Abstract
Purpose of Review
The aim of this review is to identify the implementation approaches, strategies, and outcomes for continuous glucose monitoring (CGM) in the intensive care unit (ICU). Medline and Web of Science databases were searched to report relevant literature published between September 12, 2016 and September 12, 2021. Implementation outcomes and strategies, defined by the Expert Recommendations for Implementing Change (ERIC) project, were extracted.
Recent Findings
Of the 324 titles reviewed, 16 articles were included in the review. While no studies were identified as implementation research, 14 of 16 identified implementation strategies that aligned with ERIC definitions. Included studies described a multi-disciplinary approach. Clinical outcomes included Mean Absolute Relative Difference (MARD), ranging from 7.5 to 15.3%, and 33–71% reduction in frequency of point-of-care (POC) blood glucose monitoring (BGM) using hybrid protocols.
Summary
This scoping review provides valuable insight into the process of CGM implementation in the ICU. Continued research should include implementation outcomes to inform widespread utilization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Continuous glucose monitoring (GCM) has been a mainstay of diabetes care with consistently positive outcomes across diabetes populations managed in ambulatory and home settings. While CGM has been studied in the inpatient setting, it is not approved by the Food and Drug Administration (FDA) for use within the hospital setting. The potential benefit of these systems within the hospital setting, and more specifically in the critical care environment has long been recognized. [1, 2•] Much of the previous inpatient CGM research has been focused primarily on device accuracy rather than people with diabetes (PWD) or clinical use outcomes.
During the COVID-19 pandemic, CGM emerged as an important and innovative approach to manage hyperglycemia while reducing healthcare worker exposure to the virus. In April 2020, the FDA provided emergency use authorization for CGM to be used in hospitals during the pandemic. [3] Since then, there have been increasing reports in the research literature of successful use of CGM for critically ill patients, with demonstrated safety and efficacy primarily among COVID-19 patients. [4•, 5•, 6•, 7,8,9,10] The rapid clinical deployment of CGM in the hospital during the COVID-19 pandemic provided a unique opportunity to study integration of these systems into practice. While studies demonstrate a reduction in point of care (POC) glucose monitoring, reasonable accuracy, and consistent safety, few studies specifically reported on the process of implementing CGM into current workflow. Use of an implementation science approach allows for investigation into factors that facilitate or inhibit routine uptake of research findings into practice settings. Previous reviews on the use of CGM in the hospital and critical care environment have focused primarily on clinical outcomes. [1, 11] While an understanding of clinical outcomes is essential for future inpatient CGM use, information on implementation specific strategies and outcomes are equally important to advance potential use of CGM for hospitalized patients outside of the urgency of a pandemic.
The field of implementation science provides a taxonomy of implementation strategies and outcomes to continue to advance knowledge about effective approaches for increasing uptake of new treatments or services in practice settings. [12, 13] Implementation strategies are the specific actions taken to increase routine use of a new practice. These strategies have been categorized and defined by the Expert Recommendations for Implementing Change (ERIC) project and include 73 distinct activities that have been extensively studied for their effectiveness of uptake of new practices among end users. [12] Similarly, implementation outcomes reflect measures that evaluate frequency and degree of uptake and routine use of new treatments or services within practice settings. These outcome measures include acceptability, adoption, appropriateness, cost, feasibility, fidelity, penetration, and sustainability [13].
Information on implementation factors must accompany current data on clinical effectiveness of CGM in critical care units. This information is particularly relevant, given that CGM devices currently available are designed for personal use in the ambulatory setting, and not necessarily for inpatient hospital use. Potential considerations when seeking to evaluate use of CGM for hospitalized patients include training of personnel, device set-up, data transmission and sharing, documentation of glucose measures, clinical protocols, and frequency and feasibility of routine use. While some research has evaluated CGM use for non-critically ill patients, little work has evaluated factors impacting routine use in critical care settings due to rapidly changing clinical factors that can cause unpredictable glucose fluctuations and potentially affect the accuracy and safety of interstitial glucose measurements. Additional concerns exist about interfering substances, medications, and devices that could impede CGM accuracy in the inpatient setting. [5•] Moreover, ICU patients are less likely to be able to communicate symptoms of hypoglycemia. In light of the preliminary research that has established clinical efficacy and effectiveness of CGM in critical care settings, additional data are needed to inform actual approaches to routine implementation. Therefore, the purpose of this scoping review was to identify the implementation approaches, strategies, and outcomes for CGM use in critical care hospital settings.
Methods
A scoping review was conducted to understand the implementation factors associated with CGM use in the critical care environment. A protocol to guide this scoping review was created a priori and components aligned with the Preferred Reporting and Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR).
