.1007/s00268-009-0093-4.
Gines P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatology. 2008;48(3):1002–10. https://doi.org/10.1002/hep.22418.
Farnsworth N, Fagan SP, Berger DH, Awad SS. Child-Turcotte-Pugh versus MELD score as a predictor of outcome after elective and emergent surgery in cirrhotic patients. Am J Surg. 2004;188(5):580–3. https://doi.org/10.1016/j.amjsurg.2004.07.034.
Wu SL, Zheng YX, Tian ZW, Chen MS, Tan HZ. Scoring systems for prediction of mortality in decompensated liver cirrhosis: a meta-analysis of test accuracy. World J Clin Cases. 2018;6(15):995–1006. https://doi.org/10.12998/wjcc.v6.i15.995.
Goyal SK, Dixit VK, Jain AK, Mohapatra PK, Ghosh JK. Assessment of the model for end-stage liver disease (MELD) score in predicting prognosis of patients with alcoholic hepatitis. J Clin Exp Hepatol. 2014;4(1):19–24. https://doi.org/10.1016/j.jceh.2014.02.006.
• Piotrowski D, Saczewska-Piotrowska A, Jaroszewicz J, Boron-Kaczmarska A. Predictive power of model for end-stage liver disease and Child-Turcotte-Pugh score for mortality in cirrhotic patients. Clin Exp Hepatol. 2018;4(4):240–6. https://doi.org/10.5114/ceh.2018.80125. This paper is a thorough review of the predictive ability of the MELD and CTP scoring systems.
Teh SH, Nagorney DM, Stevens SR, Offord KP, Therneau TM, Plevak DJ, et al. Risk factors for mortality after surgery in patients with cirrhosis. Gastroenterology. 2007;132(4):1261–9. https://doi.org/10.1053/j.gastro.2007.01.040.
Haynes SR, Lawler PG. An assessment of the consistency of ASA physical status classification allocation. Anaesthesia. 1995;50(3):195–9. https://doi.org/10.1111/j.1365-2044.1995.tb04554.x.
• Post-operative mortality risk in patients with cirrhosis. 2019. https://www.mayoclinic.org/medical-professionals/transplant-medicine/calculators/post-operative-mortality-risk-in-patients-with-cirrhosis/itt-20434721. 2019. This is a helpful tool to assess mortality risk in cirrhotic patients undergoing surgery. https://doi.org/10.4062/biomolther.2019.051
Sahara K, Paredes AZ, Tsilimigras DI, Hyer JM, Merath K, Wu L, et al. Impact of liver cirrhosis on perioperative outcomes among elderly patients undergoing hepatectomy: the effect of minimally invasive surgery. J Gastrointest Surg. 2019. https://doi.org/10.1007/s11605-019-04117-z.
Bhangui P, Laurent A, Amathieu R, Azoulay D. Assessment of risk for non-hepatic surgery in cirrhotic patients. J Hepatol. 2012;57(4):874–84. https://doi.org/10.1016/j.jhep.2012.03.037.
Puggioni A, Wong LL. A metaanalysis of laparoscopic cholecystectomy in patients with cirrhosis. J Am Coll Surg. 2003;197(6):921–6. https://doi.org/10.1016/j.jamcollsurg.2003.08.011.
Neri V, Ambrosi A, Di Lauro G, Fersini A, Valentino TP. Difficult cholecystectomies: validity of the laparoscopic approach. JSLS. 2003;7(4):329–33.
Curet MJ, Contreras M, Weber DM, Albrecht R. Laparoscopic cholecystectomy. Surg Endosc. 2002;16(3):453–7. https://doi.org/10.1007/s00464-001-8129-3.
Fernando R. Laparoscopic cholecystectomy. World J Surg. 2002;26(11):1401; author reply -2–1401; author reply 1402. https://doi.org/10.1007/s00268-002-1244-z.
Johnston SM, Kidney S, Sweeney KJ, Zaki A, Tanner WA, Keane FV. Changing trends in the management of gallstone disease. Surg Endosc. 2003;17(5):781–6. https://doi.org/10.1007/s00464-002-9122-1.
