Abstract
Purpose of Review
Transcatheter aortic valve replacement (TAVR) has changed the paradigm for management of severe aortic stenosis. Despite evolution of TAVR over the past 2 decades, conduction system disturbances remain a concern post-TAVR. In this review, we describe (1) permanent pacemaker (PP) implant rates associated with TAVR, (2) risk factors predicting need for PP therapy post-TAVR, (3) management of perioperative conduction abnormalities, and (4) novel areas of research.
Recent Findings
Conduction disturbances remain a common issue post-TAVR, in particular, left bundle branch block (LBBB). Though newer data describes resolution of a significant fraction of these disturbances over time, rates of pacemaker therapy remain high despite improvements in valve technology and procedural technique.
Summary
Recent consensus statements and guideline documents are important first steps in standardizing an approach to post-TAVR conduction disturbances. New areas of research show promise in both prediction and treatment of conduction disturbances post-TAVR.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Popma JJ, Adams DH, Reardon MJ, et al. Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol. 2014;63:1972–81.
Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187–98.
Leon MB, Smith CR, Mack MJ, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374:1609–20.
Mori M, Bin Mahmood SU, Geirsson A, et al. Trends in volume and risk profiles of patients undergoing isolated surgical and transcatheter aortic valve replacement. Catheter Cardiovasc Interv. 2019;93:E337–E42.
Mack MJ, Leon MB, Thourani VH, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380:1695–705.
Weber M, Sinning JM, Hammerstingl C, Werner N, Grube E, Nickenig G. Permanent pacemaker implantation after TAVR - predictors and impact on outcomes. Interv Cardiol. 2015;10:98–102.
Russo E, Potenza DR, Casella M, et al. Rate and predictors of permanent pacemaker implantation after transcatheter aortic valve implantation: current status. Curr Cardiol Rev. 2019;15:205–18.
Abdel-Wahab M, Mehilli J, Frerker C, et al. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcatheter aortic valve replacement: the CHOICE randomized clinical trial. JAMA. 2014;311:1503–14.
Maan A, Refaat MM, Heist EK, et al. Incidence and predictors of pacemaker implantation in patients undergoing transcatheter aortic valve replacement. Pacing Clin Electrophysiol. 2015;38:878–86.
Lefevre T, Kappetein AP, Wolner E, et al. One year follow-up of the multi-centre European PARTNER transcatheter heart valve study. Eur Heart J. 2011;32:148–57.
Thiele H, Kurz T, Feistritzer HJ, et al. Comparison of newer generation self-expandable vs. balloon-expandable valves in transcatheter aortic valve implantation: the randomized SOLVE-TAVI trial. Eur Heart J. 2020;41:1890–9.
Deharo P, Bisson A, Herbert J, et al. Impact of Sapien 3 balloon-expandable versus Evolut R self-expandable transcatheter aortic valve implantation in patients with aortic stenosis: data from a nationwide analysis. Circulation. 2020;141:260–8.
Grover FL, Vemulapalli S, Carroll JD, et al. 2016 Annual Report of The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol. 2017;69:1215–30.
Kodali SK, Williams MR, Smith CR, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med. 2012;366:1686–95.
Kawashima T, Sato F. Visualizing anatomical evidences on atrioventricular conduction system for TAVI. Int J Cardiol. 2014;174:1–6.
Sinhal A, Altwegg L, Pasupati S, et al. Atrioventricular block after transcatheter balloon expandable aortic valve implantation. JACC Cardiovasc Interv. 2008;1:305–9.
Moreno R, Dobarro D, Lopez de Sa E, et al. Cause of complete atrioventricular block after percutaneous aortic valve implantation: insights from a necropsy study. Circulation. 2009;120:e29–30.
Nazif TM, Dizon JM, Hahn RT, et al. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: the PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc Interv. 2015;8:60–9.
Toggweiler S, Kobza R. Pacemaker implantation after transcatheter aortic valve: why is this still happening? J Thorac Dis. 2018;10:S3614–S9.