Search Strategy
A structured librarian-assisted literature search of peer reviewed articles was performed using electronic databases including Medline and Web of Science. Reference lists of eligible articles and related systematic reviews were reviewed to identify additional articles. The search strategy was based on the following keywords: (Continuous Glucose Monitoring OR CGM) AND (ICU OR Intensive Care Unit OR Critical Care). Filters were used to limit results to reports of primary studies, in the English language, published between September 12, 2016 and September 12, 2021. Covidence systematic review software (www.covidence.org) was used for all stages of the review.
Inclusion and Exclusion Criteria
Articles were included if they were published between 9/12/2016 and 9/12/2021, were available in English language, and reported findings from original research, implementation science, and/or quality improvement designs published in a peer reviewed journal. Articles also had to report implementation approaches, strategies, and/or outcomes for CGM in pediatric and/or adult critical care settings. Publications were excluded if they were commentaries or editorials, literature reviews, published abstracts/conference proceedings, and if the setting for CGM use was not critical care.
Data Extraction
Two reviewers (ERF, MM) independently reviewed titles and abstracts of search results to determine initial eligibility based on inclusion and exclusion criteria. The same two reviewers then reviewed the full text articles to verify final inclusion in the review. At each stage of the review process, any discrepancies were resolved through consensus with a third reviewer (KMD).
Extracted data elements were established a-priori in the review protocol. Two reviewers (ERF, MM) independently extracted data from included articles using standardized extraction forms. Extracted data elements included the following elements: title/author, year of publication, aims, country, setting (type of unit), project design, theory/model/framework guiding the project, implementation strategies as outlined by the ERIC group, [12] and implementation outcomes as outlined by Proctor. [13] Specific components of the implementation process were also extracted, which included type of training/education for CGM use, team members involved in use/implementation, protocol identified/used, and CGM data transmission strategy. Lastly, clinical outcomes were extracted and included mean absolute relative difference (MARD) ([absolute value of the reference glucose – CGM glucose]/reference glucose), time in range (70-180 mg/dl), and Clark Error Grid of glucose values. MARD is a commonly used measurement that is easy to calculate and interpret which matches CGM values to a comparison glucose measurement for all patients in a sample.
Results
The initial search retrieved 443 manuscripts with 324 titles and abstracts reviewed after duplicates were removed (Fig. 1). Of these, 290 were excluded for not meeting initial inclusion criteria resulting in 34 articles that underwent full text review. Articles were eliminated for the follow reasons: no approaches, strategies, and/or outcomes of CGM implementation or sustainability efforts were reported (n = 12); because the research in fact did not occur in the critical care setting (n = 2); studies were not original research, implementation science, and/or QI designs (n = 2); the study used blinded CGM (n = 1); and because no outcomes were reported (n = 1). Sixteen articles were identified to meet inclusion criteria and were included in the review.
Characteristics of Included Studies
All 16 articles included in the review were original research studies. Included studies represented a wide variety of methodological approaches including: randomized controlled trial (n = 4) [14, 15, 16, 17], retrospective cohort studies (n = 7) [4•, 5•, 6•, 8, 10, 18, 19•, 20], prospective cohort studies (n = 3) [9, 21, 22], quasi-experimental (n = 1) [23], and qualitative (n = 1) designs [24]. Eight studies included implementation and clinical data collected during the COVID-19 pandemic [4•, 5•, 6•, 7, 8, 9, 10, 24]. Studies were from 2016 to 2021 and incorporated a total of 1,290 critical care patients. Most studies were conducted in medical intensive care units (MICU) (n = 11) [4•, 5•, 8, 9, 10, 14, 19•, 21, 24, 25], with other studies conducted in mixed intensive care unit (ICU) environments (n = 2) [18, 26], in the pediatric ICU (PICU) [27], and in a cardiac ICU (n = 1) [28]. Half of the studies were conducted in the USA (n = 8) [4•, 5•, 6•, 7, 8, 10, 15, 20, 24], while others were conducted in Europe (n = 5) [14, 17, 21, 22, 29], China (n = 1) [16], Korea (n = 1)[28], and Columbia (n = 1). [9] A number of different types of CGM devices were used (Table 1), with the Dexcom G6 CGM system used most frequently. [4•, 5•, 6•, 7, 8, 10, 20] Several studies featured CGM systems that are not commercially available [14,15,16,17,18, 21, 22, 28].
Implementation Approaches and Strategies
There was wide heterogeneity in implementation approaches across the included studies (Table 2). The majority of studies (n = 10) reported at least intermittent non-adjunctive CGM use, meaning a confirmatory POC measure was not always required. [4•, 5•, 8, 10, 18, 19•, 24, 25, 26, 28] In 9 studies, the CGM value could be used to titrate insulin. [4•, 5•, 7, 9, 10, 17, 20, 24, 25, 29] Interestingly non-adjunctive use and use for insulin titration were not mutually exclusive. For example, Song 2017 reported that the CGM could be used non-adjunctively but when CGM glucose values met a threshold for insulin adjustment or dosing, then POC glucose was obtained for insulin administration. [28] Not surprisingly, the majority of articles reporting non-adjunctive use and CGM use for insulin dosing were observational studies conducted during the COVID-19 pandemic [4•, 5•, 8, 9, 10, 19•, 20, 24].