Diamond T, Parks RW. Perioperative management of obstructive jaundice. Br J Surg. 1997;84(2):147–9. https://doi.org/10.1002/bjs.1800840203.
Liu F, Li Y, Wei Y, Li B. Preoperative biliary drainage before resection for hilar cholangiocarcinoma: whether or not? A systematic review. Dig Dis Sci. 2011;56(3):663–72. https://doi.org/10.1007/s10620-010-1338-7.
Adler DG, Haseeb A, Francis G, Kistler CA, Kaplan J, Ghumman SS, et al. Efficacy and safety of therapeutic ERCP in patients with cirrhosis: a large multicenter study. Gastrointest Endosc. 2016;83(2):353–9. https://doi.org/10.1016/j.gie.2015.08.022.
Li DM, Zhao J, Zhao Q, Qin H, Wang B, Li RX, et al. Safety and efficacy of endoscopic retrograde cholangiopancreatography for common bile duct stones in liver cirrhotic patients. J Huazhong Univ Sci Technolog Med Sci. 2014;34(4):612–5. https://doi.org/10.1007/s11596-014-1325-x.
Navaneethan U, Njei B, Zhu X, Kommaraju K, Parsi MA, Varadarajulu S. Safety of ERCP in patients with liver cirrhosis: a national database study. Endosc Int Open. 2017;5(4):E303–E14. https://doi.org/10.1055/s-0043-102492.
Eker HH, van Ramshorst GH, de Goede B, Tilanus HW, Metselaar HJ, de Man RA, et al. A prospective study on elective umbilical hernia repair in patients with liver cirrhosis and ascites. Surgery. 2011;150(3):542–6. https://doi.org/10.1016/j.surg.2011.02.026.
Carbonell AM, Wolfe LG, DeMaria EJ. Poor outcomes in cirrhosis-associated hernia repair: a nationwide cohort study of 32,033 patients. Hernia. 2005;9(4):353–7. https://doi.org/10.1007/s10029-005-0022-x.
• Schlosser KA, Kao AM, Zhang Y, Prasad T, Kasten KR, Davis BR, et al. MELD-Na score associated with postoperative complications in hernia repair in non-cirrhotic patients. Hernia. 2019;23(1):51–9. https://doi.org/10.1007/s10029-018-1849-2. This paper reviews the use of MELD-Na as a predictor of postoperative complications in hernia repair.
Cho SW, Bhayani N, Newell P, Cassera MA, Hammill CW, Wolf RF, et al. Umbilical hernia repair in patients with signs of portal hypertension: surgical outcome and predictors of mortality. Arch Surg. 2012;147(9):864–9. https://doi.org/10.1001/archsurg.2012.1663.
Azoulay D, Buabse F, Damiano I, Smail A, Ichai P, Dannaoui M, et al. Neoadjuvant transjugular intrahepatic portosystemic shunt: a solution for extrahepatic abdominal operation in cirrhotic patients with severe portal hypertension. J Am Coll Surg. 2001;193(1):46–51.
Rossle M, Ochs A, Gulberg V, Siegerstetter V, Holl J, Deibert P, et al. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med. 2000;342(23):1701–7. https://doi.org/10.1056/NEJM200006083422303.
Sanyal AJ, Genning C, Reddy KR, Wong F, Kowdley KV, Benner K, et al. The North American study for the treatment of refractory ascites. Gastroenterology. 2003;124(3):634–41. https://doi.org/10.1053/gast.2003.50088.
Kim JJ, Dasika NL, Yu E, Fontana RJ. Cirrhotic patients with a transjugular intrahepatic portosystemic shunt undergoing major extrahepatic surgery. J Clin Gastroenterol. 2009;43(6):574–9. https://doi.org/10.1097/MCG.0b013e31818738ef.