Bob-Manuel T, Nanda A, Latham S, Pour-Ghaz I, Skelton WP, Khouzam RN. Permanent pacemaker insertion in patients with conduction abnormalities post transcatheter aortic valve replacement: a review and proposed guidelines. Ann Transl Med. 2018;6:11.
Maeno Y, Abramowitz Y, Kawamori H, et al. A highly predictive risk model for pacemaker implantation after TAVR. JACC Cardiovasc Imaging. 2017;10:1139–47.
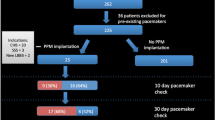
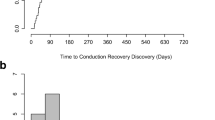
Ream K, Sandhu A, Valle J, et al. Ambulatory rhythm monitoring to detect late high-grade atrioventricular block following transcatheter aortic valve replacement. J Am Coll Cardiol. 2019;73:2538–47.
Lenders GD, Collas V, Hernandez JM, et al. Depth of valve implantation, conduction disturbances and pacemaker implantation with CoreValve and CoreValve Accutrak system for Transcatheter Aortic Valve Implantation, a multi-center study. Int J Cardiol. 2014;176:771–5.
Khawaja MZ, Rajani R, Cook A, et al. Permanent pacemaker insertion after CoreValve transcatheter aortic valve implantation: incidence and contributing factors (the UK CoreValve Collaborative). Circulation. 2011;123:951–60.
Barbanti M. Increased pacemaker implantation rate after new-generation balloon-expandable SAPIEN 3 valve: who was to blame, the valve or the doctor? JACC Cardiovasc Interv. 2016;9:814–6.
van Rosendael PJ, Delgado V, Bax JJ. Pacemaker implantation rate after transcatheter aortic valve implantation with early and new-generation devices: a systematic review. Eur Heart J. 2018;39:2003–13.
Sandhu A, Tzou W, Ream K, et al. Heart block after discharge in patients undergoing TAVR with latest-generation valves. J Am Coll Cardiol. 2018;71:577–8.
Petronio AS, Sinning JM, Van Mieghem N, et al. Optimal implantation depth and adherence to guidelines on permanent pacing to improve the results of transcatheter aortic valve replacement with the Medtronic CoreValve System: the CoreValve prospective, International, Post-Market ADVANCE-II Study. JACC Cardiovasc Interv. 2015;8:837–46.
Schroeter T, Linke A, Haensig M, et al. Predictors of permanent pacemaker implantation after Medtronic CoreValve bioprosthesis implantation. Europace. 2012;14:1759–63.
Lange P, Greif M, Vogel A, et al. Reduction of pacemaker implantation rates after CoreValve(R) implantation by moderate predilatation. EuroIntervention. 2014;9:1151–7.
Pibarot P, Hahn RT, Weissman NJ, et al. Association of paravalvular regurgitation with 1-year outcomes after transcatheter aortic valve replacement with the SAPIEN 3 valve. JAMA Cardiol. 2017;2:1208–16.
De Torres-Alba F, Kaleschke G, Diller GP, et al. Changes in the pacemaker rate after transition from Edwards SAPIEN XT to SAPIEN 3 transcatheter aortic valve implantation: the critical role of valve implantation height. JACC Cardiovasc Interv. 2016;9:805–13.
van der Boon RM, Nuis RJ, Van Mieghem NM, et al. New conduction abnormalities after TAVI--frequency and causes. Nat Rev Cardiol. 2012;9:454–63.
Bax JJ, Delgado V, Bapat V, et al. Open issues in transcatheter aortic valve implantation. Part 2: procedural issues and outcomes after transcatheter aortic valve implantation. Eur Heart J. 2014;35:2639–54.
Chamandi C, Barbanti M, Munoz-Garcia A, et al. Long-term outcomes in patients with new-onset persistent left bundle branch block following TAVR. JACC Cardiovasc Interv. 2019;12:1175–84.
Houthuizen P, van der Boon RM, Urena M, et al. Occurrence, fate and consequences of ventricular conduction abnormalities after transcatheter aortic valve implantation. EuroIntervention. 2014;9:1142–50.