In studies describing CGM device set up and sensor insertion most indicated members of the research team performed these tasks. [14, 16,17,18, 21, 28] However, during the COVID-19 pandemic, device set-up was performed by members of the endocrinology/diabetes team [4•, 10, 24] while sensor insertion and pairing of the CGM was completed by either the endocrinology/diabetes team [6•, 10, 19•] or by members of the nursing team. [4•, 5•, 8, 9, 20, 24] Several studies described CGM glucose monitoring as performed by nurses, [5•, 20, 24]while in others, the endocrinology team[8] or research team[14] primarily performed monitoring activities. Individuals involved in CGM activities and team composition varied across included studies. Nurses were mentioned most often [5 •, 6 •, 8, 9, 10, 15, 16, 17, 18, 19•, 21, 22, 24] with only 2 studies not mentioning their involvement. [14, 28] Not surprisingly, the pre-COVID era studies all mentioned the role of research staff members, [14, 15, 16, 17, 18, 21, 28] whereas 7 of the 8-pandemic era retrospective studies reported endocrinology/diabetes (DM) team involvement [5•, 6•, 8, 9, 10, 19•, 24].
How glucose was visualized or transmitted was described in 10 studies. [5•, 6•, 8, 10, 16, 18, 19•, 24, 28, 30] Glucose was most often transmitted via Bluetooth to receivers or phones, [5•, 6•, 8, 10, 18, 19•, 20, 24] often kept outside the patient room. [5•, 6•, 8, 10, 19•, 20, 24] Davis et. al., created a glucose telemetry system in which CGM glucose data was transmitted to the Dexcom G6 app on phones kept just outside the person’s room. The Dexcom Follow app was then used to transmit glucose to the nurses’ station where values could be visualized and alarms could be heard in real-time. [5•] Several studies mentioned the use of download visualization software (i.e., Dexcom Clarity, LibreView, CoPilot Health Management System) [5 •, 6•, 9, 18, 24] with a handful specifically mentioning use by the endocrinology/DM teams [5•, 20, 24].
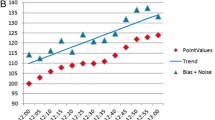
While none of the studies were identified specifically as implementation research, 14 of the 16 identified inpatient implementation strategies that aligned with ERIC definitions (Table 2). Only two studies did not report on any implementation strategies. [14, 28] Across the remaining studies, the frequency of specific implementation strategies used are displayed in Fig. 2. Seventeen different ERIC strategies were described and included in descending order: facilitate relay of clinical data, [4•, 5•, 6•, 8, 9, 10, 16, 17, 19•, 24, 27] educational meetings, [4•, 18, 22, 24] change in physical structure, [6•, 8, 10, 24, 25] distribute materials, [8, 9, 25] identify facilitators and barriers, [21, 24] develop educational materials, [8, 24, 25] assess for readiness,[21, 24] provide clinical supervision, [8, 24] centralize technical assistance, [15, 24] create new clinical teams, [24] conduct ongoing training, [4•] identify and prepare champions, [24] change record systems, [5•] data experts, [5•] data warehousing techniques, [5•] build a coalition, [24] and bedside reference materials [8].
Clinical and Implementation Outcomes
Several different clinical and implementation outcomes were reported across the various studies, which were not consistent or mutually exclusive. (Table 3). Most studies reported both clinical and implementation outcomes (10/16, 63%), [4•, 5•, 6•, 8, 15, 16, 20, 21, 22, 26, 28] while one study reported only implementation outcomes (1/16, 6%), [24] and some reported only clinical outcomes (5/16, 31%). [7, 9, 10, 14, 18] Clinical outcomes are synthesized in Fig. 2. MARD was reported in 7 studies and ranged from 7.5 to 15.3%. [4•, 8, 10, 19•, 21, 22, 29] MARD source varied between studies including arterial,[29] a combination of capillary, venous, or arterial[4•, 8, 10, 21, 22] or not specified. [19•] Seven studies reported Clark Error Grid analysis with results showing > 75% of values in zone A (within 20% of reference glucose value). [5•, 6•, 10, 19•, 21, 22, 28] Time in range (70–180 mg/dl), was reported in 5 studies and fell within a wide range of 46.1% and 75.7%. [4•, 5•, 17, 19•, 30] In one study, time in range was reported as 144-180 mg/dl to better align with American Diabetes Association in hospital recommendations for critical care [31] and found significantly higher time between 144 and 180 mg/dl for participants on CGM vs. standard POC blood glucose monitoring (BGM) ((51.5% vs 29.0%). [16] One study reported similar accuracy (60.1% vs. 57%, in zone A of the Clark Error Grid, respectively) between CGM placement sites (thigh vs. abdomen). [28] Frequency of POC BGM was reported most often in COVID-19 related studies that used a hybrid protocol combining reduced frequency POC BGM and intermittent non-adjunctive CGM. Reduction in POC was dependent on hybrid protocol design, for which studies reported a 33–71% reduction in POCBGM [4•, 5•, 6•, 8, 10, 19•, 20].