• Tabchouri N, Barbier L, Menahem B, Perarnau JM, Muscari F, Fares N, et al. Original study: transjugular intrahepatic portosystemic shunt as a bridge to abdominal surgery in cirrhotic patients. J Gastrointest Surg. 2019. https://doi.org/10.1007/s11605-018-4053-x. This recent paper discusses the controversial use of TIPS prior to abdominal surgeries in cirrhotic patients.
Parvinian A, Bui JT, Knuttinen MG, Minocha J, Gaba RC. Transjugular intrahepatic portosystemic shunt for the treatment of medically refractory ascites. Diagn Interv Radiol. 2014;20(1):58–64. https://doi.org/10.5152/dir.2013.13131.
•• Northup PG, Friedman LS, Kamath PS. AGA clinical practice update on surgical risk assessment and perioperative management in cirrhosis: expert review. Clin Gastroenterol Hepatol. 2019;17(4):595–606. https://doi.org/10.1016/j.cgh.2018.09.043. These guidelines provide an up-to-date overview of the current standard of practice in management of cirrhotic patients.
Oh HK, Kim H, Ryoo S, Choe EK, Park KJ. Inguinal hernia repair in patients with cirrhosis is not associated with increased risk of complications and recurrence. World J Surg. 2011;35(6):1229–33; discussion 34. https://doi.org/10.1007/s00268-011-1007-9.
Serfaty L, Aumaitre H, Chazouilleres O, Bonnand AM, Rosmorduc O, Poupon RE, et al. Determinants of outcome of compensated hepatitis C virus-related cirrhosis. Hepatology. 1998;27(5):1435–40. https://doi.org/10.1002/hep.510270535.
Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112(2):463–72. https://doi.org/10.1053/gast.1997.v112.pm9024300.
• El-Serag HB. Hepatocellular carcinoma: recent trends in the United States. Gastroenterology. 2004;127(5 Suppl 1):S27–34. This paper reviews the incidence and epidemiology of hepatocellular carcinoma in the United States.
Cucchetti A, Ercolani G, Vivarelli M, Cescon M, Ravaioli M, La Barba G, et al. Impact of model for end-stage liver disease (MELD) score on prognosis after hepatectomy for hepatocellular carcinoma on cirrhosis. Liver Transpl. 2006;12(6):966–71. https://doi.org/10.1002/lt.20761.
Procopet B, Berzigotti A. Diagnosis of cirrhosis and portal hypertension: imaging, non-invasive markers of fibrosis and liver biopsy. Gastroenterol Rep (Oxf). 2017;5(2):79–89. https://doi.org/10.1093/gastro/gox012.
Meyer J, Balaphas A, Combescure C, Morel P, Gonelle-Gispert C, Buhler L. Systematic review and meta-analysis of thrombocytopenia as a predictor of post-hepatectomy liver failure. HPB (Oxford). 2019. https://doi.org/10.1016/j.hpb.2019.01.016.
Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg. 2009;250(5):825–30. https://doi.org/10.1097/SLA.0b013e3181b3b2d8.
Kim T, Kim BW, Wang HJ, Lee HY, Won JH, Kim J, et al. Quantitative assessment of the portal pressure for the liver surgery using serological tests. Ann Surg. 2016;264(2):330–8. https://doi.org/10.1097/SLA.0000000000001460.
Truty MJ, Vauthey JN. Uses and limitations of portal vein embolization for improving perioperative outcomes in hepatocellular carcinoma. Semin Oncol. 2010;37(2):102–9. https://doi.org/10.1053/j.seminoncol.2010.03.013.
Aldrighetti L, Guzzetti E, Pulitano C, Cipriani F, Catena M, Paganelli M, et al. Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol. 2010;102(1):82–6. https://doi.org/10.1002/jso.21541.
Memeo R, de'Angelis N, Compagnon P, Salloum C, Cherqui D, Laurent A, et al. Laparoscopic vs. open liver resection for hepatocellular carcinoma of cirrhotic liver: a case-control study. World J Surg. 2014;38(11):2919–26. https://doi.org/10.1007/s00268-014-2659-z.