Nazif TM, Williams MR, Hahn RT, et al. Clinical implications of new-onset left bundle branch block after transcatheter aortic valve replacement: analysis of the PARTNER experience. Eur Heart J. 2014;35:1599–607.
Urena M, Mok M, Serra V, et al. Predictive factors and long-term clinical consequences of persistent left bundle branch block following transcatheter aortic valve implantation with a balloon-expandable valve. J Am Coll Cardiol. 2012;60:1743–52.
Testa L, Latib A, De Marco F, et al. Clinical impact of persistent left bundle-branch block after transcatheter aortic valve implantation with CoreValve Revalving System. Circulation. 2013;127:1300–7.
Schymik G, Tzamalis P, Bramlage P, et al. Clinical impact of a new left bundle branch block following TAVI implantation: 1-year results of the TAVIK cohort. Clin Res Cardiol. 2015;104:351–62.
Franzoni I, Latib A, Maisano F, et al. Comparison of incidence and predictors of left bundle branch block after transcatheter aortic valve implantation using the CoreValve versus the Edwards valve. Am J Cardiol. 2013;112:554–9.
• Auffret V, Puri R, Urena M, et al. Conduction disturbances after transcatheter aortic valve replacement: current status and future perspectives. Circulation. 2017;136:1049–69 This work is a high-quality review of conduction system disturbances and risk factors associated with need for permanent pacemaker therapy post-TAVR.
• Rodes-Cabau J, Ellenbogen KA, Krahn AD, et al. Management of conduction disturbances associated with transcatheter aortic valve replacement: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;74:1086–106 This document outlines strategies for the management of conduction disturbances post-TAVR. It puts forth an organized method to approach such disturbances.
Bavaria JE, Tommaso CL, Brindis RG, et al. 2018 AATS/ACC/SCAI/STS expert consensus systems of care document: operator and institutional recommendations and requirements for transcatheter aortic valve replacement: a joint report of the American Association for Thoracic Surgery, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2019;73:340–74.
Meduri CU, Kereiakes DJ, Rajagopal V, et al. Pacemaker implantation and dependency after transcatheter aortic valve replacement in the REPRISE III Trial. J Am Heart Assoc. 2019;e012594:8.
Sandhu A, Aleong RG, Ream K, et al. Abstract 16381: Pacing burden in those undergoing permanent pacemaker implantation after Tavr with latest generation valves. Circulation. 2019;140:A16381-A.
Fry E, Fan J, Davis A, et al. Abstract 11330: High and low pacing burden associations for pacemakers implanted post Tavr. Circulation. 2019;140:A11330-A.
Nazif T, Sanchez C, Whisenant B, et al. Analysis of the initial united states experience with the biotrace tempo temporary pacing lead in transcatheter aortic valve replacement (TAVR) and other cardiac procedures. J Am Coll Cardiol. 2018;71:A1285.
Vijayaraman P, Cano O, Koruth JS, et al. His-Purkinje conduction system pacing following transcatheter aortic valve replacement: feasibility and safety. JACC Clin Electrophysiol. 2020;6:649–57.
Kiani S, Kamioka N, Black GB, et al. Development of a risk score to predict new pacemaker implantation after transcatheter aortic valve replacement. J Am Coll Cardiol Intv. 2019;12:2133–42.
Krishnaswamy A, Sammour Y, Mangieri A, et al. The utility of rapid atrial pacing immediately post-TAVR to predict the need for pacemaker implantation. J Am Coll Cardiol Intv. 2020;13:1046–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Sandhu has nothing to disclose. Dr. Tzou reports personal fees from Medtronic, Boston Scientific, and Biotronik, and grants and personal fees from Abbott.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Sandhu, A., Tzou, W.S. A Disruptive Technology: Determining Need for Permanent Pacing After TAVR. Curr Cardiol Rep 23, 53 (2021). https://doi.org/10.1007/s11886-021-01481-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-021-01481-8