Implementation outcomes included various measures of components outlined by Proctor in the field of implementation science (acceptability, adoption, appropriateness, cost, feasibility, fidelity, penetration, sustainability). [13] Across the studies included in this review, feasibility was reported most often (6), along with fidelity (2), acceptability (2), and appropriateness (1). Feasibility was defined as the ability to successfully implement CGM (e.g., training program development, sustained use, successful data capture), while fidelity was the degree to which CGM was implemented as prescribed (e.g., protocol adherence, consistent application) [13].
Acceptability was defined as the perception among end users that CGM was satisfactory for routine use, and appropriateness referred to the perceived fit or relevance of CGM for the population and setting among end users. [13] Using these established definitions, two studies reported non-adherence to the protocol in which nurses continued to check POC glucose after CGM had been validated for intermittent non-adjunctive use. [4•, 8] Interestingly, both studies reported that nursing adherence improved over time. [4•, 8] Only three studies examined nursing acceptance of CGM systems within the ICU with two studies conducted during the COVID-19 pandemic showing positive sentiment. [6•, 21, 24] In a qualitative focus group, nurses reported perceived accuracy was high and there was a strong sense of nursing ownership over the technology. [24] Interestingly, while nurses felt time spent obtaining glucose information was reduced, they actually reported time monitoring glucose increased because CGM values were continuously available. [24] Chow et. al. reported survey data showing 63% of nurses felt CGM use improved clinical care and 49% indicated CGM reduced use of personal protective equipment (PPE). [6•] In an earlier study by Wollersheim et. al., 79.1% of nurses rated CGM as non-beneficial. [21] It is important to note that the study used older technology that required frequent calibration and additionally, the study reported a high rate of premature removal of sensors (21 out of 31) with 71% of early removals attributed to sensor related issues [21].
Discussion
This scoping review is the first to synthesize existing literature on factors influencing implementation of CGM in the critical care setting. Examination of factors influencing use of the systems within the critical care infrastructure will help facilitate safe and effective use of CGM. This information is critically important during a pandemic as health systems work to rapidly deploy CGM, but even more importantly, this information will establish a blueprint for successful deployment of CGM into routine critical care settings.
The inclusion of both clinical and implementation outcomes and strategies within research protocols is essential for the evaluation of CGM in the critical care environment. While an examination of clinical outcomes such as sensor accuracy and glycemic management are of undoubted importance, if we are to move toward routine use of CGM in the hospital, an examination of implementation factors such as fidelity to treatment guidelines and feasibility are also critical. We can illustrate this by examining current standard of care POC glucose monitoring in the inpatient setting. The accuracy of inpatient POC meters, particularly those FDA approved for critical care use, is excellent with 97.2% of the Novo StatStrip’s values lying in A zone and 2.8% in the B zone of the Clark Error Grid. [32] However, intensive inpatient POC blood glucose monitoring is a time-consuming task, often resulting in insufficient frequency and inadequate timing of BGMing [32].
The communication of implementation approaches and strategies are essential as health systems begin to consider what supports (e.g., training, team) are needed for safe and effective future use of these systems within the hospital. Specifically, clinical outcomes should be evaluated and reported in the context of implementation strategies and approaches. For instance, two observational COVID-19 era studies reported vastly differed in time in range (46.1% vs. 72.5%, respectively) as their clinical outcomes. [7, 30] These outcomes can be heavily influenced by the protocol via which CGM was deployed, but also by team composition, training, and ongoing management and monitoring of values. Reductions in POC BGMare also difficult to evaluate without contextual factors, such as full institutional protocol description, to understand whether this was an expected reduction in frequency of POCBGM [7].
Several studies included in this review did report on approaches to implementation, which included team composition, delineation of roles, and protocols. Overall, team composition and delineation of CGM tasks and responsibilities varied significantly across studies. Previous publications have discussed the importance of hospitalendocrinology and diabetes teams in the future implementation of hospital CGM. [2•, 33] All but one pandemic era study mentioned endocrinology and diabetes team involvement which is an important consideration for health systems and hospitals that do not have dedicated inpatient diabetes teams.