Martin RC, Scoggins CR, McMasters KM. Laparoscopic hepatic lobectomy: advantages of a minimally invasive approach. J Am Coll Surg. 2010;210(5):627–34, 34-6. https://doi.org/10.1016/j.jamcollsurg.2009.12.022.
Vega EA, Kutlu OC, Joechle K, De La Cruz N, Ko D, Conrad C. Preoperative prognosticators of safe laparoscopic hepatocellular carcinoma resection in advanced cirrhosis: a propensity score matching population-based analysis of 1799 Western patients. J Gastrointest Surg. 2019;23:1157–65. https://doi.org/10.1007/s11605-019-04139-7.
Nguyen GC, Correia AJ, Thuluvath PJ. The impact of cirrhosis and portal hypertension on mortality following colorectal surgery: a nationwide, population-based study. Dis Colon Rectum. 2009;52(8):1367–74. https://doi.org/10.1007/DCR.0b013e3181a80dca.
Meunier K, Mucci S, Quentin V, Azoulay R, Arnaud JP, Hamy A. Colorectal surgery in cirrhotic patients: assessment of operative morbidity and mortality. Dis Colon Rectum. 2008;51(8):1225–31. https://doi.org/10.1007/s10350-008-9336-y.
Paolino J, Steinhagen RM. Colorectal surgery in cirrhotic patients. ScientificWorldJournal. 2014;2014:239293:1–5. https://doi.org/10.1155/2014/239293.
Lian L, Menon KV, Shen B, Remzi F, Kiran RP. Inflammatory bowel disease complicated by primary sclerosing cholangitis and cirrhosis: is restorative proctocolectomy safe? Dis Colon Rectum. 2012;55(1):79–84. https://doi.org/10.1097/DCR.0b013e3182315745.
Coakley KM, Sarasani S, Prasad T, Steele SR, Paquette I, Heniford BT, et al. MELD-Na score as a predictor of anastomotic leak in elective colorectal surgery. J Surg Res. 2018;232:43–8. https://doi.org/10.1016/j.jss.2018.04.012.
Brolin RE, Bradley LJ, Taliwal RV. Unsuspected cirrhosis discovered during elective obesity operations. Arch Surg. 1998;133(1):84–8. https://doi.org/10.1001/archsurg.133.1.84.
Nair S, Verma S, Thuluvath PJ. Obesity and its effect on survival in patients undergoing orthotopic liver transplantation in the United States. Hepatology. 2002;35(1):105–9. https://doi.org/10.1053/jhep.2002.30318.
Wu R, Ortiz J, Dallal R. Is bariatric surgery safe in cirrhotics? Hepat Mon. 2013;13(2):e8536. https://doi.org/10.5812/hepatmon.8536.
Bonner K, Heimbach JK. Obesity management in the liver transplant recipient: the role of bariatric surgery. Curr Opin Organ Transplant. 2018;23(2):244–9. https://doi.org/10.1097/MOT.0000000000000513.
de Goede B, Klitsie PJ, Lange JF, Metselaar HJ, Kazemier G. Morbidity and mortality related to non-hepatic surgery in patients with liver cirrhosis: a systematic review. Best Pract Res Clin Gastroenterol. 2012;26(1):47–59. https://doi.org/10.1016/j.bpg.2012.01.010.
Poulsen TL, Thulstrup AM, Sorensen HT, Vilstrup H. Appendicectomy and perioperative mortality in patients with liver cirrhosis. Br J Surg. 2000;87(12):1664–5. https://doi.org/10.1046/j.1365-2168.2000.01599.x.
Tsugawa K, Koyanagi N, Hashizume M, Tomikawa M, Ayukawa K, Akahoshi K, et al. A comparison of an open and laparoscopic appendectomy for patients with liver cirrhosis. Surg Laparosc Endosc Percutan Tech. 2001;11(3):189–94. https://doi.org/10.1097/00129689-200106000-00008.
Warnick P, Mai I, Klein F, Andreou A, Bahra M, Neuhaus P, et al. Safety of pancreatic surgery in patients with simultaneous liver cirrhosis: a single center experience. Pancreatology. 2011;11(1):24–9. https://doi.org/10.1159/000323961.