Prior to this review, team member roles and responsibilities had not been synthesized. Given that glucose monitoring with traditional POC BGM is currently performed by nurses or by individuals under nursing supervision (e.g., nursing assistants), an understanding of nursing role and responsibilities in the implementation of CGM in the critical care environment is essential. All but two studies mentioned at least some aspect of the nursing role in CGM use. [4•, 5•, 6•, 8, 9, 10, 15, 17, 19•, 20, 21, 22, 24, 25, 29] These pandemic-era studies provided valuable data on how nurses use CGM in clinical practice and nursing scope surrounding the technology. In addition to nursing team members, pandemic-era approaches also involved other individuals within a multi-disciplinary team and roles among members. Teams included members of the diabetes or endocrinology service, [4•, 5•, 6•, 8, 10, 19•, 20, 24] critical care medicine, [10, 24] and pharmacy. [5•, 20, 24] While these studies reported on team composition, less information was supplied on actual role delineation among team members. For example, few studies explored or reported on the fact that the ICU nurse needs to use CGM data in real time to dose insulin and prevent and treat hyperglycemia and hypoglycemia, whereas prescribers on care teams may be more likely to use CGM data retrospectively to make treatment decisions and change insulin orders. Future research is needed to better explore this concept of role delineation in CGM use within critical care settings.
In addition to team composition and roles for CGM use, several studies reported on protocols which inform the overall approach to scale this type of monitoring for use in critical care settings. Hybrid protocols were widely described in COVID-19 pandemic-era studies and offered a means of reducing the frequency of POC measures while still requiring intermittent POC BGMfor confirmation of CGM accuracy or when glucose exceeded certain thresholds or other clinical criteria were met. [4•, 5•, 6•, 8, 10, 19•, 20] All 6 studies using hybrid protocols required more stringent validation measures on sensor insertion [4•, 5•, 6•, 8, 10, 19•, 20] and 3 studies did not use the CGM clinically for the first 24 h. [6•, 8, 10] Previous outpatient CGM research has shown somewhat lower accuracy during the first 12–24 h of CGM use, [34]supporting the rationale for increased POC BGM and validation on initial CGM insertion. Of the 6 studies describing hybrid protocol use, 4 used 20% as a threshold for nonadjunctive use. [4•, 5•, 6•, 7, 20] with one study requiring the difference in values to be < 35 mg/dl [10] Another study allowed intermittent non-adjunctive use if the CGM glucose level fell between 100 and 200 mg/dl. [8] Ongoing POC BGM and validation was most often performed every 6 h, [4•, 5•, 20] while two studies required only daily POC, [10, 19•], and one study fluctuated between Q2 and Q4 hour POC glucose monitoring [8]. The data from this review shows safe and effective intermittent non-adjunctive use of CGM within the constraints of a hybrid protocol. Specifically, investigations into CGM impact on workflow among nurses is of particular interest, given preliminary work demonstrating reduced care burden, coupled with current estimates of an unprecedented nursing shortage [35].
Another consideration when evaluating implementation approaches is the type of CGM sensor. Many of the studies included in this review feature older technologies which are either no longer commercially available, [15, 18, 28] or were previously under development for the inpatient environment but not commercially available. [14, 16, 17, 21, 22] The effect of technology specification on clinical outcomes such as accuracy is well understood and studied, however technology design has a significant impact on implementation. For instance, Wollersheim et. al., reported poor acceptance and use of CGM, which they attributed to application and performance of the CGM system. In the study, 21 out of 31 sensors were removed prematurely, data transmission was poor, and the system under investigation required every 8 h calibrations for routine use. Not surprisingly, nearly 80% of nurses found the system to be unhelpful [21].
When examining implementation strategies, several were reported consistently across the studies included in this review. All studies utilized facilitated relay of clinical data, while 6 studies included use of educational meetings, and 5 reported use of changes to clinical structures. Facilitating relay of clinical data refers to providing real-time data to clinicians about key process/outcomes using various channels of communication to promote use of the targeted innovation. [12] Clearly this component is critical for increasing routine use of CGM as clinical providers need to be able to easily access readings in real time to inform treatment interventions. Relay of this clinical data for CGM was done by a variety of measures, including use of apps and handheld devices, receivers placed just outside the person’s room for ease of visualization, and centralized dashboards. Conducting educational meetings was another implementation strategy commonly used. This strategy refers to holding meetings with different stakeholder groups to teach them about the clinical innovation. [12] Education would be a required component for implementation of any new technology; as such, it is an expected strategy to increase initial and ongoing use of CGM in critical care settings. The final common implementation strategy was change in physical structures and equipment, which is defined as evaluating and adapting structures and equipment to accommodate the targeted innovation. [12] Studies, particularly those performed on CGM use during the COVID-19 pandemic, report on changing the physical structure of critical care rooms to accommodate closed door systems with CGM receivers placed in clear view of clinical staff either right outside the room, or in adjacent areas. Other implementation strategies were reported in single studies and included creating new clinical teams, building a coalition, conducting ongoing training, use of champions, changing record systems, use of data experts, data warehousing, and creating bedside reference materials. As research continues to evaluate use of CGM in critical care settings, integrating this taxonomy of strategies is necessary to generate evidence about frequency and effectiveness of specific implementation strategies. Ultimately, this collective information about strategies can be used to inform future development of toolkits and bundles for sites seeking to integrate CGM as routine care.
The majority (11 out of 16) of the studies in this review reported on some aspect of implementation outcomes. One study used a qualitative design and only reported on implementation outcomes [24]; the remaining (10 out of 11) studies reported on both clinical and implementation outcomes. Across implementation outcomes, feasibility was reported most often. Feasibility refers to the degree that a new treatment or innovation can be successful integrated into a practice setting. [13] Common measurement indices for this outcome are lacking [36]: as such, there was wide heterogeneity in how this outcome was measured and reported across the studies in our review. Indicators of feasibility included measurement of startup time, [22] percentage of successful measurements,[28] average down time, [32] number of nurse encounters, [5•] and degree and duration of CGM insertion. [4•, 24] Fidelity to treatment protocols is an important implementation outcome, yet was only reported in two studies. [15, 25] However, both reported fidelity as the degree of adherence to CGM protocols. Similarly, acceptability, defined as the degree that stakeholders perceive the innovation to be agreeable, [13] was only reported in 2 studies, [8, 21] but both included nurse perceptions of CGM use. Future research evaluating CGM use should aim to incorporate these and other implementation outcomes using established definitions, [13] as well as recommendations for measurement and reporting [36] to continue to generate knowledge on optimal methods for uptake of routine CGM use in critical care settings.
Use of hybrid implementation research designs [37] is one approach to efficiently advance CGM use in critical care settings. Hybrid effectiveness-implementation designs incorporate a dual focus to evaluate both effectiveness of an intervention and factors associated with implementation. In traditional research approaches, implementation research is often not pursued until clinical outcomes are well established in the field, which may take several years. This approach contributes to the persistent research to practice gap, delaying systematic uptake of best practices. However, because hybrid designs combine elements of both effectiveness and implementation research, it is possible to simultaneously generate evidence on whether a therapy or treatment is effective, and what are the best mechanisms to integrate it into routine clinical practices. Use of this approach for CGM use in critical care has potential to enable more rapid adoption of CGM as a standard of care if it continues to demonstrate positive benefit for patients and clinicians. Incorporation of implementation outcomes, and particularly cost, offers additional benefit to inform return on investment and drive decisions at policy and reimbursement levels [38, 39].
This scoping review has several limitations including the fact that many of the inpatient studies used older technologies that are either no longer commercially available or were under development at the time. Given that technology specifications can greatly influence implementation and expected accuracy, findings from a study using one type of technology may not be generalized across similar technologies. Additionally, studies differed according to protocol and research method. It is possible that some studies that include implementation data were missed based on the search strategy, inclusion or exclusion criteria, or the databases searched.
Conclusion
This scoping review provides valuable consensus on implementation strategies and outcomes employed in existing studies in the critical care environment. The rapid integration of CGM into the hospital setting during the COVID-19 pandemic provided a unique opportunity to assess implementation while generating valuable clinical outcomes data. The use of CGM in the inpatient setting holds tremendous promise to improve glycemic outcomes, and reduce nursing workload and associated healthcare costs; however, the inpatient use of CGM beyond the pandemic presents unique challenges associated with staff training, use in a variety of health systems and team structures, and EHR integration, necessitating future implementation research.
Data Availability
These data were derived from the following resources available in the public domain: Medline and Web of Science.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Umpierrez GE, Klonoff DC. Diabetes Technology Update: Use of Insulin Pumps and Continuous Glucose Monitoring in the Hospital. Diabetes Care. 2018;41:1579–89.
MC Perez-Guzman T Shang JY Zhang D Jornsay DC Klonoff 2021 Continuous Glucose Monitoring in the Hospital EndocrinolMetab Seoul 36 240 55 The authors present one of the first comprehensive reviews highlighting inpatient CGMduring the COVID-19 pandemic with a summary of outcomes including accuracy data.Consideration for use of CGM by level of care (e.g., intensive care unit, surgery) and roleof multidisiplinary team are discussed.
U.S. Food & Drug. Coronavirus (COVID-19) Update FDA allows expanded use of devices to monitor patients vital signs remotely
Faulds, E. R., et al. 2021 Use of Continuous Glucose Monitor in Critically Ill COVID 19 Patients Requiring Insulin Infusion An Observational Study J Clin Endocrinol Metab 106(10):e4007–e4016. A retrospective analysis of an initial cohort (N=19) of COVID-19 patients using CGM within a hybrid point-of-care + CGM protocol. The authors report a 71% reduction in frequency of POC glucose testing compared with standard hourly POC testing for patients on IV insulin. Glycemic outcomes included TIR (70–180mg/dl), which was 72% after day one, and MARD, which was 13.9%.