Nielsen SS, Thulstrup AM, Lund L, Vilstrup H, Sorensen HT. Postoperative mortality in patients with liver cirrhosis undergoing transurethral resection of the prostate: a Danish nationwide cohort study. BJU Int. 2001;87(3):183–6. https://doi.org/10.1046/j.1464-410x.2001.02048.x.
Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–9. https://doi.org/10.1056/NEJMsa0810119.
Morrow R. Perioperative quality and improvement. Anesthesiol Clin. 2012;30(3):555–63. https://doi.org/10.1016/j.anclin.2012.07.011.
Bohmer AB, Wappler F, Tinschmann T, Kindermann P, Rixen D, Bellendir M, et al. The implementation of a perioperative checklist increases patients’ perioperative safety and staff satisfaction. Acta Anaesthesiol Scand. 2012;56(3):332–8. https://doi.org/10.1111/j.1399-6576.2011.02590.x.
Ojeda A, Moreno LA. Pain management in patients with liver cirrhosis. Gastroenterol Hepatol. 2014;37(1):35–45. https://doi.org/10.1016/j.gastrohep.2013.05.007.
Dwyer JP, Jayasekera C, Nicoll A. Analgesia for the cirrhotic patient: a literature review and recommendations. J Gastroenterol Hepatol. 2014;29(7):1356–60. https://doi.org/10.1111/jgh.12560.
Hong YM, Yoon KT, Heo J, Woo HY, Lim W, An DS, et al. The prescription pattern of acetaminophen and non-steroidal anti-inflammatory drugs in patients with liver cirrhosis. J Korean Med Sci. 2016;31(10):1604–10. https://doi.org/10.3346/jkms.2016.31.10.1604.
Crosti PF, Giovannelli CA, Bardi U, Vigo PL. Hepatic blood-flow in cirrhosis. Lancet. 1971;2(7719):322.
Meierhenrich R, Wagner F, Schutz W, Rockemann M, Steffen P, Senftleben U, et al. The effects of thoracic epidural anesthesia on hepatic blood flow in patients under general anesthesia. Anesth Analg. 2009;108(4):1331–7. https://doi.org/10.1213/ane.0b013e3181966e6f.
Bunchorntavakul C, Supanun R, Atsawarungruangkit A. Nutritional status and its impact on clinical outcomes for patients admitted to hospital with cirrhosis. J Med Assoc Thail. 2016;99(Suppl 2):S47–55.
Maharshi S, Sharma BC, Srivastava S. Malnutrition in cirrhosis increases morbidity and mortality. J Gastroenterol Hepatol. 2015;30(10):1507–13. https://doi.org/10.1111/jgh.12999.
Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, Boffo G, et al. Nutrition and survival in patients with liver cirrhosis. Nutrition. 2001;17(6):445–50. https://doi.org/10.1016/S0899-9007(01)00521-4.
• Plauth M, Bernal W, Dasarathy S, Merli M, Plank LD, Schutz T, et al. ESPEN guideline on clinical nutrition in liver disease. Clin Nutr. 2019;38:485–521. https://doi.org/10.1016/j.clnu.2018.12.022. This paper includes the most recent ESPEN guides of the nutritional management of patients with liver disease.
Tonnesen H, Rosenberg J, Nielsen HJ, Rasmussen V, Hauge C, Pedersen IK, et al. Effect of preoperative abstinence on poor postoperative outcome in alcohol misusers: randomised controlled trial. BMJ. 1999;318(7194):1311–6. https://doi.org/10.1136/bmj.318.7194.1311.
Tonnesen H. Alcohol abuse and postoperative morbidity. Dan Med Bull. 2003;50(2):139–60.
Vinet E, Perreault P, Bouchard L, Bernard D, Wassef R, Richard C, et al. Transjugular intrahepatic portosystemic shunt before abdominal surgery in cirrhotic patients: a retrospective, comparative study. Can J Gastroenterol. 2006;20(6):401–4. https://doi.org/10.1155/2006/245082.