Davis GM, Faulds E, Walker T, et al. 2021 Remote Continuous Glucose Monitoring With a Computerized Insulin Infusion Protocol for Critically Ill Patients in a COVID 19 Medical ICU Proof of Concept Diabetes Care 44 1055 8 The authors report on experience and outcomes from an initial cohort (N=9) using a hybrid CGM and POC glucose monitoring protocol in the ICU during the COVID-19 pandemic. Mean TIR (70–180mg/dl) was 71.4%. CGM reduced POC tests to 8.24+/-3.06, resulting in 63% reduction and 75.7% of CGM values were within 20% of POC reference values. The authors provide a detailed description of a remote patient monitoring and telemetry system configured within the ICU.
Chow KW, Kelly DJ, Rieff MC, et al. 2021 Outcomes and Healthcare Provider Perceptions of Real-Time Continuous Glucose Monitoring rtCGM in Patients With Diabetes and COVID-19 Admitted to the ICU J Diabetes Sci Technol 1932296820985263 The largest retrospective analysis of hospitalized COVID-19 patients (N=30) using CGM. There was a high concordance of CGM values with arterial reference values (within 20%) in all but 2 patients. CGM enabled a reduction in glucose from 440mg/dL to 200–300mg/dL within first 12hrs and sustained decreases to 100–200mg/dL within 7 days. Reduction in daily POC testing in 50% of patients. The publication is one of a handful to include nursing perspectives with a nursing survey showing 63% of nurses (N=66) felt that CGM improved the care their patient received.
Agarwal S, Mathew J, Davis GM, et al. Continuous Glucose Monitoring in the Intensive Care Unit During the COVID-19 Pandemic. Diabetes Care. 2021;44:847–9.
Sadhu AR, Serrano IA, Xu J, et al. Continuous Glucose Monitoring in Critically Ill Patients With COVID-19: Results of an Emergent Pilot Study. J Diabetes Sci Technol. 2020;14:1065–73.
Gómez AM, Henao DC, Muñoz OM, et al. Glycemic control metrics using flash glucose monitoring and hospital complications in patients with COVID-19. Diabetes Metab Syndr. 2021;15:499–503.
Longo RR, Elias H, Khan M, Seley JJ. 2021 Use and Accuracy of Inpatient CGM During the COVID-19 Pandemic An Observational Study of General Medicine and ICU Patients J Diabetes Sci Technol 19322968211008446
van Steen SC, Rijkenberg S, Limpens J, van der Voort PH, Hermanides J, DeVries JH. 2017 The Clinical Benefits and Accuracy of Continuous Glucose Monitoring Systems in Critically Ill Patients-A Systematic Scoping Review Sensors Basel 17
Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21.
Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38:65–76.
De Block CEM, Rogiers P, Jorens PG, Schepens T, Scuffi C, Van Gaal LF. A comparison of two insulin infusion protocols in the medical intensive care unit by continuous glucose monitoring. Ann Intensive Care. 2016;6:115.
Agus MS, Wypij D, Hirshberg EL, et al. Tight Glycemic Control in Critically Ill Children. N Engl J Med. 2017;376:729–41.
Lu M, Zuo Y, Guo J, Wen X, Kang Y. Continuous glucose monitoring system can improve the quality of glucose control and glucose variability compared with point-of-care measurement in critically ill patients: A randomized controlled trial. Medicine (Baltimore). 2018;97: e12138.
Preiser JC, Lheureux O, Thooft A, Brimioulle S, Goldstein J, Vincent JL. Near-Continuous Glucose Monitoring Makes Glycemic Control Safer in ICU Patients. Crit Care Med. 2018;46:1224–9.
Rijkenberg S, van Steen SC, DeVries JH, van der Voort PHJ. Accuracy and reliability of a subcutaneous continuous glucose monitoring device in critically ill patients. J Clin Monit Comput. 2018;32:953–6419.
Agarwal S, Mathew J, Davis GM, et al. 2021 Continuous Glucose Monitoring in the Intensive Care Unit During the COVID 19 Pandemic Diabetes Care 44 847 9 Retrospective (N=11), hybrid protocol. Frequency of POC decreased by 60% with routine CGM use. Mean number of hours of potential POC testing was 72.1hrs, which decreased to 28hrs with CGM use. Median number of days on CGM was 9.0. Mean TIR (70–180mg/dl) was 46.1%. MARD was 12.5%, with 77% of values within zone. 98% of sensors had clinically acceptable correlation.
Davis GM, Faulds E, Walker T, et al. Remote Continuous Glucose Monitoring With a Computerized Insulin Infusion Protocol for Critically Ill Patients in a COVID-19 Medical ICU: Proof of Concept. Diabetes Care. 2021;44:1055–8.
Wollersheim T, Engelhardt LJ, Pachulla J, et al. Accuracy, reliability, feasibility and nurse acceptance of a subcutaneous continuous glucose management system in critically ill patients: a prospective clinical trial. Ann Intensive Care. 2016;6:70.
Leopold JH, van Hooijdonk RTM, Boshuizen M, et al. Point and trend accuracy of a continuous intravenous microdialysis-based glucose-monitoring device in critically ill patients: a prospective study. Ann Intensive Care. 2016;6:68.
Song IK, Lee JH, Kang JE, Park YH, Kim HS, Kim JT. Continuous glucose monitoring system in the operating room and intensive care unit: any difference according to measurement sites? J Clin Monit Comput. 2017;31:187–94.
Faulds ER, Jones L, McNett M, et al. Facilitators and Barriers to Nursing Implementation of Continuous Glucose Monitoring (CGM) in Critically Ill Patients With COVID-19. Endocr Pract. 2021;27:354–61.
Lu MZ, Zuo YY, Guo J, Wen XP, Kang Y. 2018 Continuous glucose monitoring system can improve the quality of glucose control and glucose variability compared with point-of-care measurement in critically ill patients A randomized controlled trial Medicine 97
Preiser JC, Lheureux O, Thooft A, Brimioulle S, Goldstein J, Vincent JL. Near-Continuous Glucose Monitoring Makes Glycemic Control Safer in ICU Patients. Crit Care Med. 2018;46:1224–9.
Agus MSD, Wypij D, Hirshberg EL, et al. Tight Glycemic Control in Critically Ill Children. N Engl J Med. 2017;376:729–41.
Song IK, Lee JH, Kang JE, Park YH, Kim HS, Kim JT. Continuous glucose monitoring system in the operating room and intensive care unit: any difference according to measurement sites? J Clin Monit Comput. 2017;31:187–94.
Rijkenberg S, van Steen SC, DeVries JH, van der Voort PHJ. Accuracy and reliability of a subcutaneous continuous glucose monitoring device in critically ill patients. J Clin Monit Comput. 2018;32:953–64.
Gomez AM, Henao DC, Munoz OM, et al. Glycemic control metrics using flash glucose monitoring and hospital complications in patients with COVID-19. Diabetes & Metabolic Syndrome-Clinical Research & Reviews. 2021;15:499–503.
ElSayed, N. A., et al. 2023 "16 Diabetes Care in the Hospital Standards of Care in Diabetes-2023 Diabetes Care 46 Supplement_1 S267-S278
Rabiee A, Magruder JT, Grant C, et al. Accuracy and reliability of the Nova StatStrip(R) glucose meter for real-time blood glucose determinations during glucose clamp studies. J Diabetes Sci Technol. 2010;4:1195–201.
Preiser JC, Chase JG, Hovorka R, et al. Glucose Control in the ICU: A Continuing Story. J Diabetes Sci Technol. 2016;10:1372–81.
Fortmann AL, Bagsic SSR, Talavera L, et al. Glucose as the Fifth Vital Sign: A Randomized Controlled Trial of Continuous Glucose Monitoring in a Non-ICU Hospital Setting. Diabetes Care. 2020;43:2873–7.
Wadwa RP, Laffel LM, Shah VN, Garg SK. Accuracy of a Factory-Calibrated, Real-Time Continuous Glucose Monitoring System During 10 Days of Use in Youth and Adults with Diabetes. Diabetes Technol Ther. 2018;20:395–402.
Boom DT, Sechterberger MK, Rijkenberg S, et al. Insulin treatment guided by subcutaneous continuous glucose monitoring compared to frequent point-of-care measurement in critically ill patients: a randomized controlled trial. Crit Care. 2014;18:453.
Lengnick-Hall R, Gerke DR, Proctor EK, et al. Six practical recommendations for improved implementation outcomes reporting. Implement Sci. 2022;17:16.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50:217–26.
Grimshaw JM, Thomas RE, MacLennan G, et al. 2004 Effectiveness and efficiency of guideline dissemination and implementation strategies Health Technol Assess 8 iii-iv 1–72
Author information
Authors and Affiliations
Contributions
ERF, KMD, and MM designed the scoping review protocol. ERF extracted manuscripts from included databases. ERF and MM reviewed titles and abstracts and later full text articles. KMD resolved any discrepancies. ERF and MM extracted data from included studies. ERF, KMD, and MM crafted the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Eileen R Faulds received consultation from Dexcom, and speaker fees from Medscape and Dexcom. Molly McNett, Eileen R. Faulds, and Kathleen M. Dungan have received research funding from Dexcom LLC. K.D. has declared research support from Sanofi, Viacyte, Abbott, and Dexcom, consulting activities with Eli Lilly, Boehringer Ingelheim, Elsevier, Dexcom, honoraria from UptoDate, Medscape, Academy for Continued Healthcare Learning, Cardiometabolic Health Congress.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Faulds, E.R., Dungan, K.M. & McNett, M. Implementation of Continuous Glucose Monitoring in Critical Care: A Scoping Review. Curr Diab Rep 23, 69–87 (2023). https://doi.org/10.1007/s11892-023-01503-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-023-01503-5