Saad WE, Saad NE, Davies MG, Bozorgdadeh A, Orloff MS, Patel NC, et al. Elective transjugular intrahepatic portosystemic shunt creation for portal decompression in the immediate pretransplantation period in adult living related liver transplant recipient candidates: preliminary results. J Vasc Interv Radiol. 2006;17(6):995–1002. https://doi.org/10.1097/01.RVI.0000223683.87894.a4.
Schenk P, Fuhrmann V, Madl C, Funk G, Lehr S, Kandel O, et al. Hepatopulmonary syndrome: prevalence and predictive value of various cut offs for arterial oxygenation and their clinical consequences. Gut. 2002;51(6):853–9. https://doi.org/10.1136/gut.51.6.853.
Saner FH, Kirchner C. Monitoring and treatment of coagulation disorders in end-stage liver disease. Visc Med. 2016;32(4):241–8. https://doi.org/10.1159/000446304.
Rai R, Nagral S, Nagral A. Surgery in a patient with liver disease. J Clin Exp Hepatol. 2012;2(3):238–46. https://doi.org/10.1016/j.jceh.2012.05.003.
Villanueva C, Colomo A, Bosch A, Concepcion M, Hernandez-Gea V, Aracil C, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368(1):11–21. https://doi.org/10.1056/NEJMoa1211801.
Salooja N, Perry DJ. Thrombelastography. Blood Coagul Fibrinolysis. 2001;12(5):327–37. https://doi.org/10.1097/00001721-200107000-00001.
• De Pietri L, Bianchini M, Montalti R, De Maria N, Di Maira T, Begliomini B, et al. Thrombelastography-guided blood product use before invasive procedures in cirrhosis with severe coagulopathy: a randomized, controlled trial. Hepatology. 2016;63(2):566–73. https://doi.org/10.1002/hep.28148. This paper evaluates the use of TEM to guide blood product use in cirrhotics , minimizing the unnecessary use of products and thus decreasing the risk of complications.
• Michelson AD, Smolensky Koganov E, Forde EE, Carmichael SL, Frelinger AL 3rd. Avatrombopag increases platelet count but not platelet activation in patients with thrombocytopenia resulting from liver disease. J Thromb Haemost. 2018;16(12):2515–9. https://doi.org/10.1111/jth.14295. This paper presents the newest FDA-approved treatment for thrombocytopenia in liver disease that could revolutionize the management of this patient population.
Tsiompanidis E, Siakavellas SI, Tentolouris A, Eleftheriadou I, Chorepsima S, Manolakis A, et al. Liver cirrhosis-effect on QT interval and cardiac autonomic nervous system activity. World J Gastrointest Pathophysiol. 2018;9(1):28–36. https://doi.org/10.4291/wjgp.v9.i1.28.
Singal AK, Salameh H, Kamath PS. Prevalence and in-hospital mortality trends of infections among patients with cirrhosis: a nationwide study of hospitalised patients in the United States. Aliment Pharmacol Ther. 2014;40(1):105–12. https://doi.org/10.1111/apt.12797.
Hagstrom H, Nasr P, Ekstedt M, Hammar U, Stal P, Askling J, et al. Cardiovascular risk factors in non-alcoholic fatty liver disease. Liver Int. 2019;39(1):197–204. https://doi.org/10.1111/liv.13973.
Fan ST, Lo CM, Lai EC, Chu KM, Liu CL, Wong J. Perioperative nutritional support in patients undergoing hepatectomy for hepatocellular carcinoma. N Engl J Med. 1994;331(23):1547–52. https://doi.org/10.1056/NEJM199412083312303.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Liver
Rights and permissions
About this article
Cite this article
Diaz, K.E., Schiano, T.D. Evaluation and Management of Cirrhotic Patients Undergoing Elective Surgery. Curr Gastroenterol Rep 21, 32 (2019). https://doi.org/10.1007/s11894-019-0700-y
Published:
DOI: https://doi.org/10.1007/s11894-019-0700-y